Abstract
Purpose of Review
This review article discusses the updated World Health Classification of chondrogenic skeletal tumors and the role of conventional and advanced magnetic resonance (MR) imaging in the evaluation of chondrogenic skeletal lesions with emphasis on select diagnostic dilemmas.
Recent Findings
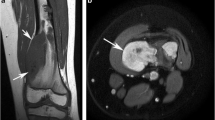
The majority of benign chondrogenic skeletal lesions have typical radiographic and MR features. Conventional MR imaging sequences can be helpful in the distinction of tumor-like lesions from chondrogenic tumors, and the evaluation of anatomic extent, particularly with regard to the detection of soft tissue masses associated with a chondrosarcoma (CS). Benign, atypical, and malignant chondrogenic lesions can have overlapping features on diffusion-weighted imaging (DWI) with apparent diffusion coefficient (ADC) mapping although dynamic contrast-enhanced (DCE) sequences can be helpful in the characterization of chondrogenic tumors as benign or malignant. Patients with multiple chondrogenic tumor conditions or syndromes are predisposed to developing CS and extra-skeletal malignancies, and as such, a small subset may benefit from imaging surveillance.
Summary
The majority of chondrogenic skeletal lesions can be characterized confidently on imaging. In the small subset of intermediate and malignant chondrogenic lesions with overlapping imaging and pathological features, a multidisciplinary approach should be used.













Similar content being viewed by others
References
Recently published papers of particular interest have been highlighted as: •• Of major importance
Fletcher C, Bridge J, Hogendoorn P. WHO classification of tumours of soft tissue and bone. In: Pathology and genetics of tumours of soft tissue and bone. Lyon (France): IARC Press; 2013.
Golden T, Siordia JA. Osteochondromyxoma: review of a rare carney complex criterion. J Bone Oncol. 2016;5(4):194–7.
Hong ED, Carrino JA, Weber KL, Fayad LM. Prevalence of shoulder enchondromas on routine MR imaging. Clin Imaging. 2011;35(5):378–84.
Walden MJ, Murphey MD, Vidal JA. Incidental enchondromas of the knee. AJR Am J Roentgenol. 2008;190:1611–5.
Forest M, Amouroux J. Pathology of pseudotumoral lesions. In: Forest M, Tomeno B, Vanel D, editors. Orthopedic surgical pathology: diagnosis of tumors and pseudotumoral lesions of bone and joints. Edinburgh: Churchill Livingstone; 1997. p. 519–670.
Woertler K. Benign bone tumours and tumour-like lesions: value of cross-sectional imaging. Eur Radiol. 2003;13:1820–35.
De Beuckeleer LHL, De Schepper AMA, Ramon F. Magnetic resonance imaging of cartilaginous tumours: is it useful or necessary? Skelet Radiol. 1996;25:137–41.
Flemming DJ, Murphey MD. Enchondroma and chondrosarcoma. Semin Musculoskelet Radiol. 2000;4(1):59–71.
Propeck T, Bullard MA, Lin J, Doi K, Martel W. Radiologic–pathologic correlation of intraosseous lipomas. AJR. 2000;175:673–8.
Gholamrezanezhad A, Basques K, Kosmas C. Peering beneath the surface: juxtacortical tumors of bone (part I). Clin Imaging. 2018;27(51):1–11.
Lewis MM, Kenan S, Yabut SM, Norman A, Steiner G. Periosteal chondroma. A report of ten cases and review of the literature. Clin Orthop Relat Res. 1990;256:185–92.
Kenan S, Abdelwahab IF, Klein MJ, Hermann G, Lewis MM. Lesions of juxtacortical origin (surface lesions of bone). Skelet Radiol. 1993;22:337–57.
Wu CT, Inwards CY, O’Laughlin S, Rock MG, Beabout JW, Unni KK. Chondromyxoid fibroma of bone: a clinicopathologic review of 278 cases. Hum Pathol. 1998;29(5):438–46.
Maheshwari AV, Jelinek JS, Song AJ, Nelson KJ, Murphey MD, Henshaw RM. Metaphyseal and diaphyseal chondroblastomas. Skelet Radiol. 2011;40(12):1563–73.
Murphey MD, Flemming DJ, Boyea SR, et al. From the archives of the AFIP. Enchondroma versus chondrosarcoma in the appendicular skeleton: differentiating features. Radiographics. 1998;18:1213–37.
Geirnaerdt MJ, Bloem JL, Eulderink F, Hogendoorn PC, Taminiau AH. Cartilaginous tumours: correlation of gadolinium-enhanced MR imaging and histopathologic findings. Radiology. 1993;186:813–7.
Murphey MD, Walker EA, Wilson AJ, Kransdorf MJ, Temple HT, Gannon FH. From the archives of the AFIP: imaging of primary chondrosarcoma: radiologic–pathologic correlation. Radiographics. 2003;23(5):1245–78.
•• Bernard SA, Murphey MD, Flemming DJ, Kransdorf MJ. Improved differentiation of benign osteochondromas from secondary oseochondromas with standardized measurement of cartilage cap at CT and MR imaging. Radiology 2010; 255:857–867. Cartilage cap thickness of 2 cm or greater on CT or MRI is a useful anatomic feature for the characterization of a chondrogenic lesions as CS rather than osteochondroma with sensitivities and specificities of 100% and 98% for MR imaging and 100 and 95% for CT, respectively.
Geirnaerdt MJ, Hermans J, Bloem JL, et al. Usefulness of radiography in differentiating enchondroma from central grade I chondrosarcoma. AJR Am J Roentgenol. 1997;169:1097–104.
Del Grande F, Ahlawat S, Subhangwong T, Fayad LM. Characterization of indeterminate soft tissue masses referred for biopsy: what is the added value of contrast imaging at 3.0 tesla? J Magn Reson Imaging. 2017;45(2):390–400.
Pekcevik Y, Kahya MO, Kaya A. Diffusion-weighted magnetic resonance imaging in the diagnosis of bone tumors: preliminary Results. J Clin Imaging Sci. 2013;31(3):63.
Hayashida Y, Hirai T, Yakushiji T, Katahira K, Shimomura O, Imuta M, et al. Evaluation of diffusion-weighted imaging for the differential diagnosis of poorly contrast-enhanced and T2-prolonged bone masses: initial experience. J Magn Reson Imaging. 2006;23:377–82.
Nagata S, Nishimura H, Uchida M, Hayabuchi N. Usefulness of diffusion-weighted MRI in differentiating benign from malignant musculoskeletal tumors. Nihon Igaku Hoshasen Gakkai Zasshi. 2005;65:30–6.
Douis H, Jeys L, Grimer R, Vaiyapuri S, Davies AM. Is there a role for diffusion-weighted MRI (DWI) in the diagnosis of central cartilage tumors? Skelet Radiol. 2015;44(7):963–9.
Douis H, Davies MA, Sian P. The role of diffusion-weighted MRI (DWI) in the differentiation of benign from malignant skeletal lesions of the pelvis. Eur J Radiol. 2016;85(12):2262–8.
Ahlawat S, Khandheria P, Subhawong TK, Fayad LM. Differentiation of benign and malignant skeletal lesions with quantitative diffusion weighted MRI at 3T. Eur J Radiol. 2015;84(6):1091–7.
•• De Coninck T, Jans L, Sys G, Huysse W, Verstraeten T, Forsyth R, Poffyn B, Verstraete K. Dynamic contrast-enhanced MR imaging for differentiation between enchondroma and chondrosarcoma. Eur Radiol. 2013;23(11):3140–52. Dynamic contrast enhanced MR sequences can be complementary to routine anatomic MR sequences for the characterization of chondrogenic skeletal lesions as benign or malignant.
Verstraete KL, De Deene Y, Roels H, Dierick A, Uyttendaele D, Kunnen M. Benign and malignant musculoskeletal lesions: dynamic contrast-enhanced MR imaging-parametric “first-pass” images depict tissue vascularisation and perfusion. Radiology. 1994;192:835–43.
Geirnaerdt MJ, Hogendoorn PC, Bloem JL, Taminiau AH, van der Woude HJ. Cartilaginous tumours: fast contrast-enhanced MR imaging. Radiology. 2000;214:539–46.
Sujlana P, Skrok J, Fayad LM. Review of dynamic contrast-enhanced MRI: technical aspects and applications in the musculoskeletal system. J Magn Reson Imaging. 2018;47(4):875–90.
•• Skeletal Lesions Interobserver Correlation among Expert Diagnosticians (SLICED) Study Group. Reliability of histopathologic and radiologic grading of cartilaginous neoplasms in long bones. J Bone Joint Surg Am. 2007;89:2113–23. This study demonstrates the low reliability of both radiologists and pathologists for the characterization of chondrogenic skeletal lesions in long bones as benign or malignant and when malignant as low or high grade malignances.
Schwartz HS, Zimmerman NB, Simon MA, Wroble RR, Millar EA, Bonfiglio M. The malignant potential of enchondromatosis. J Bone Joint Surg Am. 1987;69(2):269–74.
•• Verdegaal SH, Bovée JV, Pansuriya TC, Grimer RJ, Ozger H, Jutte PC, San Julian M, Biau DJ, van der Geest IC, Leithner A, Streitbürger A, Klenke FM, Gouin FG, Campanacci DA, Marec-Berard P, Hogendoorn PC, Brand R, Taminiau AH. Incidence, predictive factors, and prognosis of chondrosarcoma in patients with Ollier disease and Maffucci syndrome: an international multicenter study of 161 patients. Oncologist. 2011;16(12):1771–9. Patients with Ollier disease and Maffucci syndrome presenting with enchondromas located in long bones or axial skeleton, especially the pelvis, have an increased risk of developing secondary chondrosarcoma, and are identified as the population that needs regular screening on early detection of malignant transformation.
Ahlawat S, Fayad LM, Khan MS, Bredella MA, Harris GJ, Evans DG, Farschtschi S, Jacobs MA, Chhabra A, Salamon JM, Wenzel R, Mautner VF, Dombi E, Cai W, Plotkin SR, Blakeley JO; Whole Body MRI Committee for the REiNS International Collaboration; REiNS International Collaboration Members 2016. Current whole-body MRI applications in the neurofibromatoses: NF1, NF2, and schwannomatosis. Neurology. 2016;87(7 Suppl 1):S31–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Shivani Ahlawat declares no potential conflicts of interest. Laura M. Fayad reports Gant support: GERRAF 2008-10, Siemens 2011-12.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical collection on Musculoskeletal Imaging.
Rights and permissions
About this article
Cite this article
Ahlawat, S., Fayad, L.M. MR Imaging of Chondrogenic Tumors: Update on Select Imaging Challenges. Curr Radiol Rep 6, 24 (2018). https://doi.org/10.1007/s40134-018-0284-6
Published:
DOI: https://doi.org/10.1007/s40134-018-0284-6