Abstract
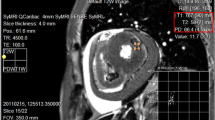
Myocardial infarct (MI) size has been increasingly used as an endpoint in multiple clinical trials and has thus become an important clinical measure. While late gadolinium enhancement MRI is considered the clinical reference standard to detect, characterize, and quantify MI, there is no established universal quantification algorithm that provides reliable MI assessment in every scenario. Efforts have been made to improve the binary threshold-based methods which dichotomize MRI voxels as either healthy or infarcted. Novel algorithms have also been proposed to quantify the actual infarcted tissue content of each MRI voxel while accounting for partial volume averaging, a common issue in quantitative MRI. Currently, the full-width at half-maximum binary algorithm seems to have the highest accuracy and reproducibility. Non-binary algorithms show comparable results; however, the literature is limited in terms of their clinical feasibility.



Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kali A, Choi EY, Sharif B, et al. Native T1 mapping by 3-T CMR imaging for characterization of chronic myocardial infarctions. JACC Cardiovasc Imaging. 2015;8(9):1019–30.
Suranyi P, Kiss P, Brott BC, et al. Percent infarct mapping: an R1-map-based CE-MRI method for determining myocardial viability distribution. Magn Reson Med. 2006;56(3):535–45.
Hwang SH, Choi EY, Park CH, et al. Evaluation of extracellular volume fraction thresholds corresponding to myocardial late-gadolinium enhancement using cardiac magnetic resonance. Int J Cardiovasc Imaging. 2014;30(Suppl 2):137–44.
Farrelly C, Rehwald W, Salerno M, et al. Improved detection of subendocardial hyperenhancement in myocardial infarction using dark blood-pool delayed enhancement MRI. Am J Roentgenol. 2011;196(2):339–48.
Kim HW, Rehwald WG, Wendell DC, et al. Black-blood contrast-enhanced MRI: validation of a novel technique for the diagnosis of myocardial infarction. Proc Intl Soc Mag Reson Med. 2015;23:662.
Varga-Szemes A, Muscogiuri G, Rehwald W, et al. Accuracy of a prototype dark blood late gadolinium enhancement technique for the detection and quantification of myocardial infarction. J Cardiovasc Magn Reson. 2016;18(Suppl 1):Q65.
Kim RJ, Chen EL, Lima JA, et al. Myocardial Gd-DTPA kinetics determine MRI contrast enhancement and reflect the extent and severity of myocardial injury after acute reperfused infarction. Circulation. 1996;94(12):3318–26.
Cerqueira MD, Weissman NJ, Dilsizian V, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation. 2002;105(4):539–42.
Schuijf JD, Kaandorp TA, Lamb HJ, et al. Quantification of myocardial infarct size and transmurality by contrast-enhanced magnetic resonance imaging in men. Am J Cardiol. 2004;94(3):284–8.
Sievers B, Elliott MD, Hurwitz LM, et al. Rapid detection of myocardial infarction by subsecond, free-breathing delayed contrast-enhancement cardiovascular magnetic resonance. Circulation. 2007;115(2):236–44.
Funada A, Kanzaki H, Noguchi T, et al. Prognostic significance of late gadolinium enhancement quantification in cardiac magnetic resonance imaging of hypertrophic cardiomyopathy with systolic dysfunction. Heart Vessels. 2015. doi:10.1007/s00380-015-0670-4.
Kwon DH, Asamoto L, Popovic ZB, et al. Infarct characterization and quantification by delayed enhancement cardiac magnetic resonance imaging is a powerful independent and incremental predictor of mortality in patients with advanced ischemic cardiomyopathy. Circ Cardiovasc Imaging. 2014;7(5):796–804.
Karim R, Housden RJ, Balasubramaniam M, et al. Evaluation of current algorithms for segmentation of scar tissue from late gadolinium enhancement cardiovascular magnetic resonance of the left atrium: an open-access grand challenge. J Cardiovasc Magn Reson. 2013;15:105.
•• McAlindon E, Pufulete M, Lawton C, et al. Quantification of infarct size and myocardium at risk: evaluation of different techniques and its implications. Eur Heart J Cardiovasc Imaging. 2015;16(7):738–46. Valuable comparison of the current binary infarct quantification techniques also including manual segmentation.
Burns RJ, Gibbons RJ, Yi Q, et al. The relationships of left ventricular ejection fraction, end-systolic volume index and infarct size to six-month mortality after hospital discharge following myocardial infarction treated by thrombolysis. J Am Coll Cardiol. 2002;39(1):30–6.
Beek AM, Bondarenko O, Afsharzada F, et al. Quantification of late gadolinium enhanced CMR in viability assessment in chronic ischemic heart disease: a comparison to functional outcome. J Cardiovasc Magn Reson. 2009;11:6.
Baks T, van Geuns RJ, Biagini E, et al. Recovery of left ventricular function after primary angioplasty for acute myocardial infarction. Eur Heart J. 2005;26(11):1070–7.
Scott PA, Morgan JM, Carroll N, et al. The extent of left ventricular scar quantified by late gadolinium enhancement MRI is associated with spontaneous ventricular arrhythmias in patients with coronary artery disease and implantable cardioverter-defibrillators. Circ Arrhythm Electrophysiol. 2011;4(3):324–30.
Fishbein M, Meerbaum S, Rit J, et al. Early phase acute myocardial infarct size quantification: validation of the triphenyl tetrazolium chloride tissue enzyme staining technique. Am Heart J. 1981;101(5):593–600.
Schmidt A, Azevedo CF, Cheng A, et al. Infarct tissue heterogeneity by magnetic resonance imaging identifies enhanced cardiac arrhythmia susceptibility in patients with left ventricular dysfunction. Circulation. 2007;115(15):2006–14.
Yan AT, Shayne AJ, Brown KA, et al. Characterization of the peri-infarct zone by contrast-enhanced cardiac magnetic resonance imaging is a powerful predictor of post-myocardial infarction mortality. Circulation. 2006;114(1):32–9.
Schuleri KH, Centola M, George RT, et al. Characterization of peri-infarct zone heterogeneity by contrast-enhanced multidetector computed tomography: a comparison with magnetic resonance imaging. J Am Coll Cardiol. 2009;53(18):1699–707.
Schelbert EB, Hsu LY, Anderson SA, et al. Late gadolinium-enhancement cardiac magnetic resonance identifies postinfarction myocardial fibrosis and the border zone at the near cellular level in ex vivo rat heart. Circ Cardiovasc Imaging. 2010;3(6):743–52.
Varga-Szemes A, Simor T, Lenkey Z, et al. Infarct density distribution by MRI in the porcine model of acute and chronic myocardial infarction as a potential method transferable to the clinic. Int J Cardiovasc Imaging. 2014;30(5):937–48.
Kim RJ, Fieno DS, Parrish TB, et al. Relationship of MRI delayed contrast enhancement to irreversible injury, infarct age, and contractile function. Circulation. 1999;100(19):1992–2002.
Gerber BL, Garot J, Bluemke DA, et al. Accuracy of contrast-enhanced magnetic resonance imaging in predicting improvement of regional myocardial function in patients after acute myocardial infarction. Circulation. 2002;106(9):1083–9.
Mewton N, Revel D, Bonnefoy E, et al. Comparison of visual scoring and quantitative planimetry methods for estimation of global infarct size on delayed enhanced cardiac MRI and validation with myocardial enzymes. Eur J Radiol. 2011;78(1):87–92.
Bondarenko O, Beek AM, Hofman MB, et al. Standardizing the definition of hyperenhancement in the quantitative assessment of infarct size and myocardial viability using delayed contrast-enhanced CMR. J Cardiovasc Magn Reson. 2005;7(2):481–5.
Fieno DS, Kim RJ, Chen EL, et al. Contrast-enhanced magnetic resonance imaging of myocardium at risk: distinction between reversible and irreversible injury throughout infarct healing. J Am Coll Cardiol. 2000;36(6):1985–91.
• Mesubi O, Ego-Osuala K, Jeudy J, et al. Differences in quantitative assessment of myocardial scar and gray zone by LGE-CMR imaging using established gray zone protocols. Int J Cardiovasc Imaging. 2015;31(2):359–68. This article investigates the segmentation of myocardial scar vs. gray zone using different binary algorithms.
Kim RJ, Wu E, Rafael A, et al. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med. 2000;343(20):1445–53.
Beek AM, Kuhl HP, Bondarenko O, et al. Delayed contrast-enhanced magnetic resonance imaging for the prediction of regional functional improvement after acute myocardial infarction. J Am Coll Cardiol. 2003;42(5):895–901.
Amado LC, Gerber BL, Gupta SN, et al. Accurate and objective infarct sizing by contrast-enhanced magnetic resonance imaging in a canine myocardial infarction model. J Am Coll Cardiol. 2004;44(12):2383–9.
Ibrahim T, Nekolla SG, Hornke M, et al. Quantitative measurement of infarct size by contrast-enhanced magnetic resonance imaging early after acute myocardial infarction: comparison with single-photon emission tomography using Tc99m-sestamibi. J Am Coll Cardiol. 2005;45(4):544–52.
Hsu L, Natanzon A, Kellman P, et al. Quantitative myocardial infarction on delayed enhancement MRI. Part I: animal validation of an automated feature analysis and combined thresholding infarct sizing algorithm. J Magn Reson Imaging. 2006;23(3):298–308.
Otsu N. A threshold selection method from gray-level histograms. IEEE Trans Syst Man Cyberb. 1979;9:62–6.
Vermes E, Childs H, Carbone I, et al. Auto-threshold quantification of late gadolinium enhancement in patients with acute heart disease. J Magn Reson Imaging. 2013;37(2):382–90.
Rajchl M, Stirrat J, Goubran M, et al. Comparison of semi-automated scar quantification techniques using high-resolution, 3-dimensional late-gadolinium-enhancement magnetic resonance imaging. Int J Cardiovasc Imaging. 2015;31(2):349–57.
Woie L, Maloy F, Eftestol T, et al. Comparing a novel automatic 3D method for LGE-CMR quantification of scar size with established methods. Int J Cardiovasc Imaging. 2014;30(2):339–47.
Baron N, Kachenoura N, Cluzel P, et al. Comparison of various methods for quantitative evaluation of myocardial infarct volume from magnetic resonance delayed enhancement data. Int J Cardiol. 2013;167(3):739–44.
•• Khan JN, Nazir SA, Horsfield MA, et al. Comparison of semi-automated methods to quantify infarct size and area at risk by cardiovascular magnetic resonance imaging at 1.5T and 3.0T field strengths. BMC Res Notes. 2015;8:52. Comparison of segmentation algorithms between 2D and 3D image datasets. The article covers basic thresholding aprooaches, the Otsu automated technique, as well as manual segmentation.
Flett AS, Hasleton J, Cook C, et al. Evaluation of techniques for the quantification of myocardial scar of differing etiology using cardiac magnetic resonance. JACC Cardiovasc Imaging. 2011;4(2):150–6.
Wagner A, Mahrholdt H, Thomson L, et al. Effects of time, dose, and inversion time for acute myocardial infarct size measurements based on magnetic resonance imaging-delayed contrast enhancement. J Am Coll Cardiol. 2006;47(10):2027–33.
Rajiah P, Desai MY, Kwon D, et al. MR imaging of myocardial infarction. Radiographics. 2013;33(5):1383–412.
Heiberg E, Ugander M, Engblom H, et al. Automated quantification of myocardial infarction from MR images by accounting for partial volume effects: animal, phantom, and human study. Radiology. 2008;246(2):581–8.
Simor T, Suranyi P, Ruzsics B, et al. Percent infarct mapping for delayed contrast enhancement magnetic resonance imaging to quantify myocardial viability by Gd(DTPA). J Magn Reson Imaging. 2010;32(4):859–68.
Kirschner R, Varga-Szemes A, Brott BC, et al. Quantification of myocardial viability distribution with Gd(DTPA) bolus-enhanced, signal intensity-based percent infarct mapping. Magn Reson Imaging. 2011;29(5):650–8.
• Lenkey Z, Varga-Szemes A, Simor T, et al. Age-independent myocardial infarct quantification by signal intensity percent infarct mapping in swine. J Magn Reson Imaging. 2015. doi:10.1002/jmri.25046. This article highlights that the non-binary percent infarct mapping technique can be used in all stages of myocardial infarction and reports inter- and intra-observer variablity for the non-binary and binary methods.
Nilsson B, Heyden A. A fast algorithm for level set-like active contours. Pattern Recognit Lett. 2003;24:1331–7.
Robbers LF, Eerenberg ES, Teunissen PF, et al. Magnetic resonance imaging-defined areas of microvascular obstruction after acute myocardial infarction represent microvascular destruction and haemorrhage. Eur Heart J. 2013;34(30):2346–53.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Akos Varga-Szemes reports personal fees from Guerbet. U. Joseph Schoepf reports grants from Siemens Healthcare, Bayer, Bracco, GE Healthcare, Medrad, and Astellas; personal fees from Siemens Healthcare and Guerbet; and non-financial support from Siemens Healthcare, Bayer, GE Healthcare, and Medrad. Dr. Schoepf is a section editor for Current Radiology Reports. Carlo N. De Cecco reports personal fees from Guerbet. Gabriel A. Elgavish is an Officer for Elgavish Paramagnetics Inc. Pal Suranyi reports non-financial support from Siemens Healthcare, Bayer, and GE Healthcare. Rob J van der Geest, Christian Tesche, and Stephen R. Fuller each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human subjects performed by any of the authors. Some figures in this manuscript were prepared using animal research data for which approval from institutional animal care committee was obtained.
Additional information
This article is part of the Topical Collection on New Imaging Technologies.
Rights and permissions
About this article
Cite this article
Varga-Szemes, A., van der Geest, R.J., Schoepf, U.J. et al. MRI Post-Processing Methods for Myocardial Infarct Quantification. Curr Radiol Rep 4, 30 (2016). https://doi.org/10.1007/s40134-016-0159-7
Published:
DOI: https://doi.org/10.1007/s40134-016-0159-7