Abstract
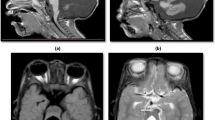
Cystic malformations within the posterior fossa are rather common findings in pediatric neuroimaging. They may be divided in two main groups based on their location and size: large extra-cerebellar and small intra-cerebellar cystic malformations. Both groups include various diseases: Dandy–Walker malformation, Blake’s pouch cyst, posterior fossa arachnoid cysts, and mega cisterna magna are extra-cerebellar posterior fossa cystic malformations, while α-dystroglycanopathies, GPR56-related fronto-parietal polymicrogyria, and Poretti–Boltshauser due to LAMA1 mutations are intra-cerebellar posterior fossa cystic malformations. These diseases may be differentiated based on the neuroimaging pattern. Differentiation between the various diseases associated with extra- and intra-cerebellar cystic malformations is important in terms of diagnosis, management, prognosis, and counseling of the affected families.








Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Boltshauser E. Cerebellum-small brain but large confusion: a review of selected cerebellar malformations and disruptions. Am J Med Genet A. 2004;126A(4):376–85.
Doherty D, Millen KJ, Barkovich AJ. Midbrain and hindbrain malformations: advances in clinical diagnosis, imaging, and genetics. Lancet Neurol. 2013;12(4):381–93.
Bosemani T, Orman G, Boltshauser E, Tekes A, Huisman TA, Poretti A. Congenital abnormalities of the posterior fossa. Radiographics. 2015;35(1):200–20.
Jissendi-Tchofo P, Severino M, Nguema-Edzang B, Toure C, Soto Ares G, Barkovich AJ. Update on neuroimaging phenotypes of mid-hindbrain malformations. Neuroradiology. 2015;57(2):113–38.
Patel S, Barkovich AJ. Analysis and classification of cerebellar malformations. AJNR Am J Neuroradiol. 2002;23(7):1074–87.
Tortori-Donati P, Fondelli MP, Rossi A, Carini S. Cystic malformations of the posterior cranial fossa originating from a defect of the posterior membranous area. Mega cisterna magna and persisting Blake’s pouch: two separate entities. Childs Nerv Syst. 1996;12(6):303–8.
Barth PG. Cerebellar dentate dysplasia. Brain Dev. 2011;33(8):621–6.
• Boltshauser E, Scheer I, Huisman TA, Poretti A. Cerebellar cysts in children: a pattern recognition approach. Cerebellum. 2015;14(3):308–16. Recent article reviewing various forms of intra-cerebellar cysts with different etiologies and pathomechanisms.
Liao C, Fu F, Li R, Yang X, Xu Q, Li D. Prenatal diagnosis and molecular characterization of a novel locus for Dandy–Walker malformation on chromosome 7p21.3q. Eur J Med Genet. 2012;55(8–9):472–5.
Grinberg I, Northrup H, Ardinger H, Prasad C, Dobyns WB, Millen KJ. Heterozygous deletion of the linked genes ZIC1 and ZIC4 is involved in Dandy–Walker malformation. Nat Genet. 2004;36(10):1053–5.
Aldinger KA, Lehmann OJ, Hudgins L, et al. FOXC1 is required for normal cerebellar development and is a major contributor to chromosome 6p25.3 Dandy-Walker malformation. Nat Genet. 2009;41(9):1037–42.
Zanni G, Barresi S, Travaglini L, et al. FGF17, a gene involved in cerebellar development, is downregulated in a patient with Dandy-Walker malformation carrying a de novo 8p deletion. Neurogenetics. 2011;12(3):241–5.
Darbro BW, Mahajan VB, Gakhar L, et al. Mutations in extracellular matrix genes NID1 and LAMC1 cause autosomal dominant Dandy-Walker malformation and occipital cephaloceles. Hum Mutat. 2013;34(8):1075–9.
• Barkovich AJ, Millen KJ, Dobyns WB. A developmental and genetic classification for midbrain-hindbrain malformations. Brain. 2009;132(Pt 12):3199–230. This article proposes a classification of mid-hindbrain malformations based upon embryology and genetics.
Limperopoulos C, Folkerth R, Barnewolt CE, Connolly S, Du Plessis AJ. Posthemorrhagic cerebellar disruption mimicking Dandy-Walker malformation: fetal imaging and neuropathology findings. Semin Pediatr Neurol. 2010;17(1):75–81.
Pichiecchio A, Decio A, Di Perri C, Parazzini C, Rossi A, Signorini S. “Acquired” Dandy-Walker malformation and cerebellar hemorrhage: usefulness of serial MRI. Eur J Paediatr Neurol. 2015;20:188–91.
Kumar R, Kumar Jain M, Kumar Chhabra D. Dandy-Walker syndrome: different modalities of treatment and outcome in 42 cases. Childs Nerv Syst. 2001;17(6):348–52.
Alexiou GA, Sfakianos G, Prodromou N. Dandy-Walker malformation: analysis of 19 cases. J Child Neurol. 2010;25(2):188–91.
Klein O, Pierre-Kahn A, Boddaert N, Parisot D, Brunelle F. Dandy-Walker malformation: prenatal diagnosis and prognosis. Childs Nerv Syst. 2003;19(7–8):484–9.
Boddaert N, Klein O, Ferguson N, et al. Intellectual prognosis of the Dandy-Walker malformation in children: the importance of vermian lobulation. Neuroradiology. 2003;45(5):320–4.
• Correa GG, Amaral LF, Vedolin LM. Neuroimaging of Dandy-Walker malformation: new concepts. Top Magn Reson Imaging. 2011;22(6):303–12. Recent review article on neuroimaging findings of extra-cerebellar posterior fossa cystic malformations.
Mohanty A, Biswas A, Satish S, Shankar Praharaj S, Sastry KV. Treatment options for Dandy-Walker malformation. J Neurosurg. 2006;105(5):348–56.
Parisi MA, Dobyns WB. Human malformations of the midbrain and hindbrain: review and proposal classification scheme. Mol Genet Metab. 2003;80(1–2):36–53.
Yildiz H, Yazici Z, Hakyemez B, Erdogan C, Parlak M. Evaluation of CSF flow patterns of posterior fossa cystic malformations using CSF flow MR imaging. Neuroradiology. 2006;48(9):595–605.
Limperopoulos C, Robertson RL, Khwaja OS, et al. How accurately does current fetal imaging identify posterior fossa anomalies? AJR Am J Roentgenol. 2008;190(6):1637–43.
Malinger G, Lev D, Lerman-Sagie T. The fetal cerebellum. Pitfalls in diagnosis and management. Prenat Diagn. 2009;29(4):372–80.
Adamsbaum C, Moutard ML, André C, et al. MRI of the fetal posterior fossa. Pediatr Radiol. 2005;35(2):124–40.
Poretti A, Boltshauser E, Doherty D. Cerebellar hypoplasia: differential diagnosis and diagnostic approach. Am J Med Genet C Semin Med Genet. 2014;166(2):211–26.
• Nelson MD, Jr., Maher K, Gilles FH. A different approach to cysts of the posterior fossa. Pediatr Radiol. 2004;34(9):720–32. Review article discussing neuroimaging and neuropathology features of extra-cerebellar posterior fossa cystic malformations.
Hirono S, Ito D, Murai H, et al. Postnatal development of Blake’s pouch cyst: a case report and new insight for its pathogenesis. Childs Nerv Syst. 2014;30(10):1767–71.
Cornips EM, Overvliet GM, Weber JW, et al. The clinical spectrum of Blake’s pouch cyst: report of six illustrative cases. Childs Nerv Syst. 2010;26(8):1057–64.
Calabro F, Arcuri T, Jinkins JR. Blake’s pouch cyst: an entity within the Dandy-Walker continuum. Neuroradiology. 2000;42(4):290–5.
Ali ZS, Lang SS, Bakar D, Storm PB, Stein SC. Pediatric intracranial arachnoid cysts: comparative effectiveness of surgical treatment options. Childs Nerv Syst. 2014;30(3):461–9.
Martinez-Lage JF, Perez-Espejo MA, Almagro MJ, Lopez-Guerrero AL. Hydrocephalus and arachnoid cysts. Childs Nerv Syst. 2011;27(10):1643–52.
Boltshauser E, Martin F, Altermatt S. Outcome in children with space-occupying posterior fossa arachnoid cysts. Neuropediatrics. 2002;33(3):118–21.
Marin-Sanabria EA, Yamamoto H, Nagashima T, Kohmura E. Evaluation of the management of arachnoid cyst of the posterior fossa in pediatric population: experience over 27 years. Childs Nerv Syst. 2007;23(5):535–42.
Shekdar K. Posterior fossa malformations. Semin Ultrasound CT MRI. 2011;32(3):228–41.
Altman NR, Naidich TP, Braffman BH. Posterior fossa malformations. AJNR Am J Neuroradiol. 1992;13(2):691–724.
Long A, Moran P, Robson S. Outcome of fetal cerebral posterior fossa anomalies. Prenat Diagn. 2006;26(8):707–10.
Forzano F, Mansour S, Ierullo A, Homfray T, Thilaganathan B. Posterior fossa malformation in fetuses: a report of 56 further cases and a review of the literature. Prenat Diagn. 2007;27(6):495–501.
Bolduc ME, Du Plessis AJ, Sullivan N, et al. Spectrum of neurodevelopmental disabilities in children with cerebellar malformations. Dev Med Child Neurol. 2011;53(5):409–16.
Bonnemann CG, Wang CH, Quijano-Roy S, et al. Diagnostic approach to the congenital muscular dystrophies. Neuromuscul Disord. 2014;24(4):289–311.
Moore SA, Saito F, Chen J, et al. Deletion of brain dystroglycan recapitulates aspects of congenital muscular dystrophy. Nature. 2002;418(6896):422–5.
Aida N, Yagishita A, Takada K, Katsumata Y. Cerebellar MR in Fukuyama congenital muscular dystrophy: polymicrogyria with cystic lesions. AJNR Am J Neuroradiol. 1994;15(9):1755–9.
Mercuri E, Muntoni F. The ever-expanding spectrum of congenital muscular dystrophies. Ann Neurol. 2012;72(1):9–17.
• Clement E, Mercuri E, Godfrey C, et al. Brain involvement in muscular dystrophies with defective dystroglycan glycosylation. Ann Neurol. 2008;64(5):573–82. Spectrum of neuroimaging findings in α-dystroglycanopathies and correlation between neuroimaging phenotype and genotype in 27 patients.
Amir T, Poretti A, Boltshauser E, Huisman TA. Differential diagnosis of ventriculomegaly and brainstem kinking on fetal MRI. Brain Dev. 2015;38:103–8.
• Bahi-Buisson N, Poirier K, Boddaert N, et al. GPR56-related bilateral frontoparietal polymicrogyria: further evidence for an overlap with the cobblestone complex. Brain. 2010;133(11):3194–209. Clinical and neuroimaging phenotype in 14 patients with GPR56 mutations.
Li S, Jin Z, Koirala S, et al. GPR56 regulates pial basement membrane integrity and cortical lamination. J Neurosci. 2008;28(22):5817–26.
Koirala S, Jin Z, Piao X, Corfas G. GPR56-regulated granule cell adhesion is essential for rostral cerebellar development. J Neurosci. 2009;29(23):7439–49.
Giera S, Deng Y, Luo R, et al. The adhesion G protein-coupled receptor GPR56 is a cell-autonomous regulator of oligodendrocyte development. Nat Commun. 2015;6(6):121.
• Poretti A, Hausler M, von Moers A, et al. Ataxia, intellectual disability, and ocular apraxia with cerebellar cysts: a new disease? Cerebellum. 2014;13(1):79–88. Clinical and neuroimaging phenotype in children with Poretti-Boltshauser syndrome.
• Aldinger KA, Mosca SJ, Tetreault M, et al. Mutations in LAMA1 cause cerebellar dysplasia and cysts with and without retinal dystrophy. Am J Hum Genet. 2014;95(2):227–34. First article reporting LAMA1 mutations in children with Poretti-Boltshauser syndrome.
Heng C, Lefebvre O, Klein A, et al. Functional role of laminin alpha1 chain during cerebellum development. Cell Adhes Migr. 2011;5(6):480–9.
Ichikawa-Tomikawa N, Ogawa J, Douet V, et al. Laminin alpha1 is essential for mouse cerebellar development. Matrix Biol. 2012;31(1):17–28.
Edwards MM, Mammadova-Bach E, Alpy F, et al. Mutations in Lama1 disrupt retinal vascular development and inner limiting membrane formation. J Biol Chem. 2010;285(10):7697–711.
Edwards MM, McLeod DS, Grebe R, Heng C, Lefebvre O, Lutty GA. Lama1 mutations lead to vitreoretinal blood vessel formation, persistence of fetal vasculature, and epiretinal membrane formation in mice. BMC Dev Biol. 2011;11:60.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Neuroimaging.
Rights and permissions
About this article
Cite this article
Poretti, A., Bosemani, T. Cystic Malformations Within the Posterior Fossa. Curr Radiol Rep 4, 17 (2016). https://doi.org/10.1007/s40134-016-0147-y
Published:
DOI: https://doi.org/10.1007/s40134-016-0147-y