Abstract
Purpose
In this review, we outline the guiding principles of safe and effective healthcare transition in adolescents and young adults (AYA) with kidney disease. We describe the inherent challenges associated with the process and review the available literature and resources that may support the healthcare team in achieving successful and safe transition.
Recent Findings
Safely guiding patients and families through the transition from pediatric to adult care is an important responsibility of the pediatric healthcare team. Growing evidence shows that lack of transition readiness increases morbidity and mortality in patients with chronic kidney disease and reduces allograft survival in transplanted AYA. Multidisciplinary efforts from multiple pediatric groups have developed evidence-based tools to holistically assess transition readiness and implement healthcare transition programs.
Summary
Increasing numbers of children with kidney disease are under the care of specialist pediatricians and pediatric nephrologists. Advancing diagnostics, medical management, and access to kidney replacement therapies—including both dialysis and transplantation—have steadily improved outcomes for these children. Thankfully, many are surviving childhood and adolescence and ultimately require transition to adult services. Without proper preparation for a successful healthcare transition, AYAs are at particularly high risk for poor health outcomes during this time. Growing evidence supports early, multi-disciplinary evaluation of patients and their families to inform the development of individualized transition programs which consider all aspects of this complex process. Herein, we compile the available evidence relating to best practice for healthcare transition and review available tools and strategies to promote better outcomes in this vulnerable AYA group.

Similar content being viewed by others
Data Availability
Not applicable.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
United States Renal Data System. 2022 USRDS Annual Data Report: epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2022.
Lewis MA, Shaw J, Sinha MD, Adalat S, Hussain F, Castledine C, et al. Chapter 14: Demography of the UK Paediatric Renal Replacement Therapy population in 2008. Nephron Clin Pract. 2010;115(1):c279–88.
Dobbels F, Van Damme-Lombaert R, Vanhaecke J, De Geest S. Growing pains: non-adherence with the immunosuppressive regimen in adolescent transplant recipients. Pediatr Transplant. 2005;9(3):381–90.
Samuel SM, Nettel-Aguirre A, Soo A, Hemmelgarn B, Tonelli M, Foster B. Avoidable hospitalizations in youth with kidney failure after transfer to or with only adult care. Pediatrics. 2014;133(4):e993-1000.
Watson AR. Non-compliance and transfer from paediatric to adult transplant unit. Pediatr Nephrol Berl Ger. 2000;14(6):469–72.
Prestidge C, Romann A, Djurdjev O, Matsuda-Abedini M. Utility and cost of a renal transplant transition clinic. Pediatr Nephrol Berl Ger. 2012;27(2):295–302.
Francis A, Johnson DW, Melk A, Foster BJ, Blazek K, Craig JC, et al. Survival after kidney transplantation during childhood and adolescence. Clin J Am Soc Nephrol CJASN. 2020;15(3):392–400.
Harden PN, Walsh G, Bandler N, Bradley S, Lonsdale D, Taylor J, et al. Bridging the gap: an integrated paediatric to adult clinical service for young adults with kidney failure. BMJ. 2012;1(344):e3718.
Watson AR, Harden PN, Ferris ME, Kerr PG, Mahan JD, Ramzy MF, et al. Transition from pediatric to adult renal services: a consensus statement by the International Society of Nephrology (ISN) and the International Pediatric Nephrology Association (IPNA). Kidney Int. 2011;80(7):704–7.
Kubota W, Honda M, Okada H, Hattori M, Iwano M, Akioka Y, et al. A consensus statement on health-care transition of patients with childhood-onset chronic kidney diseases: providing adequate medical care in adolescence and young adulthood. Clin Exp Nephrol. 2018;22(4):743–51.
Pape L, Ernst G. Health care transition from pediatric to adult care: an evidence-based guideline. Eur J Pediatr. 2022;181(5):1951–8. This article provides a comprehensive overview of recent evidence relating to the transition from pediatric to adult care, it is not specific to nephrology patients.
Toulany A, Gorter JW, Harrison M. A call for action: recommendations to improve transition to adult care for youth with complex health care needs. Paediatr Child Health. 2022;27(5):297–309. Recently published guidance on the transition of AYAs with complex medical conditions, highlighting key principles of transition care which are relevant to the safe transition of nephrology patients.
White PH, Cooley WC, Transitions Clinical Report Authoring Group, American Academy of Pediatrics, American Academy of Family Physicians, American College of Physicians, et al. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2018;142(5):e20182587.
Tangri N, Peach EJ, Franzén S, Barone S, Kushner PR. Patient management and clinical outcomes associated with a recorded diagnosis of stage 3 chronic kidney disease: the REVEAL-CKD Study. Adv Ther. 2023;40(6):2869–85.
Koenig CJ, Maguen S, Daley A, Cohen G, Seal KH. Passing the baton: a grounded practical theory of handoff communication between multidisciplinary providers in two department of veterans affairs outpatient settings. J Gen Intern Med. 2013;28(1):41–50.
Foster BJ, Dahhou M, Zhang X, Platt RW, Samuel SM, Hanley JA. Association between age and graft failure rates in young kidney transplant recipients. Transplantation. 2011;92(11):1237–43.
Van Arendonk KJ, James NT, Boyarsky BJ, Garonzik-Wang JM, Orandi BJ, Magee JC, et al. Age at graft loss after pediatric kidney transplantation: exploring the high-risk age window. Clin J Am Soc Nephrol CJASN. 2013;8(6):1019–26.
Gogtay N, Giedd JN, Lusk L, Hayashi KM, Greenstein D, Vaituzis AC, et al. Dynamic mapping of human cortical development during childhood through early adulthood. Proc Natl Acad Sci U S A. 2004;101(21):8174–9.
Matsuda-Abedini M, Marks SD, Foster BJ. Transition of young adult kidney transplant recipients. Pediatr Nephrol. 2023;38(2):383–90. A very recent review highlighting the important barriers to successful healthcare transition for kidney transplant recipients.
Hartung EA, Erus G, Jawad AF, Laney N, Doshi JJ, Hooper SR, et al. Brain magnetic resonance imaging findings in children and young adults with CKD. Am J Kidney Dis Off J Natl Kidney Found. 2018;72(3):349–59.
Hooper SR, Gerson AC, Butler RW, Gipson DS, Mendley SR, Lande MB, et al. Neurocognitive functioning of children and adolescents with mild-to-moderate chronic kidney disease. Clin J Am Soc Nephrol CJASN. 2011;6(8):1824–30.
Chen K, Didsbury M, van Zwieten A, Howell M, Kim S, Tong A, et al. Neurocognitive and educational outcomes in children and adolescents with CKD: a systematic review and meta-analysis. Clin J Am Soc Nephrol CJASN. 2018;13(3):387–97.
Murray PD, Brodermann MH, Gralla J, Wiseman AC, Harden PN. Academic achievement and employment in young adults with end-stage kidney disease. J Ren Care. 2019;45(1):29–40.
Rodriguez Cuellar CI, de la García Puente S, Hernández Moraria J, Bojórquez Ochoa A, Filler G, Zaltzman Grishevich S. High depression rates among pediatric renal replacement therapy patients: a cross-sectional study. Pediatr Transplant. 2019;23(8):e13591.
Bangudi S, Shankar D, Stanek C, Hart L, Nahata L, Cronin RM, et al. Primary care provider use and depression screening among transitioning adolescents and young adults with sickle cell disease. Blood. 2022;140(Supplement 1):7983–4.
Kreuzer M, Drube J, Prüfe J, Schaefer F, Pape L. Current management of transition of young people affected by rare renal conditions in the ERKNet. Eur J Hum Genet. 2019;27(12):1783–90.
Wildes DM, Costigan CS, Kinlough M, Flynn J, Dolan N, Riordan M, et al. Transitional care models in adolescent kidney transplant recipients - a systematic review. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc - Eur Ren Assoc. 2022;gfac175. A recent systematic review which served as a call to action, highlighting the need for improvement in transitional care models for patients with kidney transplants.
Narla NP, Ratner L, Bastos FV, Owusu SA, Osei-Bonsu A, Russ CM. Paediatric to adult healthcare transition in resource-limited settings: a narrative review. BMJ Paediatr Open. 2021;5(1):e001059.
Nagra A, McGinnity PM, Davis N, Salmon AP. Implementing transition: ready steady go. Arch Dis Child Educ Pract Ed. 2015;100(6):313–20.
Ardissino G, Testa S, Daccò V, Paglialonga F, Viganò S, Felice-Civitillo C, et al. Puberty is associated with increased deterioration of renal function in patients with CKD: data from the ItalKid Project. Arch Dis Child. 2012;97(10):885–8.
Celedón CG, Bitsori M, Tullus K. Progression of chronic renal failure in children with dysplastic kidneys. Pediatr Nephrol. 2007;22(7):1014–20.
Yassaee A, Hale D, Armitage A, Viner R. The impact of age of transfer on outcomes in the transition from pediatric to adult health systems: a systematic review of reviews. J Adolesc Health Off Publ Soc Adolesc Med. 2019;64(6):709–20.
Zhong Y, Gilleskie DB, van Tilburg MAL, Hooper SR, Rak E, Javalkar K, et al. Longitudinal self-management and/or transition readiness per the TRxANSITION index among patients with chronic conditions in pediatric or adult care settings. J Pediatr. 2018;203:361-370.e1.
McPherson M, Thaniel L, Minniti CP. Transition of patients with sickle cell disease from pediatric to adult care: assessing patient readiness. Pediatr Blood Cancer. 2009;52(7):838–41.
Schwartz LA, Tuchman LK, Hobbie WL, Ginsberg JP. A social-ecological model of readiness for transition to adult-oriented care for adolescents and young adults with chronic health conditions. Child Care Health Dev. 2011;37(6):883–95.
van Staa AL, Jedeloo S, van Meeteren J, Latour JM. Crossing the transition chasm: experiences and recommendations for improving transitional care of young adults, parents and providers. Child Care Health Dev. 2011;37(6):821–32.
Sawicki GS, Lukens-Bull K, Yin X, Demars N, Huang IC, Livingood W, et al. Measuring the transition readiness of youth with special healthcare needs: validation of the TRAQ–Transition Readiness Assessment Questionnaire. J Pediatr Psychol. 2011;36(2):160–71.
Wood DL, Sawicki GS, Miller MD, Smotherman C, Lukens-Bull K, Livingood WC, et al. The Transition Readiness Assessment Questionnaire (TRAQ): its factor structure, reliability, and validity. Acad Pediatr. 2014;14(4):415–22.
Cohen E, Gandhi S, Toulany A, Moore C, Fu L, Orkin J, et al. Health care use during transfer to adult care among youth with chronic conditions. Pediatrics. 2016;137(3):e20152734.
Cohen SE, Hooper SR, Javalkar K, Haberman C, Fenton N, Lai H, et al. Self-management and transition readiness assessment: concurrent, predictive and discriminant validation of the STARx Questionnaire. J Pediatr Nurs. 2015;30(5):668–76.
Díaz-González de Ferris ME, Del Villar-Vilchis M, Guerrero R, Barajas-Valencia VM, Vander-Schaaf EB, de Pomposo A, et al. Self-management and health care transition among adolescents and young adults with chronic kidney disease: medical and psychosocial considerations. Adv Chronic Kidney Dis. 2017;24(6):405–9.
Ferris M, Cohen S, Haberman C, Javalkar K, Massengill S, Mahan JD, et al. Self-management and transition readiness assessment: development, reliability, and factor structure of the STARx Questionnaire. J Pediatr Nurs. 2015;30(5):691–9.
Ferris ME, Harward DH, Bickford K, Layton JB, Ferris MT, Hogan SL, et al. A clinical tool to measure the components of health-care transition from pediatric care to adult care: the UNC TR(x)ANSITION scale. Ren Fail. 2012;34(6):744–53.
Scarponi D, Cammaroto V, Pasini A, La Scola C, Mencarelli F, Bertulli C, et al. Multidisciplinarity in transition pathways for patients with kidney disease: the current state of play. Front Pediatr [Internet]. 2021 [cited 2023 Jul 28];9. Available from: https://www.frontiersin.org/articles/10.3389/fped.2021.689758.
Nishi L, Langman C, Ghossein C. A nephrology pediatric to adult transition clinic: a pilot program. Kidney Med. 2019;1(6):405–6.
Watson AR. Problems and pitfalls of transition from paediatric to adult renal care. Pediatr Nephrol Berl Ger. 2005;20(2):113–7.
Weitz M, Heeringa S, Neuhaus TJ, Fehr T, Laube GF. Standardized multilevel transition program: does it affect renal transplant outcome? Pediatr Transplant. 2015;19(7):691–7.
Harmer MJ, Everitt LH, Parker L, Davis N, Connett G, Nagra A. Structured transition is associated with improved outcomes in diabetes. Pract Diabetes. 2022;39(1):18–22a.
Raina R, Wang J, Krishnappa V. Structured transition protocol for children with cystinosis. Front Pediatr. 2017;5:191.
Schraeder K, Allemang B, Scott C, McBrien K, Dimitropoulos G, Felske A, et al. Primary care during the transition to adult care for adolescents involved with pediatric specialty services: a scoping review protocol. Syst Rev. 2021;10(1):46.
Lovera LA, Trejos J, Encarnación LK, Pereira C, Padilla A, Restrepo JM, et al. Caracterización de adolescentes trasplantados de riñón y en protocolo pretasplante en Cali, Colombia. Enferm Nefrológica. 2022;25(2):133–9.
Muñoz FNB, Montilla LAL, Oviedo LAA, Restrepo JMR. Significado de la transición infancia-adolescencia-juventud en personas con enfermedad renal crónica. Cult Los Cuid. 2018;50:34–47.
Paone MC, Wigle M, Saewyc E. The ON TRAC model for transitional care of adolescents. Prog Transplant Aliso Viejo Calif. 2006;16(4):291–302.
Corr M, McKeaveney C, Wurm F, Courtney A, Noble H. Patient education interventions for adolescent and young adult kidney transplant recipients- a scoping review. PLoS ONE. 2023;18(7):e0288807.
Ferris ME, Mahan JD. Pediatric chronic kidney disease and the process of health care transition. Semin Nephrol. 2009;29(4):435–44.
Von Scheven E, Tucker LB, Moorthy LN, Lawson EF, Neville C, DaCosta D, et al. Improving transition readiness and quality of life (QOL) with a pediatric lupus health passport. Pediatr Rheumatol. 2012;10(1):A23.
McQuillan RF, Toulany A, Kaufman M, Schiff JR. Benefits of a transfer clinic in adolescent and young adult kidney transplant patients. Can J Kidney Health Dis. 2015;1(2):81.
Allemang B, Allan K, Johnson C, Cheong M, Cheung P, Odame I, et al. Impact of a transition program with navigator on loss to follow-up, medication adherence, and appointment attendance in hemoglobinopathies. Pediatr Blood Cancer. 2019;66(8):e27781.
Dimitropoulos G, Morgan-Maver E, Allemang B, Schraeder K, Scott SD, Pinzon J, et al. Health care stakeholder perspectives regarding the role of a patient navigator during transition to adult care. BMC Health Serv Res. 2019;19(1):390.
Luke A, Doucet S, Azar R. Paediatric patient navigation models of care in Canada: an environmental scan. Paediatr Child Health. 2018;23(3):e46-55.
Wells KJ, Battaglia TA, Dudley DJ, Garcia R, Greene A, Calhoun E, et al. Patient navigation: state of the art or is it science? Cancer. 2008;113(8):1999–2010.
Johnson MAJ, Javalkar K, van Tilburg M, Haberman C, Rak E, Ferris ME. The relationship of transition readiness, self-efficacy, and adherence to preferred health learning method by youths with chronic conditions. J Pediatr Nurs. 2015;30(5):e83-90.
Fair C, Rupp S, Hart L, Alvarez-Elías A, Perry M, Ferris M. Defining successful transition: pediatric provider perspective. In: Applied Mathematical Modelling. 2018. p 191–200.
Low JK, Manias E. Use of technology-based tools to support adolescents and young adults with chronic disease: systematic review and meta-analysis. JMIR MHealth UHealth. 2019;7(7):e12042.
Green JA, Ephraim PL, Hill-Briggs FF, Browne T, Strigo TS, Hauer CL, et al. Putting patients at the center of kidney care transitions: PREPARE NOW, a cluster randomized controlled trial. Contemp Clin Trials. 2018;73:98–110.
Green JA, Ephraim PL, Hill-Briggs F, Browne T, Strigo TS, Hauer CL, et al. Integrated digital health system tools to support decision making and treatment preparation in CKD: the PREPARE NOW Study. Kidney Med. 2021;3(4):565-575.e1.
Barney A, Buckelew S, Mesheriakova V, Raymond-Flesch M. The COVID-19 pandemic and rapid implementation of adolescent and young adult telemedicine: challenges and opportunities for innovation. J Adolesc Health. 2020;67(2):164.
Klein JD, Koletzko B, El-Shabrawi MH, Hadjipanayis A, Thacker N, Bhutta Z. Promoting and supporting children’s health and healthcare during COVID-19 – International Paediatric Association Position Statement. Arch Dis Child. 2020;105(7):620–4.
Committee on Improving the Health, Safety, and Well-Being of YoungAdults, Board on Children, Youth, and Families, Institute of Medicine, National Research Council. Investing in the health and well-being of young adults [Internet]. Bonnie RJ, Stroud C, Breiner H, editors. Washington (DC): National Academies Press (US); 2015 [cited 2023 Nov 30]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK284787/.
Transition to adulthood for youth with chronic conditions and special health care Needs. J Adolesc Health. 2020;66(5):631–4.
Author information
Authors and Affiliations
Contributions
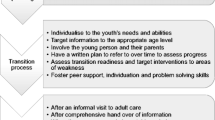
CC wrote the main manuscript text and prepared the original figures and tables. DW, AC, and AM edited the main text and creatively contributed to conceptualizing the tables and figures. All authors critically reviewed the final manuscript and agree to its submission.
Corresponding author
Ethics declarations
Ethical Approval
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Costigan, C.S., Wildes, D.M., Alvarez-Elias, A.C. et al. Safely Transitioning Patients in Nephrology. Curr Pediatr Rep 12, 1–10 (2024). https://doi.org/10.1007/s40124-024-00312-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40124-024-00312-y