Abstract
In the United Arab Emirates, retinopathy has been shown to be present in 19% of the diabetic population, with diabetes identified in up to 40% of individuals aged over 55 years. Despite the prevalence of diabetic retinal diseases, there are no unified national guidelines on the management of diabetic macular edema (DME). These published guidelines are based on evidence taken from the literature and published trials of therapies, and consensus opinion of a representative expert panel with an interest in this condition, convened by the Emirates Society of Ophthalmology. The aim is to provide evidence-based, clinical guidance for the best management of different aspects of DME, with a special focus on vision-threatening diabetic retinopathy. Treatment should be initiated in patients with best-corrected visual acuity 20/30 or worse, and/or features of DME as seen on optical coherence tomography (OCT) with central retinal thickness (CRT) of at least 300 μm or in symptomatic patients with vision better than 20/25, and/or CRT less than 300 μm where there are OCT features consistent with center-involving macular edema. The treatment of DME is effective irrespective of glycated hemoglobin (HbA1c) level, and treatment must not be denied or delayed in order to optimize systemic parameters. All ophthalmic treatment options should be discussed with the patient for better compliance and expectations. Non-center-involving DME can be initially observed until progression toward the center is documented. Macular laser no longer has a primary role in center-involving DME, and anti-vascular endothelial growth factor (anti-VEGF) therapy should be considered as first-line treatment for all patients, unless contraindicated. If anti-VEGF is contraindicated, a steroid dexamethasone implant can be considered for first-line treatment. Recommendations for the treatment of DME in special circumstances and in relapsing and refractory DME are also discussed.
Similar content being viewed by others
Driven by the increasing prevalence of diabetes, diabetic macular edema (DME) is becoming an increasing concern for ophthalmologists around the globe and particularly in the United Arab Emirates (UAE). |
These guidelines provide treatment recommendations for both center-involving and non-center-involving DME, including the use of anti-vascular endothelial growth factor (VEGF) injections, and the treatment of DME in special circumstances. |
The aim of these guidelines on the management of DME is to continuously advance the standard of ophthalmology practice in the UAE, in order to improve eye and visual health in the UAE community and beyond. |
Introduction
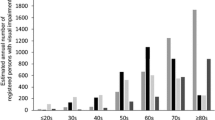
Diabetic macular edema (DME) is becoming an increasing concern for ophthalmologists around the globe, driven by the increasing prevalence of diabetes. In the United Arab Emirates (UAE), rapid urbanization and socioeconomic development have led to the widespread adoption of a sedentary lifestyle and Westernized diet in the local population; consequently, there is a high prevalence of both obesity and diabetes. In 2019, International Diabetes Federation (IDF) statistics reported a diabetes prevalence rate of 16.3% for the adult population in the UAE aged between 20 and 79 years, and higher than for other Middle East and North Africa countries [1]. A survey of Emiratis and expatriates in 1999–2000 reported a 20.0% rate in the 20–64-years age group, using the oral glucose tolerance test, similar to rates reported in neighboring Middle East and North Africa countries [2]. Since then, there have been few studies on diabetes prevalence in the UAE.
The Weqaya screening program conducted in Abu Dhabi collected data from 50,138 participants between 2008 and 2010 [3]. This showed age-standardized prevalence rates of 17.6% for diabetes and 27.1% for pre-diabetes. More recently, a study of UAE citizens in the Northern Emirates found that the prevalence of diabetes was 25.1% [4]. It was higher in UAE citizens than in expatriates (25% versus 13–19% depending on the country) [1, 2, 5]. The prevalence of diabetes rose with age to a maximum of 40% after the age of 55 years, and the prevalence of impaired fasting glycemia was 5% in men and 7% in women. Overall, 41% of individuals with diabetes were undiagnosed prior to the survey [2]. Obesity was common in all ethnic groups and the presence of diabetes was associated with increasing waist-to-hip ratio, age, and systolic blood pressure and ethnicity [2]. Comorbidity with glucose intolerance occurred with obesity in 8% of individuals and with hypertension in 5%.
The aim of these guidelines on the management of DME is to continuously advance the standard of ophthalmology practice in the UAE, in order to improve eye and visual health in the UAE community and beyond, and to provide evidence-based, clinical guidance for the best management of different aspects of diabetic eye disease. The foundations of the guidelines are based on evidence taken from the literature and published trials of therapies, as well as consensus opinion of a representative expert panel convened by the Emirates Society of Ophthalmology in the second half of 2019 with an interest in this condition. As this article is based on previously conducted studies, it does not contain any studies with human participants or animals performed by any of the authors.
The scope of the guidelines is limited to management of DME with a special focus on vision-threatening diabetic retinopathy. The guidelines offer recommendations regarding service provision to facilitate delivery of optimal clinical care for patients and have been prepared primarily for ophthalmologists. They are, however, also relevant for other healthcare professionals, service providers, and commissioning organizations, such as insurance companies, as well as patient groups. This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Recommendations
Treatment Initiation
DME should be treated to improve vision when it is decreased, to maintain vision, and to prevent structural damage to the macula [6]. Treatment is initiated on the basis of careful assessment of the structure and function of the macula [7]. Conditions needed to initiate treatment are best-corrected visual acuity 20/30 or worse, and/or features of DME as seen on optical coherence tomography (OCT) with central retinal thickness (CRT) of at least 300 μm [6, 8] or symptomatic patients with vision better than 20/25 [9], and/or CRT less than 300 μm [8, 9] with OCT features consistent with center-involving macular edema. OCT intra-device reproducibility is satisfactory; however, CRT cutoffs are devise-specific [9] since retinal thickness and volume measurements differ between systems [10].
Once the decision to treat has been made, it is recommended that visual acuity be assessed before initiation of treatment, after the initial loading dose of 3–6 intravitreal anti-vascular endothelial growth factor (VEGF) injections, at monthly intervals, and periodically during treatment, as per physician’s discretion [11, 12]. It may, however, be assessed at every visit. It is also recommended to check intraocular pressure (IOP) before initiation of treatment, after loading dose, and periodically during treatment, as per physician’s discretion [6, 13]. Again, this may be carried out at every visit [6, 13]. Spectral-domain OCT is recommended before the initiation of treatment, after loading dose, and periodically during treatment, as per physician’s discretion [14, 15]. Ocular fundus exam is recommended before the initiation of treatment and periodically during treatment, as per physician’s discretion [15], and fundus fluorescein angiography (FFA) may be carried out before the initiation of treatment and periodically to assess the macular perfusion and/or peripheral ischemia [6, 15]. OCT angiography can be used for evaluation of macular blood supply and the presence of macular ischemia [15].
General Guidance in DME Management
The treatment of DME is effective irrespective of glycated hemoglobin (HbA1c) level, and treatment must not be denied or delayed in order to optimize systemic parameters [16,17,18]; although it is recommended to check for other ocular causes of vision loss such as cataract progression.
Systemic management of patients with DME consists of optimal control of diabetes mellitus and HbA1c [16,17,18], arterial hypertension [19,20,21], dyslipidemia [22,23,24,25,26,27], smoking cessation [24, 28], weight loss if required for a normal body mass index [28], renal impairment [24, 28], and sleep apnea [28], as all are factors associated with better management of DME. Patients should therefore be encouraged to pursue this with their diabetologist. Fenofibrate [29] and statins [30] can be recommended to the family physicians/endocrinologists as anti-dyslipidemia medication, as both have a positive effect on diabetic retinopathy and DME. We recommend also checking for any new medications that can exacerbate DME, such as glitazones [17, 28, 31].
It is important to perform FFA and/or OCT angiography in order to assess macular ischemia in those cases where there is no improvement in visual acuity despite a reduction in macular thickness after a loading dose with anti-VEGF injections or a dexamethasone implant [32, 33]. Importantly, all ophthalmic treatment options should be discussed with the patient for better compliance and expectations [34].
Clinically significant macular edema is retinal thickening at or within 500 μm of the center of the macula; and/or hard exudates at or within 500 μm of the center of the macula if associated with thickening of the adjacent retina, and/or zone(s) of retinal thickening one disc area in size, any part of which is within one disc diameter from the center of the macula [35]. A flowchart for the management of DME is shown in Fig. 1.
Flowchart for DME management. *Rule out contraindications for anti-VEGF. **Rule out contraindications for dexamethasone implant. ***Poor response: failure to gain at least 5 letters of vision; failure to reduce CRT by 10%. ****Rule out contraindications for fluocinolone implant. BCVA best-corrected visual acuity, CRT central retinal thickness, dex, dexamethasone, DME diabetic macular edema, FFA fundus fluorescein angiography, IOP intraocular pressure, MI myocardial infarction, OCT optical coherence tomography, OCTA optical coherence tomography angiography, PRN pro re nata, VEGF vascular endothelial growth factor
Treatment Recommendations for Non-Center-Involving DME
Non-center-involving DME is retinal thickening in the macula that does not involve the central subfield zone, 1 mm in diameter on OCT [6]. It can be initially observed until progression toward the center is documented. Anti-VEGF therapy can be initiated, or FFA-guided focal laser treatment administered to leaking microaneurysms at least 300–500 μm from the center of the macula [36]. Focal laser treatment should, however, only be performed by a retina specialist in specific circumstances [36, 37].
Treatment Recommendation for Center-Involving DME
Center-involving macular edema is retinal thickening in the macula that involves the central subfield zone, 1 mm in diameter on OCT [6]. Macular laser no longer has a primary role in center-involving DME [36] and anti-VEGF therapy should be considered as first-line treatment for all patients, unless contraindicated [38, 39]. A steroid dexamethasone implant can be used as a first-line treatment if anti-VEGF is contraindicated, or if there is poor compliance with the anti-VEGF regimen treatment, and may be recommended in patients who are vitrectomized, pseudophakic, or with chronic DME [40, 41]. IOP should be monitored in patients in whom a steroid implant is used [41].
Intravitreal Anti-VEGF Therapy
Treatment goals and strategy should be discussed with patients [28] and treatment algorithms may vary according to patient’s and physician’s preference [42]. Physicians should also ensure the patient’s systemic diseases, particularly dyslipidemia and hypertension, are well controlled [15]. Fixed, pro re nata, and treat-and-extend dosing (based on visual acuity and OCT) can be considered [43]. Only licensed and approved anti-VEGF agents, such as intravitreally administered aflibercept and ranibizumab, should be used, and no biosimilars/medicines are allowed to be imported to the country and used other than what is legally distributed [44, 45].
All patients treated with anti-VEGF agents should have a loading dose of 3–6 injections [44, 46]. The loading dose, 3–6 injections at monthly intervals, is based on the treatment response assessed by visual acuity and OCT [44, 46], keeping inter-OCT variability and device-specific measurements in consideration throughout patient follow-up [10]. The estimated number of optimal anti-VEGF injections is 8–9 injections in the first year of treatment (including the loading dose), and 5–6 injections in the second year [44, 46].
A poor response to anti-VEGF treatment, after the loading dose of 3–6 injections at monthly intervals, is defined as failure to gain at least five letters of vision and/or reduce CRT by 10% [47]. These criteria should be considered before switching, which may include switching to another anti-VEGF agent or to steroids after the loading phase has been completed [47]. Caution is warranted when considering switching therapies for persistent DME following three or more injections; improvements can be achieved with continued anti-VEGF treatment rather than switching therapies [48].
Physicians should consider assessing macular ischemia with FFA or OCT angiography [6, 15, 49], and OCT should be used to rule out epiretinal membrane and/or vitreomacular traction [15]. As a safety practice, it is advised not to treat with anti-VEGF agents for a minimum of 3 months after myocardial infarction or stroke [50]. Anti-VEGF treatment is not recommended during pregnancy or while breast-feeding [51]. In such cases, steroid should be used as first-line treatment [52]. Intravitreal anti-VEGF and steroid therapy should also be deferred in case of active infection [52].
Steroid Implants
Physicians should be aware that a dexamethasone implant does not usually last for more than 4 months, with a peak effect at 6–8 weeks [53,54,55,56,57]. Thus, the estimated number of dexamethasone implants is 3–4 injections over 12 months. In cases where there is a good response and if DME recurrence is less frequent than every 6 months, it is recommended to continue with dexamethasone implants [56]. The frequent recurrence of fluids (less than 3 months) after dexamethasone implant necessitates further discussion and likely a switch to anti-VEGF therapy.
If the patient does not wish to receive implants every 4 months, switching to a fluocinolone implant should be considered [47, 58,59,60]. Prior to a fluocinolone implant, a steroid challenge may be needed (i.e., starting with a dexamethasone implant, or alternatively topical steroid eye drops in compliant patients) [61,62,63]. A wide range of OCT/OCT angiography biomarkers exist for predicting treatment outcomes in DME; patients with submacular fluid, hyperreflective foci, intra-retinal cysts, and a disorganization of the continuous inner retinal layer (also referred to as DRIL) may respond better to dexamethasone implants than those without these features [64] and vessel density and foveal avascular zone may also be useful in predicting response to treatment [32]. Not every responder to dexamethasone implants will respond to fluocinolone implants, and top-up treatment may be required in addition to the fluocinolone implant, including anti-VEGF treatment and dexamethasone implants [31, 65]. Furthermore, around 10% of patients treated with dexamethasone implants will have an IOP increase of greater than 25 mmHg. If a patient develops elevated IOP with dexamethasone implants, it is not recommended to use a fluocinolone implant [66,67,68].
Pseudophakic patients are preferred for the use of steroids, otherwise patients have to be informed about the high risk for cataract surgery [15], and it is known that cataract surgery predisposes to, or worsens DME [31]. Contraindications to dexamethasone and fluocinolone acetonide intravitreal implants are eyes with active or suspected ocular or periocular infection; advanced glaucoma (requiring more than three medications), non-intact posterior capsule (yttrium aluminum garnet [YAG] capsulotomy excluded), eyes with aphakia, and hypersensitivity to dexamethasone implant or a fluocinolone acetonide intravitreal implant [58, 69].
Relapsing and Refractory DME
Relapsing DME (recurrence of DME after 3–6 months from last intravitreal anti-VEGF injection) allows the repetition of the same treatment used previously if there is clear evidence of a previous response; otherwise, the patient should be treated as being a new patient, starting with any available treatment option (i.e., anti-VEGF or dexamethasone implant) [6]. Refractory DME is defined as DME not responding to a full course of anti-VEGF agents and steroid implants. A combination therapy with anti-VEGF and steroids might be considered, although there is no strong evidence for an additional benefit with combination therapy, and referral to a retinal surgeon for vitrectomy if epiretinal membrane or vitreomacular traction is confirmed on OCT [70,71,72].
Treatment of DME in Special Circumstances
DME and Proliferative Diabetic Retinopathy
Physicians should initially assess visual acuity and conduct a fully dilated fundus exam [36].
Anti-VEGF agents are recommended in the first-line treatment of center-involving DME unless contraindicated, and in cases of non-center-involving DME and proliferative diabetic retinopathy, the use of either anti-VEGF treatment or pan-retinal photocoagulation (PRP) are valid options [73].
PRP remains the gold standard treatment for proliferative diabetic retinopathy (PDR). Navigated laser treatment achieves more uniform laser burns with less pain during shorter treatment duration in comparison with conventional pattern laser [74]. Anti-VEGF agents and PRP are both licensed treatments for the condition, and their combination can be used while the addition of laser can reduce the frequency of injections [73].
After the proliferative diabetic retinopathy is treated, anti-VEGF injections may continue for the treatment of DME. When choosing between anti-VEGF and PRP as first-line therapy for PDR, treatment decisions should be guided by consideration of the relative advantages of each therapeutic modality and anticipated patient compliance with follow-up and treatment recommendations [73]. Core management of the retinopathy status is recommended either by continuing anti-VEGF injections or initiating PRP [73].
Cataract Surgery
In order to stabilize DME in planning for cataract surgery, it is recommended to give either anti-VEGF injections or steroids 1–2 weeks preoperatively or at the time of surgery [75, 76]. The use of non-steroidal anti-inflammatory drug topical eye drops is recommended postoperatively [75, 77].
Fibrovascular Membranes and Tractional Retinal Detachment Near or Involving the Macula
It is recommended not to give any anti-VEGF injections, unless the physician is planning vitreoretinal surgery or has planned access to a retinal surgery service or to a retina surgeon [78].
Vitreomacular Traction/Epiretinal Membrane
Physicians should consult with the vitreoretinal surgeon before giving injections in patients with diabetes in whom a vitreomacular traction or epiretinal membrane is shown [79].
Vitreous Hemorrhage in Patients with DME
Vitreous hemorrhage is frequent in PDR and, in the absence of vitreomacular traction, many vitreous hemorrhages do not need vitreoretinal surgery. Physicians should consult with the vitreoretinal surgeon for patients with DME and vitreous hemorrhage [80].
DME and Pregnancy
For DME in pregnancy, first-line treatments should remain as blood glucose control and laser therapy. Pregnancy is a contraindication for anti-VEGF treatment for DME [81,82,83]. Intravitreal dexamethasone implant may be a safe and effective treatment modality for managing severe DME as first-line treatment [81, 84, 85]. Laser is another option for non-center-involving macular edema [86]. Alternatively, treatment can be deferred until after delivery. Steroid treatment should be offered only in the second or third trimesters, while the risks of IOP elevation, cataract development, and the remote risk of fetal harm should be fully discussed with the patient [81, 84, 85].
Bilateral Injection
The decision of unilateral versus bilateral injections should be at the surgeon’s discretion [87]. All risks and benefits of the procedure should be well explained to the patient, and the option of unilateral injection should be properly explained [87]. The surgeon should take the maximum precautions to avoid all risks of bilateral injection complications, as every eye should be treated as a separate procedure: precautions also can include (but are not limited to) separate gloves; separate vials with different patch number; separate surgical mask; and separate needles, syringes, and speculums, as this should be used for each eye with full preparation [36, 88].
Iodine
The use of 5% iodine in the fornix for 60 s per eye is recommended [89,90,91]. In cases of clear allergy to iodine, chlorhexidine 0.1% aqueous solution can be used with caution and warning of endophthalmitis [92].
Injection Room and International and Local Infection Control
Anti-VEGF and steroid injections can be given either in theater or in a dedicated clean room that meets international and local infection control guidelines [92,93,94]. The clean room should be separated from the examination room, adequately equipped, and approved by the appropriate hospital teams (microbiology/infection control/health and safety). The details of such specifications should be discussed with the local health and safety representatives. Any room where minor operations take place is suitable as long as infected cases are excluded.
Mask and Gloves
The physician must wear a mask and sterile gloves [88], and the patient must wear a mask covering the nose or a drape [95]. The InVitrea device can be used instead of lid speculum and caliper [95], and the physician should ensure sterility of the periorbital skin with 10% povidone-iodine [88]. Prior to the procedure, the patient should be advised to avoid talking while lying down and prior to mask/drape placement, to avoid air droplet contamination [88, 95, 96].
Post-Injection Management and Follow-up
Antibiotics are not recommended, either pre- or post-injection [88, 97]. Patients should be given information about postoperative complications and a telephone number to contact in case of symptoms including increase in redness, eye pain, vision reduction, or any symptoms of endophthalmitis [98].
Summary
The Emirates Society of Ophthalmology clarifies that these guidelines are made by retinal specialists on the basis of international guidelines and studies, and clinical trials, which have been fully acknowledged. These include recommendations from the International Diabetes Federation in 2019 [28], and from the European Society of Retina Specialists and International Council of Ophthalmology in 2017 [15, 36]. As such, these guidelines developed by the Emirates Society of Ophthalmology may also be applicable in other regions of the world, especially where country- or region-specific guidelines do not exist.
It is our hope that consensus guidelines will assist in advancing the standard of ophthalmology practice in the UAE, and consequently improve eye and visual health in the UAE community.
The authors have made considerable efforts to ensure that the information upon which the recommendations are based is current and accurate. The guidelines do not cover rare, complex, complicated, or unusual cases and it is recommended that readers refer to other relevant sources of information such as summaries of product characteristics for pharmaceutical products, as well as other clinical literature or guidelines where necessary. In all cases, the management of each individual patient should be individualized on the basis of their specific disease characteristics, treatment requirements, and subsequent responses to therapy.
References
International Diabetes Federation. 2019. IDF Diabetes Atlas, Ninth Edition. https://www.diabetesatlas.org/upload/resources/material/20200302_133351_IDFATLAS9e-final-web.pdf.
Malik M, Bakir A, Saab BA, King H. Glucose intolerance and associated factors in the multi-ethnic population of the United Arab Emirates: results of a national survey. Diabetes Res Clin Pract. 2005;69:188–95.
Hajat C, Harrison O, Al SZ. Weqaya: a population-wide cardiovascular screening program in Abu Dhabi, United Arab Emirates. Am J Public Health. 2012;102:909–14.
Sulaiman N, Mahmoud I, Hussein A, et al. Diabetes risk score in the United Arab Emirates: a screening tool for the early detection of type 2 diabetes mellitus. BMJ Open Diabetes Res Care. 2018;6: e000489.
Alawadi F, Abusnana S, Afandi B, et al. Emirates Diabetes Society consensus guidelines for the management of type 2 diabetes mellitus–2020. Dubai Diabetes Endocrinol J. 2020;26:1–20.
Wong TY, Sun J, Kawasaki R, et al. Guidelines on diabetic eye care: the International Council of Ophthalmology recommendations for screening, follow-up, referral, and treatment based on resource settings. Ophthalmology. 2018;125:1608–22.
Cohen SR, Gardner TW. Diabetic retinopathy and diabetic macular edema. Dev Ophthalmol. 2016;55:137–46.
Giocanti-Auregan A, Hrarat L, Qu LM, et al. Functional and anatomical outcomes in patients with serous retinal detachment in diabetic macular edema treated with ranibizumab. Invest Ophthalmol Vis Sci. 2017;58:797–800.
Glassman AR, Baker CW, Beaulieu WT, et al. Assessment of the DRCR Retina Network approach to management with initial observation for eyes with center-involved diabetic macular edema and good visual acuity: a secondary analysis of a randomized clinical trial. JAMA Ophthalmol. 2020;138:341–9.
Lammer J, Scholda C, Prunte C, et al. Retinal thickness and volume measurements in diabetic macular edema: a comparison of four optical coherence tomography systems. Retina. 2011;31:48–55.
Wells JA, Glassman AR, Jampol LM, et al. Association of baseline visual acuity and retinal thickness with 1-year efficacy of aflibercept, bevacizumab, and ranibizumab for diabetic macular edema. JAMA Ophthalmol. 2016;134:127–34.
Mitchell P, Sheidow TG, Farah ME, et al. Effectiveness and safety of ranibizumab 0.5 mg in treatment-naive patients with diabetic macular edema: results from the real-world global LUMINOUS study. PLoS ONE. 2020;15: e0233595.
Kanchanaranya N, Lam W. Treatment of refractory diabetic macular edema: triamcinolone vs bevacizumab and ‘switch-over’ treatment. Clin Experiment Ophthalmol. 2008;36(Suppl 1):A459–584.
Wells JA, Glassman AR, Ayala AR, et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N Engl J Med. 2015;372:1193–203.
Schmidt-Erfurth U, Garcia-Arumi J, Bandello F, et al. Guidelines for the management of diabetic macular edema by the European Society of Retina Specialists (EURETINA). Ophthalmologica. 2017;237:185–222.
Davis MD, Fisher MR, Gangnon RE, et al. Risk factors for high-risk proliferative diabetic retinopathy and severe visual loss: early treatment diabetic retinopathy study report #18. Invest Ophthalmol Vis Sci. 1998;39:233–52.
Klein R, Klein BE, Moss SE, Davis MD, DeMets DL. Glycosylated hemoglobin predicts the incidence and progression of diabetic retinopathy. JAMA. 1988;260:2864–71.
The Diabetes Control and Complications Trial group. The effect of intensive diabetes treatment on the progression of diabetic retinopathy in insulin-dependent diabetes mellitus. Arch Ophthalmol. 1995;113:36–51.
Klein R, Klein BE, Moss SE, Davis MD, DeMets DL. The Wisconsin epidemiologic study of diabetic retinopathy. II. Prevalence and risk of diabetic retinopathy when age at diagnosis is less than 30 years. Arch Ophthalmol. 1984;102:520–6.
Snow V, Weiss KB, Mottur-Pilson C, Clinical Efficacy Assessment Subcommittee of the American College of Physicians. The evidence base for tight blood pressure control in the management of type 2 diabetes mellitus. Ann Intern Med. 2003;138:587–92.
UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998;317:703–13.
Shi R, Zhao L, Wang F, et al. Effects of lipid-lowering agents on diabetic retinopathy: a meta-analysis and systematic review. Int J Ophthalmol. 2018;11:287–95.
Chew EY, Klein ML, Ferris FL 3rd, et al. Association of elevated serum lipid levels with retinal hard exudate in diabetic retinopathy Early Treatment Diabetic Retinopathy Study (ETDRS) report 22. Arch Ophthalmol. 1996;114:1079–84.
Lopes-Virella MF, Baker NL, Hunt KJ, et al. High concentrations of AGE-LDL and oxidized LDL in circulating immune complexes are associated with progression of retinopathy in type 1 diabetes. Diabetes Care. 2012;35:1333–40.
Lyons TJ, Jenkins AJ, Zheng D, et al. Diabetic retinopathy and serum lipoprotein subclasses in the DCCT/EDIC cohort. Invest Ophthalmol Vis Sci. 2004;45:910–8.
Klein R, Sharrett AR, Klein BE, et al. The association of atherosclerosis, vascular risk factors, and retinopathy in adults with diabetes: the atherosclerosis risk in communities study. Ophthalmology. 2002;109:1225–34.
van Leiden HA, Dekker JM, Moll AC, et al. Blood pressure, lipids, and obesity are associated with retinopathy: the Hoorn Study. Diabetes Care. 2002;25:1320–5.
International Diabetes Federation. Clinical practice recommendations for managing diabetic macular edema. 2019. https://www.idf.org/component/attachments/?task=download&id=2153.
Srinivasan S, Hande P, Shetty J, Murali S. Efficiency of fenofibrate in facilitating the reduction of central macular thickness in diabetic macular edema. Indian J Ophthalmol. 2018;66:98–105.
Kang EY, Chen TH, Garg SJ, et al. Association of statin therapy with prevention of vision-threatening diabetic retinopathy. JAMA Ophthalmol. 2019;137:363–71.
Amoaku WM, Ghanchi F, Bailey C, et al. Diabetic retinopathy and diabetic macular oedema pathways and management: UK Consensus Working Group. Eye (Lond). 2020;34:1–51.
Khadamy J, Abri Aghdam K, Falavarjani KG. An update on optical coherence tomography angiography in diabetic retinopathy. J Ophthalmic Vis Res. 2018;13:487–97.
Bradley PD, Sim DA, Keane PA, et al. The evaluation of diabetic macular ischemia using optical coherence tomography angiography. Invest Ophthalmol Vis Sci. 2016;57:626–31.
Dawn AG, Lee PP. Patient expectations for medical and surgical care: a review of the literature and applications to ophthalmology. Surv Ophthalmol. 2004;49:513–24.
Early Treatment Diabetic Retinopathy Study Group. Early Treatment Diabetic Retinopathy Study design and baseline patient characteristics. ETDRS report number 7. Ophthalmology. 1991;98:741–56.
International Council of Ophthalmology. ICO guidelines for diabetic eye care. 2017. http://www.icoph.org/downloads/ICOGuidelinesforDiabeticEyeCare.pdf.
Early Treatment Diabetic Retinopathy Study Research Group. Treatment techniques and clinical guidelines for photocoagulation of diabetic macular edema. Early Treatment Diabetic Retinopathy Study Report Number 2. Ophthalmology. 1987;94:761–74.
Sugimoto M, Tsukitome H, Okamoto F, et al. Clinical preferences and trends of anti-vascular endothelial growth factor treatments for diabetic macular edema in Japan. J Diabetes Investig. 2019;10:475–83.
Cornel S, Adriana ID, Mihaela TC, et al. Anti-vascular endothelial growth factor indications in ocular disease. Rom J Ophthalmol. 2015;59:235–42.
Querques G, Darvizeh F, Querques L, et al. Assessment of the real-life usage of intravitreal dexamethasone implant in the treatment of chronic diabetic macular edema in France. J Ocul Pharmacol Ther. 2016;32:383–9.
Urbancic M, Gardasevic TI. Dexamethasone implant in the management of diabetic macular edema from clinician’s perspective. Clin Ophthalmol. 2019;13:829–40.
Bandello F, Cunha-Vaz J, Chong NV, et al. New approaches for the treatment of diabetic macular oedema: recommendations by an expert panel. Eye. 2012;26:485–93.
Yoshitake T, Murakami T, Suzuma K, et al. Predictor of early remission of diabetic macular edema under as-needed intravitreal ranibizumab. Sci Rep. 2019;9:7599.
Korobelnik JF, Do DV, Schmidt-Erfurth U, et al. Intravitreal aflibercept for diabetic macular edema. Ophthalmology. 2014;121:2247–54.
Kabir ER, Moreino SS, Sharif Siam MK. The breakthrough of biosimilars: a twist in the narrative of biological therapy. Biomolecules. 2019;9:410.
Elman MJ, Aiello LP, Beck RW, et al. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 2010;117:1064–77.
Herbaut A, Fajnkuchen F, Qu-Knafo L, et al. Switching to aflibercept in diabetic macular edema not responding to ranibizumab and/or intravitreal dexamethasone implant. J Ophthalmol. 2017;2017:8035013.
Bressler NM, Beaulieu WT, Glassman AR, et al. Persistent macular thickening following intravitreous aflibercept, bevacizumab, or ranibizumab for central-involved diabetic macular edema with vision impairment: a secondary analysis of a randomized clinical trial. JAMA Ophthalmol. 2018;136:257–69.
Gonzalez VH, Campbell J, Holekamp NM, et al. Early and long-term responses to anti-vascular endothelial growth factor therapy in diabetic macular edema: analysis of Protocol I data. Am J Ophthalmol. 2016;172:72–9.
Zarbin MA. Anti-VEGF agents and the risk of arteriothrombotic events. Asia Pac J Ophthalmol (Phila). 2018;7:63–7.
Ehlken C, Martin G, Stahl A, Agostini HT. Reduction of vascular endothelial growth factor a in human breast milk after intravitreal injection of bevacizumab but not ranibizumab. Arch Ophthalmol. 2012;130:1226–7.
Parodi MB, Bandello F. Is laser still important in diabetic macular edema as primary or deferral therapy. Dev Ophthalmol. 2017;60:125–30.
Whitcup SM, Robinson MR. Development of a dexamethasone intravitreal implant for the treatment of noninfectious posterior segment uveitis. Ann N Y Acad Sci. 2015;1358:1–12.
Chang-Lin JE, Attar M, Acheampong AA, et al. Pharmacokinetics and pharmacodynamics of a sustained-release dexamethasone intravitreal implant. Invest Ophthalmol Vis Sci. 2011;52:80–6.
Unsal E, Eltutar K, Sultan P, Erkul SO, Osmanbasoglu OA. Efficacy and safety of intravitreal dexamethasone implants for treatment of refractory diabetic macular edema. Korean J Ophthalmol. 2017;31:115–22.
Boyer DS, Yoon YH, Belfort R Jr, et al. Three-year, randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with diabetic macular edema. Ophthalmology. 2014;121:1904–14.
Nicolo M, Musetti D, Marenco M, et al. Real-life management of diabetic macular edema with dexamethasone intravitreal implant: a retrospective analysis of long-term clinical outcomes. J Ophthalmol. 2020;2020:4860743.
Dugel PU, Bandello F, Loewenstein A. Dexamethasone intravitreal implant in the treatment of diabetic macular edema. Clin Ophthalmol. 2015;9:1321–35.
Mehta H, Gillies M, Fraser-Bell S. Perspective on the role of Ozurdex (dexamethasone intravitreal implant) in the management of diabetic macular oedema. Ther Adv Chronic Dis. 2015;6:234–45.
Adan A, Cabrera F, Figueroa MS, et al. Clinical-decision criteria to identify recurrent diabetic macular edema patients suitable for fluocinolone acetonide implant therapy (ILUVIEN(®)) and follow-up considerations/recommendations. Clin Ophthalmol. 2020;14:2091–107.
Schwartz SG, Scott IU, Stewart MW, Flynn HW Jr. Update on corticosteroids for diabetic macular edema. Clin Ophthalmol. 2016;10:1723–30.
Chawan-Saad J, Wu M, Wu A, Wu L. Corticosteroids for diabetic macular edema. Taiwan J Ophthalmol. 2019;9:233–42.
Vaz-Pereira S, Castro-de-Sousa JP, Martins D, et al. The outcomes of switching from short- to long-term intravitreal corticosteroid implant therapy in patients with diabetic macular edema. Ophthalmic Res. 2020;63:114–21.
Zur D, Iglicki M, Busch C, et al. OCT biomarkers as functional outcome predictors in diabetic macular edema treated with dexamethasone implant. Ophthalmology. 2018;125:267–75.
Pouwels X, Petersohn S, Carrera VH, et al. Fluocinolone acetonide intravitreal implant for treating recurrent non-infectious uveitis: an evidence review group perspective of a NICE single technology appraisal. Pharmacoeconomics. 2020;38:431–41.
Lee DJ. Intraocular implants for the treatment of autoimmune uveitis. J Funct Biomater. 2015;6:650–66.
Maturi RK, Pollack A, Uy HS, et al. Intraocular pressure in patients with diabetic macular edema treated with dexamethasone intravitreal implant in the 3-year Mead study. Retina. 2016;36:1143–52.
Bahadorani S, Krambeer C, Wannamaker K, et al. The effects of repeated Ozurdex injections on ocular hypertension. Clin Ophthalmol. 2018;12:639–42.
Schmit-Eilenberger VK. A novel intravitreal fluocinolone acetonide implant (Iluvien(®)) in the treatment of patients with chronic diabetic macular edema that is insufficiently responsive to other medical treatment options: a case series. Clin Ophthalmol. 2015;9:801–11.
Al-Khersan H, Hariprasad SM, Salehi-Had H. Dexamethasone and anti-VEGF combination therapy for the treatment of diabetic macular edema. Ophthalmic Surg Lasers Imaging Retina. 2019;50:4–7.
Dehghan MH, Salehipour M, Naghib J, et al. Pars plana vitrectomy with internal limiting membrane peeling for refractory diffuse diabetic macular edema. J Ophthalmic Vis Res. 2010;5:162–7.
La Mantia A, Hawrami A, Laviers H, Patra S, Zambarakji H. Treatment of refractory diabetic macular edema with a fluocinolone acetonide implant in vitrectomized and non-vitrectomized eyes. Int J Ophthalmol. 2018;11:1951–6.
Gross JG, Glassman AR, Liu D, et al. Five-year outcomes of panretinal photocoagulation vs intravitreous ranibizumab for proliferative diabetic retinopathy: a randomized clinical trial. JAMA Ophthalmol. 2018;136:1138–48.
Chhablani J, Mathai A, Rani P, et al. Comparison of conventional pattern and novel navigated panretinal photocoagulation in proliferative diabetic retinopathy. Invest Ophthalmol Vis Sci. 2014;55:3432–8.
Boscia F, Giancipoli E, D’Amico Ricci G, Pinna A. Management of macular oedema in diabetic patients undergoing cataract surgery. Curr Opin Ophthalmol. 2017;28:23–8.
Baker CW, Almukhtar T, Bressler NM, et al. Macular edema after cataract surgery in eyes without preoperative central-involved diabetic macular edema. JAMA Ophthalmol. 2013;131:870–9.
Alnagdy AA, Abouelkheir HY, El-Khouly SE, Tarshouby SM. Impact of topical nonsteroidal anti-inflammatory drugs in prevention of macular edema following cataract surgery in diabetic patients. Int J Ophthalmol. 2018;11:616–22.
Russo A, Longo A, Avitabile T, et al. Incidence and risk factors for tractional macular detachment after anti-vascular endothelial growth factor agent pretreatment before vitrectomy for complicated proliferative diabetic retinopathy. J Clin Med. 2019;8(11):1960.
Kulikov AN, Sosnovskii SV, Berezin RD, et al. Vitreoretinal interface abnormalities in diabetic macular edema and effectiveness of anti-VEGF therapy: an optical coherence tomography study. Clin Ophthalmol. 2017;11:1995–2002.
Yamamoto T, Akabane N, Takeuchi S. Vitrectomy for diabetic macular edema: the role of posterior vitreous detachment and epimacular membrane. Am J Ophthalmol. 2001;132:369–77.
Yoo R, Kim HC, Chung H. Dexamethasone intravitreal implant for diabetic macular edema in a pregnant patient. Int J Ophthalmol. 2016;9:1524–7.
Akkaya S. Early miscarriage occurring six days after intravitreal ranibizumab injection. Med Hypothesis Discov Innov Ophthalmol. 2019;8:69–72.
Mansour SE, Browning DJ, Wong K, Flynn HW Jr, Bhavsar AR. The evolving treatment of diabetic retinopathy. Clin Ophthalmol. 2020;14:653–78.
Whitcup SM, Cidlowski JA, Csaky KG, Ambati J. Pharmacology of corticosteroids for diabetic macular edema. Invest Ophthalmol Vis Sci. 2018;59:1–12.
Sarao V, Veritti D, Boscia F, Lanzetta P. Intravitreal steroids for the treatment of retinal diseases. Sci World J. 2014;2014: 989501.
Zur D, Loewenstein A. Should we still be performing macular laser for non-centre involving diabetic macular oedema? Yes Eye. 2022;36:483–4.
Kamjoo S. Intravitreal injections. Am Acad Ophthalmol. 2020. https://eyewiki.aao.org/Intravitreal_Injections#Follow_up.
Nikkhah H, Karimi S, Ahmadieh H, et al. Intravitreal injection of anti-vascular endothelial growth factor agents for ocular vascular diseases: clinical practice guideline. J Ophthalmic Vis Res. 2018;13:158–69.
Berkelman RL, Holland BW, Anderson RL. Increased bactericidal activity of dilute preparations of povidone-iodine solutions. J Clin Microbiol. 1982;15:635–9.
Ferguson AW, Scott JA, McGavigan J, et al. Comparison of 5% povidone-iodine solution against 1% povidone-iodine solution in preoperative cataract surgery antisepsis: a prospective randomised double blind study. Br J Ophthalmol. 2003;87:163–7.
Friedman DA, Mason JO 3rd, Emond T, McGwin G Jr. Povidone-iodine contact time and lid speculum use during intravitreal injection. Retina. 2013;33:975–81.
Lau PE, Jenkins KS, Layton CJ. Current evidence for the prevention of endophthalmitis in anti-VEGF intravitreal injections. J Ophthalmol. 2018;2018:8567912.
Bloch SB, Larsen M. Translational public health care perspective: intravitreal treatment of neovascular age-related macular degeneration has revolutionized clinical ophthalmology. Acta Ophthalmol. 2015;93:103–4.
Royal College of Ophthalmology. Ophthalmic service guidance—intravitreal injection therapy. 2018. https://www.rcophth.ac.uk/wp-content/uploads/2018/02/Intravitreal-Injection-Therapy-August-2018-2.pdf.
Artiaga J. Intravitreal injection assistive devices. Am Acad Ophthalmol. 2020. https://eyewiki.aao.org/Intravitreal_Injection_Assistive_Devices.
McCannel CA. Meta-analysis of endophthalmitis after intravitreal injection of anti-vascular endothelial growth factor agents: causative organisms and possible prevention strategies. Retina. 2011;31:654–61.
Bande MF, Mansilla R, Pata MP, et al. Intravitreal injections of anti-VEGF agents and antibiotic prophylaxis for endophthalmitis: a systematic review and meta-analysis. Sci Rep. 2017;7:18088.
College of Optometrists. Endophthalmitis (post-operative) (exogenous endophthalmitis). 2020. https://www.college-optometrists.org/guidance/clinical-management-guidelines/endophthalmitis-post-operative.html.
Acknowledgements
Funding
These consensus guidelines were developed following two in-person meetings in Dubai in June 2019 and December 2019. Bayer funded the provision of the meeting rooms in Dubai, including food and beverages during the meeting, a medical writer to document the discussions, and also provided funding for the journal’s Rapid Service for the publication of this report. Honoraria/consultancy fees were not paid to any of the participants for attending the meetings. Bayer had no interference in the consensus development and did not have an input on the content.
Medical Writing, Editorial, and Other Assistance
Medical writing support provided by Sarah Feeny (Apothecom UK), was funded by Bayer AG.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors contributed to the development of the guidelines. The Society acknowledges the contribution of Prof. Emad Abboud in the revision of the guidelines.
Disclosures
All named authors confirm that they have no commercial or conflicts of interest in relation to this work to declare.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Al Qassimi, N., Kozak, I., Al Karam, M. et al. Management of Diabetic Macular Edema: Guidelines from the Emirates Society of Ophthalmology. Ophthalmol Ther 11, 1937–1950 (2022). https://doi.org/10.1007/s40123-022-00547-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00547-2