Abstract
Purpose
To evaluate the changes in intraocular pressure (IOP) after intravitreal injection of triamcinolone acetonide for the management of diabetic macular edema (DME).
Methods
The study design is a prospective, interventional, two-arm, dose–response study. Nineteen patients with bilateral DME were included, one eye for every patient underwent intravitreal injection of 4 mg triamcinolone acetonide (group A, 19 eyes), and the other eye of the same patient underwent intravitreal injection of 8 mg triamcinolone acetonide (group B, 19 eyes); the selection as to which eye was to receive either dose was random. The patients were followed up for 6 months after injection; complete ophthalmological examination and optical coherent topography were done.
Results
Intravitreal triamcinolone acetonide was effective in reduction of DME in group A in the first 3 months only, while in group B with high dose (8 mg) the improvement continued for 6 months after injection. Significant IOP rise was observed in both groups with an incidence of 68.1% and 73.7% in groups A and B, respectively. IOP-lowering drugs were used to control IOP; however, one patient in each group needed glaucoma filtration surgery in both eyes after intractable glaucoma with failure of medical treatment.
Conclusion
Although intravitreal injection of triamcinolone acetonide is very effective in managing DME and with lower cost than other modalities, the rise in IOP and the burden of glaucoma are major concerns. High corticosteroid responder is an individualized reaction irrespective of the intravitreal triamcinolone acetonide dose used.
Similar content being viewed by others
Introduction
Macular edema is a common cause of reduced vision in patients with diabetic retinopathy [1].
Many studies, including the Early Treatment Diabetic Retinopathy Study (ETDRS) have demonstrated that macular photocoagulation is effective for the treatment of macular edema but it does not usually restore vision loss occurring before treatment [2–4]. Laser photocoagulation, has a moderate effect in preventing further visual loss in about 50 of patients; however, some eyes need more intervention with intravitreal injections [2, 4].
Many investigations have reported the use of intravitreal triamcinolone acetonide (TA) for treatment of diffuse diabetic macular edema (DME) because of its effectiveness and low cost [5, 6]. The exact mechanism of effects is not known, but TA is presumed to diminish retinal leakage and reduce retinal thickening in the macula, leading to improved visual acuity [7].
Different doses varying from 1 to 25 mg TA have been employed so far [1]. Spandau et al. [1] reported that the efficacy of intravitreal TA was dose-dependent, and treatment response lasted longer, and was more pronounced with increasing dosage. However, the problem of intraocular pressure (IOP) changes with intravitreal TA is still a concern with its possible effects on vision. The current study investigates the efficacy and possible side effects of intravitreal TA in DME patients. So in this study, patients with bilateral DME refractory to laser treatment were included to receive intravitreal TA 4 mg in one eye and intravitreal TA 8 mg in the other eye.
Materials and Methods
This prospective interventional two-arm, dose–response study included 38 eyes (19 patients) of patients with DME, defined according to the Early Treatment Diabetic Retinopathy [2]. The patients were 17 females and 2 males; sample size was determined according to sample size formula which was 20 eyes per group and one patient lost during follow-up.
The present study included patients with bilateral advanced DME, 17 patients were females, and this high number of females was included in the study because they were housewives with very few outdoor activities, and they started to complain after the better eye started to deteriorate. On the contrary, most males had an outdoor activity and have high visual needs, so they complain and ask for management early.
Phakic patients with bilateral diffuse DME were included; all patients had diabetes for a duration of 15 years or more. All patients included had DME for a duration of 6 months or more. No cataract in the included eyes, some eyes had equatorial cortical faint cataracts which were not clinically significant. One eye received intravitreal TA 4 mg and the other eye of the same patient received intravitreal TA 8 mg. The selection as to which eye was to receive either dose was random and simple randomization was done by using a randomization table created by computer software (Random Allocation Software, Version 1.0, 2004; (Isfahan University of Medical Sciences, Isfahan, Iran). The interval between the intravitreal injections in both eyes of the same patient was 1 week.
All patients were fully informed about the risks and benefits of potential treatment, and all procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study. The inclusion criteria for the study eyes included the following: (1) best-corrected visual acuity letter score between 20/40 and 20/320; (2) definite retinal thickening resulting from DME on clinical examination involving the center of the macula assessed to be the main cause of visual loss; (3) retinal thickness measured with optical coherence tomography (OCT) of 250 ?m or more in the central subfield; and (4) grid laser treatment was done at least 3 months earlier.
Principal exclusion criteria included: (1) prior treatment with intravitreal corticosteroids (at any time), peribulbar steroid injection within the prior 6 months, or pars plana vitrectomy (at any time); (2) a history of glaucoma or steroid-induced IOP elevation that required IOP-lowering treatment; (3) average IOP of 23 mmHg or more after three preinjection evaluations; (4) eyes with ischemic maculopathy, and (5) patients with foveal traction detected with OCT.
Assessment of DME was based on ophthalmoscopic examination, fluorescein angiography and OCT of the macula.
The study was carried out between March 2010 and March 2012.
Technique of Intravitreal Injection of TA
Intravitreal injections were done in the operating room, eyelids and eyelashes were scraped with 10% povidone iodine, and a sterile eye speculum was placed. Ocular surface was sterilized by 5% povidone iodine. After installation of topical benoxinate hydrochloride drops, a cotton-tipped swab soaked with benoxinate hydrochloride was pressed against the injection site for 10–20 s to anaesthetize the injection site. Paracentesis was done first to decrease IOP and to help the vitreous to accommodate all injected TA. By using a 27G needle, 4 mg (0.1 ml) of TA (the vial containing 40 mg of TA in 1 ml) was injected into the vitreous cavity through the lower temporal pars plana (Group A) 4 mm away from the limbus. Group B received 8 mg (0.2 ml) with the same technique. A cotton-tipped swab was pressed against the injection site to force the closure of the needle tract. The eye was bandaged for 4 h. The operative steps were done according to Bae et al. [8].
Topical moxifloxacin eyedrops were used in patients for 3 days. Patients were examined the next day and next week for visual acuity (VA), IOP measurement, and possible complications following the steroid injection. The examination was repeated weekly during the first month and then monthly if there were no complications; the examiner was masked to the treatment protocol. Visual acuity (VA) measurements were done with Snellen visual acuity chart and were converted to the logarithm of the minimum angle of resolution (log MAR) for statistical analysis. OCT was performed using the Rtvue Fourier-domain OCT (Optovue, Inc, Fremont, USA). OCT was done before injection, 1, 3, and 6 months after injection.
No repeat injection was done to the eyes during follow-up period (6 months) and no other ocular treatment of diabetic retinopathy was used.
Persistent macular edema was defined as ongoing macular edema that did not change or increase within 3 months following TA injection.
On follow-up, an IOP range of 10–22 mmHg was considered to be within the normal range.
If the patient had an IOP of 23–30 mmHg, beta blockers (Levobunolol hydrochloride) were used.
If IOP was between 30 and 40 mmHg, a combination of timolol maleate and dorzolamide hydrochloride and brimonidine tartrate was used.
If IOP was above 40 mmHg, a combination of travoprost, brimonidine tartrate and timolol maleate and dorzolamide hydrochloride was used with or without systemic acetazolamide.
If IOP was still high (above 22 mmHg) despite maximum medical treatment, trabeculectomy was done as TA induced glaucoma through extracellular matrix deposition in the trabecular meshwork [9].
Statistical Analysis
Collected data were coded, entered, and analyzed using Microsoft Excel software 2010 (Microsoft®; Michigan, USA). Data were then imported into Statistical Package for the Social Sciences (SPSS version 16.0, University of Washington, Seattle, USA) software for analysis. Baseline characteristics of the study population were presented as frequencies and percentages (%) in qualitative data or mean values and standard deviations (SD) in quantitative data. Differences between frequencies were compared by Chi-square. Differences between means were compared by Wilcoxon rank-sum test. P value of <0.05 was considered significant. Pearson correlation coefficient test was used to evaluate the correlations between the studied variables. Analysis of variance (ANOVA) test was performed for repeated measures which indicated the F value in tables.
Results
Nineteen patients were included in this study (17 women and 2 men) and both eyes had advanced DME.
The mean age of patients was 52.32 years ±11.39.
There were no differences in preoperative visual acuity and OCT findings between the eyes treated with 4 or 8 mg TA.
The primary measure of efficacy of intravitreal injection was VA, an outcome of high importance to patients. VA was measured with Snellen visual acuity chart and it was converted to log MAR for statistical analysis, the mean of VA was 1.19 ± 0.15, 1.14 ± 0.16 (log MAR) in groups A and B, respectively, before injection. Vision improved after injection with a mean 0.72 ± 0.13, 0.69 ± 0.17 in groups A and B, respectively, after 3 months of the injection. After 6 months the mean was 0.89 ± 0.23, 0.68 ± 0.19 in groups A and B, respectively (Table 1), and this difference between groups was statistically significant only at 6 months evaluation, P < 0.004 (Fig. 1).
The mean values of foveal thickness as measured by OCT were 522 ± 43 and 518 ± 53 ?m in groups A and B, respectively, before injection. One month after injection foveal thickness decreased with mean values of 334 ± 54 and 322 ± 51 ?m in groups A and B, respectively, and this improvement extended to a period of 3 months (Table 2), and at 6 months the mean values were 467 ± 64 and 344 ± 56 ?m in groups A and B, respectively, which means that the improvement was maintained in group B than in group A. This difference between groups was statistically significant only at 6 months evaluation (Fig. 2).
The mean values of IOP before injection were 14 ± 3.3 and 14 ± 2.9 mmHg in groups A and B, respectively. One month after injection the mean was 24 ± 5.3 and 25 ± 4.3 mmHg in groups A and B, respectively; the mean values of IOP never returned to preinjection level, and at 6 months after injection the mean values were 19 ± 6.2 and 20 ± 5.2 mmHg in groups A and B, respectively. The differences in the mean values of IOP before injection and post injection were statistically significant at all follow-up evaluations (Table 3).
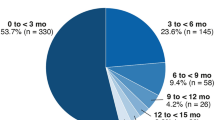
The rise in IOP had occurred in 13 eyes in group A and in 14 eyes in group B, while 6 eyes in group A and 5 eyes in group B maintained IOP within normal range without medications; the rise in IOP in both groups had occurred mainly in the third and fourth weeks after injection. During the third week, 76.9% of elevations of IOP occurred in group A and 69.23% of elevations of IOP occurred in group B (Table 4).
IOP-Lowering Drugs
No IOP-lowering drugs were needed in six eyes in group A and five eyes in group B after injection, while seven eyes in group A and eight eyes in group B needed one IOP-lowering drug.
There were two eyes in group A and one eye in group B that needed two types of eyedrops to control IOP; eyedrops used were timolol and dorzolamide and brimonidine tartrate ophthalmic solution (Table 5).
There were two eyes in group A and three eyes in group B that needed maximum medical treatment to control IOP (both eyes of two patients irrespective of intravitreal dose injected underwent high IOP rise and needed maximum medical treatment to control IOP).
Both eyes of the other two patients who received intravitreal injection in both eyes developed intractable glaucoma. They received maximum medical treatment but IOP was never controlled. Both patients underwent trabeculectomy in both eyes although one eye received 4 mg injection and the other eye of the same patient received 8 mg injection; however, the severity of the rise in IOP was the same irrespective of the dose injected (Table 5). IOP was controlled after surgical intervention.
Other Ocular Complications
Regarding ocular complications related to intravitreal injection there were no eyes with retinal detachment, vitreous hemorrhage, intraocular reaction or endophthalmitis. Only one eye in group B developed posterior subcapsular cataract.
Discussion
DME is one of the most common reasons for reduced vision in patients with diabetic retinopathy, Argon laser treatment is still the gold standard for management of DME. Some eyes, however, need more intervention with intravitreal injections [1].
Due to its effectiveness, availability, and low cost, intravitreal injection of TA is a common management of DME. The exact mechanism of action of corticosteroids is still unknown. The rationale, however, could be found in the ability of corticosteroids to inhibit the arachidonic acid pathway, of which prostaglandin is a product. Moreover, steroids may also down regulate the production of vascular endothelial growth factor, a known vascular permeability factor [10].
The included eyes in the study had no control group, and there were active interventions in both eyes, and this is because in advanced DME, leaving the patient just under observation is not acceptable.
Intravitreal injections might be useful for the treatment of diffuse DME. In fact this kind of edema has a poor prognosis with laser photocoagulation; other treatments like vitrectomy are not always followed by improvement in visual function and require a significant surgical intervention with its inherent risk, recovery time, and expense [11].
There was a significant improvement of VA at 1 and 3 months post injection in both groups’ evaluation, and at 6 months group B still showed marked improvement of visual acuity compared to group A. So the duration of the effect of intravitreal TA increased significantly with increasing dosage.
Foveal thickness was measured with OCT. There was marked reduction in foveal thickness and reduction of DME. The effect was maintained in both groups during the first 3 months with comparable results, but at 6 months evaluations the mean foveal thickness was less in group B, and the level of foveal thickness increased again in group A. This difference was statistically significant at 6 months evaluation (Fig. 2). Most literature stated that 4 mg intravitreal TA was effective for 3 months only and this was also seen in the current study [7, 8]. But in group B with high dose 8 mg TA the improvement continued for 6 months after injection, and this is in agreement with previous studies that used higher doses of intravitreal TA up to 25 mg [10–13].
The incidence in rise in IOP in group A was 68.1%, and 73.7% in group B, and these results are relatively high, and it may be a racial response to triamcinolone administration among Egyptians. However, the rate of increase of IOP in previous studies with intravitreal TA ranged from 20 to 80% [11, 14].
The time of the onset of rise in IOP was mainly during the first month after injection with a peak at the third week. In group A, 76.9% of IOP rise had occurred in the third week, while in group B, 64.3% of rise occurred in the same period (Table 4). By the end of the first month, all rises in IOP had occurred in Group A. In group B, 92.9% of rise had occurred in the first month, so it is mandatory to wait for 1 month after intravitreal injection of TA before the fellow eye is injected in cases of bilateral severe DME.
The rise in IOP was marked in both groups and two or more IOP-lowering medications were needed in 21% and 21.2% in groups A and B, respectively.
Two eyes in group A and two eyes in group B required glaucoma surgery after failure of maximum tolerated medical treatment, the IOP in such eyes remained between 40 and 50 mmHg despite the medical treatment so trabeculectomy was done in these four eyes. These four eyes of intractable glaucoma belonged to two patients (intractable glaucoma occurred in both eyes of the same patients) and so the IOP rise response was the same irrespective of intravitreal dose of TA used.
Also two other patients needed three anti-glaucoma medications to control IOP irrespective of intravitreal TA doses used (both eyes of two patients) (Table 3). So, the high corticosteroid responder was the same irrespective of intravitreal TA dose injected. This also confirms that there is individual variation in response to TA but if there is severe glaucoma in one eye then the same will occur in the other eye irrespective of the dose used.
Regarding side effects, none of the study groups showed an infectious or sterile endophthalmitis, pseudo-endophthalmitis and only one eye in group B showed the development of posterior subcapsular cataract.
The rationale of using relatively high intravitreal TA (8 mg) was to maintain improvements in vision for longer duration lower the frequency of reinjection with its psychological and financial burden and minimize the possibility of injection associated complications such as endophthalmitis.
On the other hand the intravitreal use of Ranibizumab is a standard treatment for DME; however, it is costly and in such cases, needs repeated monthly injections. Our patients were unable to take such medications because of low socioeconomic state and lack of insurance cover.
A significant rise in the serum concentration of corticosteroids was not detected after an intravitreal injection of even with high doses (20–25 mg) TA, meaning that it is safe to inject intravitreal TA to diabetic patients on the other hand injection of different dose to each eye will not be interfered by the other eye through systemic circulation [15].
However, the problem of IOP rise is still a major concern, although it is treatable it may require the patient to undergo glaucoma surgery to control it. Based on these findings, it is necessary for the provider to engage the patient in the plan of management regarding risks and benefits of potential treatment. The decision to undergo intravitreal TA treatment should reflect the patients’ personal values and preferences and should be made only after the patients are equipped with sufficient information to make an informed choice about their care.
The high rise in IOP in response to intravitreal TA may be a racial response and because of limited sample size, multinational study may be needed to determine the benefits and side effects of TA injection in management of DME.
Conclusion
Intravitreal injection of TA is effective in reduction of DME and the duration of improvement increases with higher dose injected (8 mg). However, IOP rise is a major concern as many eyes needed anti-glaucoma drugs and even glaucoma surgery and such patients need close follow-up to treat any possible complications.
References
Spandau UHM, Derse M, Schmitz-Valckenberg P, et al. Dosage dependency of intravitreal triamcinolone acetonide as treatment for diabetic macular oedema. Br J Ophthalmol. 2005;89:999–1003.
Early Treatment Diabetic Retinopathy Study Research Group. Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Arch Ophthalmol. 1985, 103:1796–806.
Aiello LM. Perspectives on diabetic retinopathy. Am J Ophthalmol. 2003;136:122–35.
Akduman L, Olk RJ. Laser photocoagulation of diabetic macular edema. Ophthalmic Surg Lasers. 1997;28:387–408.
Jonas JB, Hayler JK, Söfker A, et al. Intravitreal injection of crystalline cortisone as adjunctive treatment of proliferative diabetic retinopathy. Am J Ophthalmol. 2001;131:468–71.
Jonas JB, Söfker A. Intraocular injection of crystalline cortisone as adjunctive treatment of diabetic macular edema. Am J Ophthalmol. 2001;132:425–7.
Wilson CA, Berkowitz BA, Sato Y, et al. Treatment with intravitreal steroid reduces blood retinal barrier breakdown due to retinal photocoagulation. Arch Ophthalmol. 1992;110:1155–9.
Bae JS, Park SJ, Ham IR, Lee TG. Dose dependent effects of intravitreal triamcinolone acetonide on diffuse diabetic macular edema. Korean J Ophthalmol. 2009;23:80–5.
Kubota T, Okabe H, Hisatomi T, Yamakiri K, Sakamoto T. Tawara: A Ultrastructure of the trabecular meshwork in secondary glaucoma eyes after intravitreal triamcinolone acetonide. J Glaucoma. 2006;15:117–9.
Grenga P, Lupo S, Domanico D, et al. Efficacy of intravitreal triamcinolone acetonide in long standing diabetic macular edema: a microperimetry and optical coherence tomography study. Retina. 2008;28:1270–5.
Wingate RJ, Beaumont PE. Intravitreal triamcinolone and elevated intraocular pressure. Aust N Z J Ophthalmol. 1999;27:431–2.
Jonas JB, Spandau UH, Kamppeter BA, et al. Repeated intravitreal high-dosage injections of triamcinolone acetonide for diffuse diabetic macular edema. Ophthalmology. 2006;113:800–4.
Ghoneim E, Abd El Ghany A. Evaluation of intravitreal triamcinolone acetonide 4 mg versus 8 mg for the management of diabetic macular edema refractory to laser photocoagulation. Egypt Ophthalmol Soc. 2011;104:211–5.
Smithen LM, Ober MD, Maranan L, et al. Intravitreal triamcinolone acetonide and intraocular pressure. Am J Ophthalmol. 2004;138:740–3.
Degenring RF, Jonas JB. Serum levels of triamcinolone acetonide after intravitreal injection. Am J Ophthalmol. 2004;137:1142–3.
Acknowledgments
General support by departmental chair Professor Hussin El-Nahhas, Head of the Ophthalmology Department, Suez Canal University, Egypt. Dr. Mona Farg and Dr. Alaa Ghomaa for their help in assessment of patients and OCT investigations. Thanks to Dr. Ahmed Maaty, Department of Epidemiology, for his help. Dr. Ghoneim is the guarantor for this article, and takes responsibility for the integrity of the work as a whole. No funding or sponsorship was received for this study or publication of this article.
Conflict of interest
Dr. Ghoneim and Dr. Ahmed A. Abd El Ghany declare no conflict of interest.
Compliance with Ethics Guidelines
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
Australian New Zealand Clinical Trials Registry (ANZCTR) #ACTRN12613000014752.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Ghoneim, E.M., Abd El Ghany, A.A. Behavior of Intraocular Pressure After Intravitreal Injection of Triamcinolone Acetonide Among Egyptians. Ophthalmol Ther 2, 121–130 (2013). https://doi.org/10.1007/s40123-013-0017-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-013-0017-0