Abstract
Stigma is defined by the World Health Organization (WHO) as “a mark of shame, disgrace or disapproval that results in an individual being rejected, discriminated against and excluded from participating in a number of different areas of society”. Extensive literature searches have documented stigma in the context of health. Among the physical health conditions that are associated with stigma, chronic pain deserves particular attention. Stigma experienced by individuals with chronic pain affects their entire life. Literature identifies multiple dimensions or types of stigma, including public stigma, structural stigma and internalized stigma. Recent literature supports the biopsychosocial model of pain, according to which biological, psychological and sociocultural variables interact in a dynamic manner to shape an individual’s response to chronic pain. Chronic pain affects a higher proportion of women than men around the world. There is an inadequate education of health care professionals regarding pain assessment and their insecurity to manage patients with chronic pain. A first-line intervention strategy could be to promote pain education and to expand knowledge and assessment of chronic pain, as recently highlighted for headache disorders, paradigmatically for resistant or refractory migraine, whose diagnosis, without an adequate education to understand the possible fluctuations of the disease, may have profound psychological implications with the idea of insolvability and contribute to stigmatizing the patient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Definition of Stigma
Stigma is defined by the World Health Organisation (WHO) as “a mark of shame, disgrace or disapproval that results in an individual being rejected, discriminated against and excluded from participating in a number of different areas of society” [1]. This definition has its roots in the classical conceptualisation of stigma given in 1963 by the Canadian sociologist Erving Goffman, who defined stigma as an “attribute that is deeply discrediting”, the “situation of the individual who is disqualified from full social acceptance” [2]. In the wake of Goffman but focusing on the power relations in society [3], Link and Phelan conceptualise stigma as the co-occurrence of four components: (1) the distinguishing and labelling of human differences; (2) the association of human difference with negative attributes; (3) the separation of “us” from “them”; (4) status loss and discrimination against those labeled [4]. The concept of stigma thus becomes closely related to the social consequences of the identification and labelling of the “other” in terms of creation of social inequalities such as disapproval, rejection, exclusion and discrimination [5].
Stigma and Health Conditions
Extensive literature searches have documented stigma in the context of health [6]. Examples of mental and physical health conditions that are commonly stigmatised include major depression [7], schizophrenia [8], epilepsy [9], HIV/AIDS [10], tuberculosis [11], obesity [12] and chronic pain [13]. Experiencing stigma for having a particular health condition is a pervasive barrier interfering with patient health. In fact, individuals with stigmatised health conditions tend to avoid treatment [14] and to have poor treatment outcomes, decreased social opportunities [15], difficulty in obtaining employment [16] and a decreased overall quality of life [14].
Definition of Chronic Pain
Among the physical health conditions that are associated with stigma, chronic pain deserves particular attention. Chronic pain is one of the most common reasons people seek medical care [17] and is a leading source of human suffering and disability in the world [18]. Recently, the WHO, in collaboration with the International Association for the Study of Pain (IASP), has proposed a new definition of “chronic pain”, updating the International Classification of Diseases (ICD-11), to focus on chronic pain as a global health priority [19]. Chronic pain is defined as persistent or recurrent pain lasting > 3 months and it affects > 30% of people worldwide [20]. Examples of chronic primary pain conditions include fibromyalgia, complex regional pain syndrome, chronic migraine, temporomandibular disorder, irritable bowel syndrome and non-specific low-back and neck pain.
Stigma and Chronic Pain
Individuals affected by chronic pain are vulnerable to stigmatising the reaction of others: “Pain is all in your head”, “You must be crazy”, “If you look healthy, you cannot be in pain”, “You must have complete control over everything in your life”, “You just want attention”, “It’s just anxiety”, and “It must be nice to not work” are just some of the stigmatising sentences aimed to people with chronic pain.
Several factors contribute to chronic pain-related stigma: the absence of clear medical evidence such as clear tissue damage, which does not fit with the largely accepted biomedical model [13], the invisibility of pain symptoms as well as the subjectivity of pain assessment [21]. Among chronic pain conditions, migraine stigma has been one of the most durable and remarkably stable over time [22].
Impact of Stigma on the Public Life of Individuals with Chronic Pain
Stigma experienced by individuals with chronic pain affects their entire life. It influences their social relationships because they do not feel understood by relatives, romantic partners and friends [5, 13, 23].
Stigma matters also in clinical settings, causing underassessment and underestimation of pain by health care staff [24], with scepticism and suspicion about the reality of suffering, tendency to attribute lower pain in ratings [13, 25, 26] and consequent undertreatment and overpsychologisation of pain [27]. Even dismissal in clinical settings has been reported by patients [28].
Stigma is also experienced in the workplace [13]. Patients perceive unfriendliness and antagonism from their fellow workers [23], and they can continue to work while sick, a phenomenon known as presenteeism—resulting in a decline in productivity and efficiency in addition to poor well-being [29, 30]. Moreover, in turn, the resulting distress can lead to sickness absence and burnout [31]. In particular, migraine, whose prevalence estimates increased over the years [32], is the most common cause of lost work time due to disability in the world among people < 50 years of age, with substantial losses in productivity and employer cost [33, 34]: for instance, in Japan the estimated cost of productivity loss associated with presenteeism has been calculated at 21.3 billion US$/year, while the annual economic loss due to absenteeism has been calculated to be US$ 2.7 billion [33]. Furthermore, missed and lost productive days per year for individuals with frequent migraine attacks have been estimated to be 2 days and 46 days, respectively, accounting for approximately 20% of the work year, while for individuals with chronic migraine (> 15 headache days per month) the estimated number of days per year missing from work and with reduced productivity are 3.5 days and 87 days, respectively, accounting for 38% of the work year [33].
Impact of Stigma on Personal Well-Being of Individuals with Chronic Pain
Stigma of chronic pain is therefore pervasive, weaving its way in multiple dimensions of life.
Its impact on personal well-being is very variable [13]. Some individuals are more resilient and seem not to be affected [13, 35], while others show psychological distress, especially those with chronic musculoskeletal pain in head and neck regions [36], depressive symptoms, social withdrawal, decline in self-esteem, failed attempts at self-realisation and insomnia [24, 37, 38]. Moreover, individuals with chronic pain are twice as likely to report suicidal behaviours or to complete suicide, and according to a recent review, chronic pain itself is an important independent risk factor for suicidality, in addition to depressive symptoms and other general risk factors [39] associated with higher lethality [40]: so it is extremely important for clinicians to provide an in-depth investigation into the suicidal mind, an assessment in addition to the psychiatric evaluation, adopting a phenomenological approach [41].
Types of Stigma
In accordance with Corrigan's progressive model of self-stigma, the stigmatising attitudes and reactions of others have a detrimental impact on personal well-being only when a series of stages, namely “awareness, agreement and application” of these stigmatising attitudes, occur in the self [13, 42, 43].
Literature identifies in fact multiple dimensions or types of stigma, including public stigma, structural stigma and internalised stigma.
Public stigma refers to negative attitudes and stereotypes circulating in the general public [30, 44].
Structural stigma refers to an organisation’s policies or culture of negative attitudes and beliefs toward stigmatised individuals [45].
Finally, internalised or self-stigma can be described as a process whereby affected individuals absorb negative stereotypes, considering them self-relevant, and anticipate social rejection [16, 46,47,48].
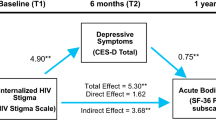
Stigma is internalised by a large percentage of people living with chronic pain. Specifically, a study conducted by Waugh et al. [37] reported that 38% of people affected by chronic pain endorsed the experience of internalised stigma, including alienation, social withdrawal and discriminatory experiences based on pain. This proportion is comparable to levels observed in the mental health literature [37, 48, 49]. The study showed that internalised stigma has a negative relationship with self-esteem and pain self-efficacy. In fact, individuals with chronic pain who experience internalised stigma may anticipate devaluation and discrimination and adopt avoidance coping behaviours such as social withdrawal, resulting in decreased sense of hope and self-esteem [50]. This state of devaluation and demoralisation may in turn make people reluctant to approach life goals and engage in satisfying and rewarding activities despite their pain [42].
Furthermore, internalised stigma was associated with cognitive functioning in relation to pain in terms of a greater tendency to catastrophise about pain and a lower perception of personal control over pain [37]. Several studies have demonstrated that catastrophic thinking in relation to pain affects long-term disability and represents a psychological barrier to recovery: it is a risk factor for pain condition’s persistence, higher reported pain levels, medication overuse and longer length of hospital stay [51, 52]. Therefore, in the context of these finding, internalised stigma represents a potentially important area to enhance our understanding and to treat individuals with chronic pain through cognitive restructuring techniques [37].
Internalised Stigma and the Biopsychosocial Model of Pain
The findings of the study by Waugh et al. [37] support the biopsychosocial model of pain, according to which biological, psychological and sociocultural variables interact in a dynamic manner to shape an individual’s response to chronic pain [53, 54].
Internalised stigma is in fact a sociocultural construct derived from the endorsement of attitudes, judgements and reactions of other people about pain through interactions with family and friends, healthcare professionals and work colleagues. This in turn affects individual’s psychology, decreasing self-esteem and self-efficacy, influencing cognitive processes in relation to pain and shaping individual’s behaviour. Therefore, there is a reciprocal and dynamic interaction between social and psychological variables in the experience of pain.
Gender Gap Pain
The biopsychosocial model can also be used as an explanatory framework to understand the “gender pain gap”.
Chronic pain affects a higher proportion of women than men around the world [55,56,57,58]. Women are at greater risk for several chronic painful disorders, such as fibromyalgia, temporomandibular disorders, migraine headache, interstitial cystitis, joint pain, irritable bowel syndrome, complex regional pain syndrome and trigeminal neuralgia [59]. The reasons for this are complex, but there are convincing findings that both biological and psychosocial factors play important and interacting roles [55]. Biological factors include differences in sex-hormone production, anatomy, neuromuscular control and inflammatory responses that in turn cause differences in processing, modulation and inhibition of painful stimuli and in response to opioids [60]. Nevertheless, studies show that psychosocial factors exert a greater influence. Expression of pain and behavioural responses to perceived pain are influenced by gender and reflect societal norms [60]. Men are expected to be stoic, in control, tolerating pain and avoiding seeking health care, whereas women are presented as being more emotionally vulnerable, more sensitive to pain and more willing to report pain [56, 61]. Therefore, it is more accepted for women to show pain and men with chronic pain risk being perceived as more feminine than the typical man [62].
These factors may explain why more women are diagnosed with chronic pain syndromes. Yet, paradoxically, studies show that female patients are taken less seriously by health-care providers, their pain is psychologised, they receive less adequate pain medication and more antidepressants compared to men, and they are more likely to report medication overuse headache (MOH), which is three times more common in women than in men [63,64,65,66,67]. Therefore, chronic pain in female patients is more stigmatised. Several studies showed that women with chronic pain are often perceived as hysterical, emotional, complaining, not wanting to get better, malingerers and fabricating the pain, as if it is all in their heads, and they are assigned psychological rather than somatic causes for their pain [56]. This apparent paradox, in which more women than men suffer from chronic pain but many remain under-diagnosed and inadequately treated, reflects the current state of our healthcare, in line to the hegemonic masculinity and andronormativity of our society [56]. Moreover, there is behavioural and electrophysiological evidence that sexism-related stigma increases female individuals’ pain perception, thus creating a vicious circle [68].
Causes and Mechanisms of Chronic Pain-Related Stigma
As widely discussed, stigma has a great impact on well-being of individuals living with chronic pain and existing studies tend to focus on it. Conversely, little work has considered causes and mechanisms of stigma. In their Topical Review, De Ruddere and Craig proposed some potential mechanisms underlying the stigmatising responses of observers towards individuals living with chronic pain [13].
First, reactions to people in pain depend on input from the individual in pain (“bottom up” sources). While acute pain evokes spontaneous facial expressions, nociceptive reflexive withdrawal or nonverbal vocalisations, chronic pain expression is less likely to be automatic or reflexive and, especially in contexts of the commonplace, the absence of automatic pain behaviour could make people suspicious of the credibility of the pain.
Moreover, reactions to people in pain are determined by “top-down” factors, such as personal belief and attitudes. From an evolutionary perspective, stigmatising behaviour could be explained because of the tendency of people to value others as contributing to their personal well-being and the good of the community and to be suspicious of possible freeloaders, those who take a common good without earning or deserving it [13, 24, 69,70,71]. In the context of chronic pain, the lack of clear tissue damage, in contrast with the widely held biomedical model, makes people doubt the authenticity and the trustworthiness of individuals with pain [72]. Additionally, it has been demonstrated being part of a social “out group”, such as people with a different skin colour, raises suspiciousness. This suspiciousness is reported be higher toward members of social out-groups [73, 74].
Another potential mechanism underlying the observer stigmatising responses arises from the causal attribution theory, which is the process of trying to determine the causes of people's behaviour. In the context of chronic pain, people tend to reward and punish other people if they perceive them to be responsible for their pain condition.
Finally, reactions to people in pain can be determined by the fact that health care professionals often do not receive adequate education regarding pain assessment and feel uncertain about managing patients with chronic pain [75, 76]. A recent systematic review on patients’ perceptions of prescription opioids, commonly prescribed in chronic pain, revealed a certain unease of health care professionals about prescribing and discussing opioids with patients [77].
Intervention Strategies to Reduce Chronic Pain-Related Stigma
In addition to focusing on underlying mechanisms in observer stigmatising responses, De Ruddere and Craig, in their Topical Review, dealt with intervention strategies to address stigma at different levels: intrapersonal, interpersonal and structural [13]. The intrapersonal level describes interventions directed at individuals to enhance resilience and coping strategies through emotion regulation and enhanced psychological flexibility in people with chronic pain and to help them to overcome stigma-related cognitive and emotional distress [13, 24, 78]. The interpersonal level describes interventions directed at small-group interactions (e.g., promoting less prejudicial manners of social interaction). The structural level describes interventions directed at the social-political environment, such as laws and policies.
Pain Education and the Biopsychosocial Model
Considering the above-mentioned inadequate education of health care professionals regarding pain assessment and their insecurity to manage patients with chronic pain, a first-line intervention strategy could be to promote pain education [75] and to expand knowledge and assessment of chronic pain, as recently highlighted for headache disorders [79, 80], especially for resistant or refractory migraine, whose diagnosis, without an adequate education to understand the possible fluctuations of the disease, may have profound psychological implications with the idea of unsolvability and contribute to stigmatising the patient [81, 82]. Nonetheless, this would also imply overcoming deeply rooted prejudices, behaviours and values embedded in our society and reversing Eccleston’s “analgesic culture” [24, 83], characterised by “the dominant belief that pain should be short-lived, diagnostically meaningful, and denote a fixable problem”. Because of its persistent condition and diagnostic uncertainty, chronic pain does not fit this model. Likewise, the absence of clear medical tissue damage does not fit with the narrow biomedical perspective on acute pain [84] which presupposes a clear pathophysiology to explain the pain experience and is focused on tissue damage and nociceptive afferent systems. Even the models proposed by psychology were found to be inadequate and often stigmatising [85].
The limits of models adopted so far compel transition to a more comprehensive and holistic model, like the biopsychosocial one, as previously discussed. This model includes the role of the central nervous system and neuroplasticity as biological substrates of the cognitive and affective processes of chronic pain [86] and integrates them with psychological and sociocultural variables that interact in a dynamic manner to shape an individual’s response to chronic pain.
A broader understanding of the processes involved in chronic pain and its transmission in clinical settings and in the wider community would contribute to reduce the stigma attached to individuals living with chronic pain.
References
World Health Organization. The World Health Report: mental health: new understanding. New Hope: World Health Organization; 2001.
Gofman E. Stigma: notes on the management of spoiled identity. New York: Simon & Schuster, Inc.; 1963.
Clair M. Stigma. Core concepts in sociology. New Jersey:Wiley-Blackwell; 2018. ISBN:978-1-119-16862-1.
Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. 2001;27(1):363–85.
Naushad N, Dunn LB, Muñoz RF, Leykin Y. Depression increases subjective stigma of chronic pain. J Affect Disord. 2018;15(229):456–62.
Weiss M, Ramakrishna J. Stigma interventions and research for international health. Lancet. 2006;367:536–8.
Yokoya S, Maeno T, Sakamoto N, Goto R, Maeno T. A brief survey of public knowledge and stigma towards depression. J Clin Med Res. 2018;10(3):202–9.
van Zelst C. Stigmatization as an environmental risk in schizophrenia: a user perspective. Schizophr Bull. 2009;35(2):293–6.
Fiest KM, Birbeck GL, Jacoby A, Jette N. Stigma in epilepsy. Curr Neurol Neurosci Rep. 2014;14(5):444.
Sweileh WM. Bibliometric analysis of literature in AIDS-related stigma and discrimination. Transl Behav Med. 2019;9(4):617–28.
Juniarti N, Evans D. A qualitative review: the stigma of tuberculosis. J Clin Nurs. 2011;20(13–14):1961–70.
Hill B, Bergmeier H, Incollingo Rodriguez AC, Barlow FK, Chung A, Ramachandran D, Savaglio M, Skouteris H. Weight stigma and obesity-related policies: a systematic review of the state of the literature. Obes Rev. 2021;22(11): e13333.
De Ruddere L, Craig KD. Understanding stigma and chronic pain: a-state-of-the-art review. Pain. 2016;157(8):1607–10.
Earnshaw VA, Quinn DM. The impact of stigma in healthcare on people living with chronic illnesses. J Health Psychol. 2012;17(2):157–68.
Corrigan P. How stigma interferes with mental health care. Am Psychol. 2004;59(7):614–25.
Picco L, Pang S, Lau YW, Jeyagurunathan A, Satghare P, Abdin E, Vaingankar JA, Lim S, Poh CL, Chong SA, Subramaniam M. Internalized stigma among psychiatric outpatients: Associations with quality of life, functioning, hope and self-esteem. Psychiatry Res. 2016;30(246):500–6.
Mäntyselkä P, Kumpusalo E, Ahonen R, Kumpusalo A, Kauhanen J, Viinamäki H, Halonen P, Takala J. Pain as a reason to visit the doctor: a study in Finnish primary health care. Pain. 2001;89:175–80.
Goldberg DS, McGee SJ. Pain as a global public health priority. BMC Public Health. 2011;11:770.
Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, Cohen M, Evers S, Finnerup NB, First MB, Giamberardino MA. Chronic pain as a symptom or a disease: the IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain. 2019;160(1):19–27.
Cohen SP, Vase L, Hooten WM. Chronic pain: an update on burden, best practices, and new advances. Lancet. 2021;397(10289):2082–97.
Wakefield EO, Zempsky WT, Puhl RM, Litt MD. Conceptualizing pain-related stigma in adolescent chronic pain: a literature review and preliminary focus group findings. Pain Rep. 2018;3(Suppl 1): e679.
Best RK, Alina A-K. Stigma's uneven decline. SocArXiv. 2022. https://doi.org/10.31235/osf.io/7nm9x.
Holloway I, Sofaer-Bennett B, Walker J. The stigmatisation of people with chronic back pain. Disabil Rehabil. 2007;29(18):1456–64.
Williams AC. Defeating the stigma of chronic pain. Pain. 2016;157(8):1581–2.
Tait RC, Chibnall JT. Physician judgments of chronic pain patients. Soc Sci Med. 1997;45(8):1199–205.
Taylor AG, Skelton JA, Butcher J. Duration of pain condition and physical pathology as determinants of nurses’ assessments of patients in pain. Nurs Res. 1984;33(1):4–8.
Tait RC, Chibnall JT, Kalauokalani D. Provider judgments of patients in pain: Seeking symptom certainty. Pain Med. 2009;10(1):11–34.
de Williams CAC, Cella M. Medically unexplained symptoms and pain: misunderstanding and myth. Curr Opin Support Palliat Care. 2012;6(2):201–6.
Allen D, Hines EW, Pazdernik V, Konecny LT, Breitenbach E. Four-year review of presenteeism data among employees of a large United States health care system: a retrospective prevalence study. Hum Resour Health. 2018;16(1):59.
Parikh SK, Kempner J, Young WB. Stigma and migraine: developing effective interventions. Curr Pain Headache Rep. 2021;25(11):75.
Aronsson V, Toivanen S, Leineweber C, Nyberg A. Can a poor psychosocial work environment and insufcient organizational resources explain the higher risk of ill-health and sickness absence in human service occupations? Evidence from a Swedish national cohort. Scand J Public Health. 2019;47(3):310–7.
Stovner LJ, Hagen K, Linde M, Steiner TJ. The global prevalence of headache: an update, with analysis of the influences of methodological factors on prevalence estimates. J Headache Pain. 2022;23(1):34.
Shimizu T, Sakai F, Miyake H, Sone T, Sato M, Tanabe S, Azuma Y, Dodick DW. Disability, quality of life, productivity impairment and employer costs of migraine in the workplace. J Headache Pain. 2021;22(1):29.
Thomas H, Kothari SF, Husøy A, Jensen RH, Katsarava Z, Tinelli M, Steiner TJ. The relationship between headache-attributed disability and lost productivity: 2. Empirical evidence from population-based studies in nine disparate countries. J Headache Pain. 2021;22(1):153.
Crocker J, Major B, Steele C. Social stigma. In: Gilbert DT, Fiske ST, Lindzey G, editors. The handbook of social psychology. London: McGraw-Hill; 1998. p. 504–53.
Al-Zahrani J, Shubair MM, Al-Ghamdi S, Aldossari KK, Alsalamah M, Al-Khateeb BF, Saeed A, Alshahrani S, AlSuwaidan AS, Alrasheed AA, El-Metwally A. Psychological predictors of chronic pain in Al Kharj region, Saudi Arabia. Ann Gen Psychiatry. 2021;20(1):23.
Waugh OC, Byrne DG, Nicholas MK. Internalized stigma in people living with chronic pain. J Pain. 2014;15(5):550.e1-10.
Dragioti E, Levin LÅ, Bernfort L, Larsson B, Gerdle B. Insomnia severity and its relationship with demographics, pain features, anxiety, and depression in older adults with and without pain: cross-sectional population-based results from the PainS65+ cohort. Ann Gen Psychiatry. 2017;23(16):15.
Racine M. Chronic pain and suicide risk: a comprehensive review. Prog Neuropsychopharmacol Biol Psychiatry. 2018;87(Pt B):269–80.
Wei S, Li H, Hou J, Chen W, Chen X, Qin X. Comparison of the characteristics of suicide attempters with major depressive disorder and those with no psychiatric diagnosis in emergency departments of general hospitals in China. Ann Gen Psychiatry. 2017;1(16):44.
Pompili M. Critical appraisal of major depression with suicidal ideation. Ann Gen Psychiatry. 2019;31(18):7.
Corrigan PW, Larson JE, Rüsch N. Self-stigma and the “why try” effect: impact on life goals and evidence-based practices. World Psychiatry. 2009;8(2):75–81.
Corrigan PW, Rao D. On the self-stigma of mental illness: stages, disclosure, and strategies for change. Can J Psychiatry. 2012;57(8):464–9.
Pescosolido BA, Martin JK. The stigma complex. Annu Rev Sociol. 2015;41:87–116.
Subu MA, Wati DF, Netrida N, Priscilla V, Dias JM, Abraham MS, Slewa-Younan S, Al-Yateem N. Types of stigma experienced by patients with mental illness and mental health nurses in Indonesia: a qualitative content analysis. Int J Ment Health Syst. 2021;15(1):77.
Corrigan P, Kerr A, Knudsen L. The stigma of mental illness: explanatory models and methods for change. Appl Prev Psychol. 2005;11:179–90.
Corrigan P, Watson A, Barr L. The self-stigma of mental illness: implications for self-esteem and self-efficacy. J Soc Clin Psychol. 2006;25:875–84.
Ritsher JB, Phelan JC. Internalized stigma predicts erosion of morale among psychiatric outpatients. Psychiatry Res. 2004;129(3):257–65.
Brohan E, Gauci D, Sartorius N, Thornicroft G, GAMIAN-Europe Study Group. Self-stigma, empowerment and perceived discrimination among people with bipolar disorder or depression in 13 European countries: the GAMIAN-Europe study. J Affect Disord. 2021;129(13):56–63.
Camp DL, Finlay WM, Lyons E. Is low self-esteem an inevitable consequence of stigma? An example from women with chronic mental health problems. Soc Sci Med. 2002;55(5):823–34.
Quartana PJ, Campbell CM, Edwards RR. Pain catastrophizing: a critical review. Expert Rev Neurother. 2009;9(5):745–58.
Sullivan MJ, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, Lefebvre JC. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain. 2001;17(1):52–64.
Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull. 2007;133(4):581–624.
Turk DC, Okifuji A. Psychological factors in chronic pain: evolution and revolution. J Consult Clin Psychol. 2002;70(3):678–90.
Bimpong K, Thomson K, Mcnamara CL, et al. The Gender Pain Gap: gender inequalities in pain across 19 European countries. Scand J Public Health. 2022;50(2):287–94.
Samulowitz A, Gremyr I, Eriksson E, Hensing G. “Brave Men” and “Emotional Women”: a theory-guided literature review on gender bias in health care and gendered norms towards patients with chronic pain. Pain Res Manag. 2018;25(2018):6358624.
Dao TT, LeResche L. Gender differences in pain. J Orofac Pain. 2000;14(3):169–84 (discussion 184-95).
Umeda M, Kim Y. Gender differences in the prevalence of chronic pain and leisure time physical activity among US adults: a NHANES study. Int J Environ Res Public Health. 2019;16(6):988.
Edmond-Charlton J, editor. Chapter 12. Sex and gender issues in pain, core curriculum for professional education in pain. 3rd ed. Seattle: IASP Press; 2005.
Templeton KJ. Sex and gender issues in pain management. J Bone Joint Surg Am. 2020;20(102 Suppl 1):32–5.
Racine M, Tousignant-Laflamme Y, Kloda LA, Dion D, Dupuis G, Choinière M. A systematic literature review of 10 years of research on sex/gender and pain perception - part 2: do biopsychosocial factors alter pain sensitivity differently in women and men? Pain. 2012;153(3):619–35.
Bernardes SF, Lima ML. Being less of a man or less of a woman: perceptions of chronic pain patients’ gender identities. Eur J Pain. 2010;14(2):194–9.
Homann DE, Tarzian AJ. The girl who cried pain: a bias against women in the treatment of pain. J Law Med Ethics. 2001;28(4):13–27.
Werner A, Isaksen LW, Malterud K. ‘I am not the kind of woman who complains of everything’: illness stories on self and shame in women with chronic pain. Soc Sci Med. 2004;59(5):1035–45.
Cosio D, Demyan A. Chronic pain management in marginalized populations: how to rebalance the provider-patient relationship. Pract Pain Manag. 2021;21(5).
Prego-Jimenez S, Pereda-Pereda E, Perez-Tejada J, Aliri J, Goñi-Balentziaga O, Labaka A. The impact of sexism and gender stereotypes on the legitimization of women’s low back pain. Pain Manag Nurs. 2022;S1524–9042(22):00097–102.
Takahashi TT, Ornello R, Quatrosi G, Torrente A, Albanese M, Vigneri S, Guglielmetti M, Maria De Marco C, Dutordoir C, Colangeli E, Fuccaro M, Di Lenola D, Spuntarelli V, Pilati L, Di Marco S, Van Dycke A, Abdullahi RA, Maassen van den Brink A, Martelletti P. Medication overuse and drug addiction: a narrative review from addiction perspective. J Headache Pain. 2021;22(1):32.
Zhang M, Zhang Y, Li Z, Hu L, Kong Y. Sexism-related stigma affects pain perception. Neural Plast. 2021;27(2021):6612456.
Kurzban R, Leary MR. Evolutionary origins of stigmatization: the functions of social exclusion. Psychol Bull. 2001;127(2):187–208.
Neuberg SL, Smith DM, Asher T. Why people stigmatize: toward a biocultural framework. In: Heatherton TF, Kleck RE, Hebl MR, Hull JG, editors. The social psychology of stigma. New York: Guilford Press; 2000. p. 31–61.
Schaller M, Neuberg S. Danger, disease, and the nature of prejudice(s). Amsterdam: Elsevier; 2012. https://doi.org/10.1016/B978-0-12-394281-4.00001-5.
De Ruddere L, Goubert L, Stevens M, de Williams CAC, Crombez G. Discounting pain in the absence of medical evidence is explained by negative evaluation of the patient. Pain. 2013;154(5):669–76.
O’Brien LT, Major B. System-justifying beliefs and psychological well-being: the roles of group status and identity. Pers Soc Psychol Bull. 2005;31(12):1718–29.
Staton LJ, Panda M, Chen I, Genao I, Kurz J, Pasanen M, Mechaber AJ, Menon M, O’Rorke J, Wood J, Rosenberg E, Faeslis C, Carey T, Calleson D, Cykert S. When race matters: disagreement in pain perception between patients and their physicians in primary care. J Natl Med Assoc. 2007;99(5):532–8.
Notcutt W, Gibbs G. Inadequate pain management: myth, stigma and professional fear. Postgrad Med J. 2010;86(1018):453–8.
Nuseir K, Kassab M, Almomani B. Healthcare providers’ knowledge and current practice of pain assessment and management: how much progress have we made? Pain Res Manag. 2016;2016:8432973.
McDonnell E, Harmon D. Chronic pain patients’ perceptions of prescription opioids: a systematic review. SN Compr Clin Med. 2020;2:2816–24.
Cook JE, Purdie-Vaughns V, Meyer IH, Busch JTA. Intervening within and across levels: a multilevel approach to stigma and public health. Soc Sci Med. 2014;103:101–9.
D’Amico D, Tepper SJ, Guastafierro E, Toppo C, Leonardi M, Grazzi L, Martelletti P, Raggi A. Mapping assessments instruments for headache disorders against the ICF biopsychosocial model of health and disability. Int J Environ Res Public Health. 2021;18(1):246.
Raggi A, Leonardi M, Sacco S, Martelletti P. Migraine outcome should not be used to determine diagnosis, severity, and therapy: moving towards a multiparametric definition of chronicity. Pain Ther. 2022;11(2):331–9.
Young WB, Park JE, Tian IX, Kempner J. The stigma of migraine. PLoS ONE. 2013;8: e54074.
Sacco S, Braschinsky M, Ducros A, Lampl C, Little P, van den Brink AM, Pozo-Rosich P, Reuter U, de la Torre ER, Sanchez Del Rio M, Sinclair AJ, Katsarava Z, Martelletti P. European headache federation consensus on the definition of resistant and refractory migraine: developed with the endorsement of the European Migraine & Headache Alliance (EMHA). J Headache Pain. 2020;21(1):76.
Eccleston C. Embodied: the psychology of physical sensation. Oxford: Oxford University Press; 2016.
Eccleston C, Crombez G. Worry and chronic pain: a misdirected problem solving model. Pain. 2007;132(3):233–6.
Eccleston C. A normal psychology of chronic pain. Psychologist. 2011;24(6):422–5.
Pelletier R, Higgins J, Bourbonnais D. Is neuroplasticity in the central nervous system the missing link to our understanding of chronic musculoskeletal disorders? BMC Musculoskelet Disord. 2015;12(16):25.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Author Contributions
All authors contributed to concept and design, statistical analysis, drafting the manuscript and approval of the final version of the manuscript.
Disclosures
Francesca Perugino and Valerio De Angelis have nothing to disclose. Maurizio Pompili is editor-in-chief of Annals of General Psychiatry. Paolo Martelletti is editor-in-chief of The Journal of Headache and Pain and editor-in-chief of SN Comprehensive Clinical Medicine.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Perugino, F., De Angelis, V., Pompili, M. et al. Stigma and Chronic Pain. Pain Ther 11, 1085–1094 (2022). https://doi.org/10.1007/s40122-022-00418-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-022-00418-5