Abstract
Introduction
Levornidazole is a novel nitroimidazole antimicrobial agent active against anaerobes. We aimed to investigate the pharmacokinetic (PK) profile of levornidazole after single and multiple oral doses of levornidazole tablets in healthy Chinese subjects and propose the dosing regimen based on pharmacokinetic/pharmacodynamic (PK/PD) analysis.
Methods
A single-center, randomized, double-blind, placebo-controlled study was conducted with a single ascending dose (250, 500, 1000, and 1500 mg) and multiple doses of 500 mg levornidazole q12h for 7 days. Food effect on PK and absolute bioavailability were investigated at the 500 mg dose level. Blood and urine samples were collected to determine the PK parameters of levornidazole. The probability of target attainment (PTA) and cumulative fraction of response (CFR) were calculated by Monte Carlo simulation to predict the clinical efficacy of levornidazole tablets.
Results
Plasma concentration reached peak about 0.5 h after single dose (250–1500 mg) of levornidazole tablets. The maximal concentration (Cmax) and exposure (AUC0–∞) of levornidazole increased linearly with dose. High-fat diet did not affect the absorption extent of levornidazole tablets. The absolute oral bioavailability of levornidazole tablets was 98.3% ± 7.6%, associated with large apparent volume of distribution (48.68 ± 4.92 l) and long half-life (11.93 ± 1.28 h). The urinary excretion of levornidazole was 7.99%. Levornidazole, administered at either 500 mg q12h or 750 mg q24h, achieved a CFR > 95.4% and PTA > 99% for B. fragilis (minimum inhibitory concentration ≤ 1.0 mg/l) infections.
Conclusion
Levornidazole tablets are absorbed rapidly and completely and distributed extensively with a long half-life and low urinary excretion after a single dose or multiple doses in healthy Chinese subjects. Levornidazole tablets can be taken with or without food. Levornidazole tablets 500 mg q12h and 750 mg q24h are expected to achieve the desired efficacy in B. fragilis infections.
Clinical Trail Registration
Trial registration number CTR20160786 at http://www.chinadrugtrials.org.cn/.
Similar content being viewed by others
Why carry out this study? |
Levornidazole is a novel nitroimidazole antimicrobial agent active against anaerobes. |
The pharmacokinetic properties and optimal dosing regimen of levornidazole tablets have not been studied adequately in Chinese subjects. |
This single-center, randomized, double-blind, placebo-controlled study aimed to evaluate the PK profiles of levornidazole after single ascending doses and multiple doses in healthy volunteers. Food effect on PK and absolute bioavailability were also investigated. |
The probability of target attainment (PTA) and cumulative fraction of response (CFR) were calculated by Monte Carlo simulation to predict the clinical efficacy of levornidazole tablets administered by different dosing regimens. |
What was learned from the study? |
We found that plasma concentration reached its peak about 0.5 h after a single dose (250–1500 mg) of levornidazole tablets. The maximal concentration (Cmax) and exposure (AUC0-∞) of levornidazole increased linearly with dose. High-fat diet did not affect the absorption extent of levornidazole tablets. |
The absolute oral bioavailability of levornidazole tablets was 98.3 ± 7.6%, associated with large apparent volume of distribution (48.68 ± 4.92 l) and long half-life (11.93 ± 1.28 h). |
The accumulation ratio was 1.98 ± 0.17 after multiple doses of levornidazole tablets 500 mg q12h. |
The urinary excretion of levornidazole and its major metabolite M16 was 7.99% and 34.02%, respectively. Levornidazole, administered at either 500 mg q12h or 750 mg q24h, achieved a CFR > 95.4% and PTA > 99% for B. fragilis (minimum inhibitory concentration ≤ 1.0 mg/l) infections. |
Our results indicate that levornidazole tablets are absorbed rapidly and completely and distributed extensively with a long half-life and low urinary excretion after a single dose or multiple doses in healthy Chinese subjects. |
Levornidazole tablets can be taken with or without food. Levornidazole tablets 500 mg q12h and 750 mg q24h are expected to achieve the desired efficacy in B. fragilis infections. |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.14125682.
Introduction
Levornidazole is a novel nitroimidazole antimicrobial agent killing bacteria by blocking the synthesis of the DNA helix or the transcription and replication of bacterial DNA. Levornidazole is the levo isomer of ornidazole with the same antibacterial mechanism but improved safety, especially a lower incidence of adverse reactions in the central nervous system [1]. The in vitro activity of levornidazole against most anaerobic species, such as Bacteroides thetaiotaomicron, Clostridium difficile, Clostridium perfringens, Peptostreptococcus spp., and especially Bacteroides fragilis, is similar to or slightly stronger than those of metronidazole, ornidazole, and dextrornidazole [2, 3]. The data from the completed clinical trials have proved that levornidazole is a safe and highly effective new anti-anaerobic agent with good market prospect.
Levornidazole is available in two dosage forms, i.e., an injectable formulation and tablets. The pharmacokinetic (PK) study on the injection of levornidazole and sodium chloride in Chinese adults has shown that single-dose administration is safe within the range of 500–1500 mg. Accumulation is observed after administration of repeat doses. Levornidazole is primarily metabolized to phase II inactive metabolite M16 (glucuronide conjugates) in human liver and eliminated via kidneys [4,5,6]. The PK profiles of levornidazole tablets have been examined after single ascending doses of 250–1000 mg and multiple doses of 500 mg q12h in healthy Chinese subjects. However, the safety and tolerability as well as accumulation of levornidazole have not been evaluated for levornidazole tablets after multiple oral doses [7]. Furthermore, it is required to further clarify the absolute oral bioavailability and the route of elimination of levornidazole tablets.
Pharmacokinetic/pharmacodynamic (PK/PD) analysis plays a crucial role in dose optimization of antimicrobial agents [8]. Early studies have shown that levornidazole is a concentration-dependent antibiotic. The area under the plasma unbound drug concentration-time curve/minimum inhibitory concentration (AUC/MIC) and maximal plasma unbound drug concentration/MIC (Cmax/MIC) are the PK/PD indices most relevant to levornidazole efficacy [9]. The previous findings of our team suggest that the accumulation of levornidazole will be alleviated if the dosing regimen is changed from 500 mg q12h to 750 mg q24h. PK/PD studies also indicate that both dosing regimens can achieve good microbiological efficacy for common anaerobes [4, 10]. However, no data are available to support the desired probability of target attainment (PTA) and cumulative fraction of response (CFR) (> 90% required for both indices) of levornidazole tablet 500 mg q12h or 750 mg q24h in the treatment of anaerobic infections.
This study was designed to analyze the PK properties of levornidazole after single and multiple oral doses of levornidazole tablets in healthy Chinese subjects, including the effects of food on PK profile, absolute bioavailability, and the route of elimination of levornidazole tablets. PK/PD analysis was also performed to evaluate the optimal dosing regimen in clinical practice.
Methods
Study Design
This study was approved by Huashan Hospital Institutional Review Board of Fudan University (IRB# 2016-349). The conduct of this study conformed to the ethical principles of the Declaration of Helsinki and the International Council for Harmonisation Good Clinical Practice guidelines. All subjects signed informed consent voluntarily before screening procedures. This clinical trial was registered at China Drug Trials Registry (no. CTR20160786) at http://www.chinadrugtrials.org.cn/.
A single-center, randomized, double-blind, placebo-controlled study was designed to evaluate the PK and safety profiles of levornidazole after oral administration of a single dose and multiple doses. The subjects received a single ascending dose of 250, 500, 1000, or 1500 mg. A self-crossover design was applied for the 500 mg dose level to examine the effects of food on PK. Ten subjects were enrolled in each dose group (250, 1000, and 1500 mg) except the 500 mg dose group, which included 12 participants to repeat the dose under fed conditions (high-fat diet) after the end of a single dose under fasted conditions. In a multiple-dose study of levornidazole tablets, 500 mg levornidazole was administered q12h to ten subjects for 7 consecutive days. Only one dose (morning dose) was scheduled on Day 7. In each dose group, there were equal numbers of males and females. Two subjects received placebo and the remaining subjects received levornidazole tablets in each dose group.
The absolute oral bioavailability was investigated in a single-center, randomized, open-label, self-crossover, two-cycle study design. Each of the 12 enrolled male subjects took levornidazole tablets 500 mg orally under fasted conditions, followed by a 5-day washout period, and received 500 mg levornidazole and NaCl via IV infusion.
Study Participants
All the enrolled subjects were healthy Chinese males or females aged 18–75 years, with body mass index of 19–26 kg/m2. Physical examination, vital signs, 12-lead electrocardiogram (ECG), and laboratory tests did not show abnormality. The subjects were excluded for any of the following: surgery that may affect drug absorption or a history of cardiovascular or neuropsychiatric disorders; known or suspected hypersensitivity to nitroimidazoles or history of allergy to any drug; pregnant or breastfeeding women; positive result for any of HIV-Ab, HBsAg, HCV-Ab, or syphilis test.
The subjects were monitored after drug administration by physical examination, vital signs, 12-lead ECG, adverse events, and laboratory tests on the day of discharge.
Investigational Drug and the Matching Placebo
Levornidazole (lot number: 201507011) was provided as levornidazole 250 mg tablets. The levornidazole-matching placebo (lot number: 201608042) was provided as pregelatinized starch/starch/magnesium stearate tablets, completely the same as levornidazole tablets in color, smell, and appearance. Injection of levornidazole and NaCl (100 ml/vial, lot number: 201605061) contains 500 mg levornidazole. The investigational drug and placebo were provided by Sanhome Pharmaceutical, Co., Ltd (Nanjing, China).
PK Sample Collection
Blood samples were collected at pre-dose (0 h) and 0.25, 0.5, 1, 2, 4, 8, 12, 24, 36, 48, 60, 72, and 96 h post-dose in single-dose study. In the multiple-dose study, blood samples were drawn before the first dose and 0.25, 0.5, 1, 2, 4, 8, and 12 h post-dose on Day 1, before the first dose on Days 2–6, before the final dose, and 0.25, 0.5, 1, 2, 4, 8, 12, 24, 36, 48, 60, 72, and 96 h after the final dose. The blood samples for calculating absolute bioavailability were drawn pre-dose (0 h) and 0.25, 0.5, 1, 2, 4, 8, 12, 24, 36, 48, 60, 72, and 96 h post-dose. Each levornidazole dose was administered via intravenous infusion over 1 h. Blood samples (4 ml) were put into a heparin tube and subjected to centrifugation at 3000 rpm for 10 min to separate plasma. The supernatant was aliquoted to two cryovial tubes for storage at – 20 °C until assay.
Urine samples were collected at pre-dose (− 12 to 0 h) and at the following intervals post-dose in the absolute bioavailability study: 0–4, 4–8, 8–12, 12–24, 24–48, 48–72, and 72–96 h. The urine samples were stored at – 20 °C or lower in a refrigerator until assay.
Assay of Levornidazole and Major Metabolite M16 in Plasma and Urine
The validated ultra-performance liquid chromatography-tandem mass spectrometry (UPLC-MS/MS) was used to determine the concentrations of levornidazole and the major metabolite M16 in plasma and urine samples [11, 12]. The samples were processed by liquid–liquid extraction before the assay. The UPLC-MS/MS assay demonstrated a linear range of 0.0100–5.00 mg/l for determination of levornidazole in plasma and urine samples. For assay of M16, the plasma samples were processed by solid-phase extraction while the urine samples were processed by liquid-liquid extraction. The UPLC-MS/MS assay provided a linear range of 0.00500–2.50 mg/l for determination of M16 in plasma and a linear range of 0.0100–10.0 mg/l for determination of M16 in urine.
PK Analysis
Phoenix WinNonlin 6.3 (Certara Corp., USA) software was used to calculate the PK parameters of levornidazole and M16 based on non-compartmental approaches. Student's t-test (IBM SPSS Statistics 19.0, USA) was used to compare the PK parameters of levornidazole on Day 1 and Day 7. The accumulation ratio (AR) was calculated to evaluate levornidazole accumulation in the body. Linear regression analysis was performed between Cmax or AUC0-∞ and doses using the power model.
WinNonlin software was used to fit the PK parameters after multiple doses of levornidazole tablets 500 mg q12h based on a two-compartment model. The resulting parameters were used to predict the PK parameters of levornidazole following multiple doses of levornidazole tablets 750 mg q24h for 7 consecutive days.
PK/PD Analysis
The in vitro PD data of levornidazole were excerpted from our previous study [2]. Levornidazole was tested in vitro for the activity against the 375 strains of anaerobes isolated from the blood, feces, and secretions of patients in Shanghai Huashan Hospital during the period from 2006 to 2013 by MIC determination. The test strains included 181 strains of gram-negative bacilli, 139 strains of gram-positive bacilli, 44 strains of gram-positive cocci, and 11 strains of gram-negative cocci.
The PK and MIC results of levornidazole were combined to perform Monte Carlo simulation. Assuming the target values of PK/PD indices for levornidazole against B. fragilis as Cmax/MIC = 14.1 and AUC0-24/MIC = 157.6 [9], the corresponding PTA and CFR were calculated for levornidazole tablets 500 mg q12h and 750 mg q24h in treatment of infections caused by B. fragilis.
Results
Safety and Tolerability
Of the 64 subjects enrolled in this study, 10 received placebo and 54 received the investigational drug. The demographic details are presented in Table 1. Study drug-related adverse events (AE) were reported in five (7.4%, 4/54) subjects after oral single ascending doses of 250–1500 mg levornidazole tablets. All the AEs were mild and transient and resolved spontaneously without treatment. No study drug-related AE was observed after multiple doses of levornidazole tablets (Table 2).
PK Parameters
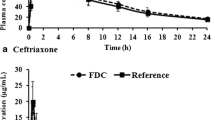
The semi-log plot of plasma concentration-time profiles following single ascending doses of levornidazole 250–1500 mg are presented in Fig. 1a. The corresponding PK parameters are listed in Table 3. Levornidazole was absorbed rapidly after oral administration under fasted conditions and reached peak plasma concentration about 0.5 h post-dose. The mean Cmax and AUC0–∞ increased with dose within a dose range from 250 to 1500 mg. Power regression model analysis demonstrated that levornidazole Cmax and AUC0–∞ increased proportionally with dose within a dose range from 250 to 1500 mg (Fig. 2). High-fat diet delayed the median Tmax from 0.5 h to 2 h post-dose but had no significant effect on Cmax and AUC (P > 0.05).
Power model to fit the increase of levornidazole Cmax (a) and AUC0–∞ (b) with increasing doses. Power model formula: LnPara = lnα + β × lnDose, where Para denotes the PK parameter, and lnα and β represent intercept and slope, respectively. AUC0–∞ area under the concentration-time curve from time 0 extrapolated to infinity, Cmax maximum concentration
The absolute bioavailability study found that after IV infusion, the Cmax of levornidazole was 33.9% higher than that following an oral single dose of levornidazole tablets in healthy subjects (P < 0.01). The other PK parameters did not show a significant difference (P > 0.05) (Table 3), such as T1/2 (11.93 ± 1.28 vs. 11.74 ± 1.12 h) and apparent volume of distribution (48.68 ± 4.92 versus 47.88 ± 5.60 l). The absolute oral bioavailability of levornidazole tablets calculated from AUC0–∞ was 98.3% ± 7.6%. At 96 h after oral administration and IV infusion, the average cumulative urinary excretion was 7.99% and 8.13% for levornidazole and 34.02% and 35.78% for metabolite M16, respectively. The AUC0–∞ ratio between M16 and levornidazole (i.e., metabolic ratio) was 13.05% and 12.83%, respectively. The trough plasma concentration increased gradually after multiple doses of levornidazole tablets 500 mg q12h in healthy subjects and reached steady state 3 days later. Compared to the PK parameters of levornidazole after the first dose on Day 1, the mean Cmax value after the final dose on Day 7 increased by 85.4% (13.0 mg/l vs. 24.1 mg/l) and AUC0–∞ increased by 1.46-fold (163.79 mg h/l vs. 403.14 mg h/l) (P < 0.01) (Table 3). Levornidazole accumulated in the body after administration of levornidazole tablets 500 mg q12h for 7 consecutive days, evidenced by AR of 1.98 ± 0.17.
The dosing regimen of levornidazole tablets 750 mg q24h for 7 consecutive days was simulated, and the AUC0-24, Cmax, and AR of levornidazole after the final dose on Day 7 were expected to be 293.35 ± 39.37 mg h/l, 23.7 ± 4.35 mg/l, and 1.35 ± 0.07, respectively.
Results of PK/PD Analysis
Figure 3 depicts the PTA of two dosing regimens of levornidazole tablets (500 mg q12h and 750 mg q24h, for 7 days) for B. fragilis. When levornidazole MIC ≤ 1 mg/l was used against B. fragilis, both dosing regimens resulted in the desired PTA (> 99%) in terms of AUC0–24/MIC target (157.6) or Cmax/MIC target (14.1). When levornidazole MIC = 2 mg/l, levornidazole 500 mg q12h achieved up to 95% PTA for AUC0–24/MIC target, but < 90% PTA for the Cmax/MIC target. Levornidazole 500 mg q24h achieved PTA < 90% for both AUC0–24/MIC and Cmax/MIC targets. Considering the distribution of levornidazole MIC values against B. fragilis, both dosing regimens are expected to achieve CFR values of 97.2% and 96.7% in terms of AUC0–24/MIC and 95.4% and 96.4% in terms of Cmax/MIC.
The probability of target attainment (PTA) of levornidazole for Bacteroides fragilis in terms of AUC0–24/MIC and Cmax/MIC. Histograms represent the distribution frequency, corresponding to the left ordinate. The broken lines represent PTA, corresponding to the right ordinate. The horizontal dotted line represents 90% PTA, corresponding to the pharmacodynamic effect of 3 log reduction of bacterial load. The target values are derived from in vitro PK/PD studies [9]. AUC0–24 area under the concentration-time curve from time 0 to 24 h, Cmax maximum concentration, MIC minimum inhibitory concentration, PK/PD pharmacokinetic/pharmacodynamic, PTA probability of target attainment
Discussion
Table 4 summarizes the key PK parameters of levornidazole versus metronidazole tablet [13], tinidazole tablet [14], and ornidazole tablet [15]. Levornidazole tablet is absorbed rapidly in the human body, associated higher exposure than tinidazole tablet, longer T1/2 than metronidazole, and PK parameters close to tinidazole. However, levornidazole is used at a lower dose than tinidazole tablet in clinical settings. The PK parameters after a single oral dose of levornidazole tablets in the present study were comparable to those in a previous report [7]. High-fat diet delays the rate of absorption after a 500 mg oral dose of levornidazole tablets compared to the absorption under fasted conditions, but does not affect the extent of absorption. Therefore, levornidazole tablets can be administered with or without food. The absolute oral bioavailability of levornidazole tablets is close to 100%, proving its complete absorption. This finding informs clinicians that levornidazole tablets can be used subsequent to injection of levornidazole and NaCl to institute a sequential regimen for treatment of the intra-abdominal, pelvic, and oral infections caused by anaerobic pathogens in clinical practice.
Our previous studies characterized the metabolism of injection of levornidazole NaCl in young healthy Chinese adults. The phase I metabolites of levornidazole include two oxidative products (M1 and M2) and one hydrolytic dechlorination product (M4) of levornidazole and two cleavage products of the imidazole ring (M3 and M5). The metabolic ratio is < 3% for all the five phase I metabolites. For phase II metabolites M6 (sulfate conjugate) and M16 (glucuronide conjugate), the metabolic ratio is 0.03% and 15.05%, respectively [4, 10]. In the present study, the metabolic ratio of M16 was 13.05% after a single oral dose of levornidazole tablets, comparable to the result (12.83%) after IV infusion of levornidazole in healthy Chinese subjects. These ratios are essentially consistent with the result from previous study. Overall, about 43% of parent drug levornidazole and its metabolite M16 is eliminated via the kidneys, suggesting that levornidazole tablet is similar to the drugs in the same class, primarily metabolized in human liver by phase II glucuronization and eliminated through the kidneys.
The AR of levornidazole is up to 1.98 after repeated oral doses of levornidazole tablets 500 mg q12h. This proves the accumulation of levornidazole in the human body. However, levornidazole was safe and well tolerated following an oral single ascending dose of levornidazole tablets from 250 to 1500 mg and multiple doses of 500 mg q12h for 7 consecutive days in healthy Chinese subjects. The dosing regimen of levornidazole tablets 750 mg q24h may reduce the AR of levornidazole to 1.35 and so significantly decrease drug accumulation in the body. This result is consistent with the AR result for injection of levornidazole NaCl 500 mg q12h and 750 mg q24h dosing regimens [4, 10].
To our knowledge, this is the first time PK/PD analysis has been performed on the dosing regimens of levornidazole tablets 500 mg q12h and 750 mg q24h based on the levornidazole MIC values against the anaerobic pathogens isolated from Chinese patients. Our findings justify the utility of these dosing regimens. Monte Carlo simulation demonstrates that both dosing regimens of levornidazole can achieve CFR > 90% against B. fragilis, informing good microbiological efficacy. When levornidazole MIC ≤ 1 mg/l is used against B. fragilis, both dosing regimens can achieve > 90% PTA on average in terms of the specified PD targets. Therefore, it is expected that for the infections caused by B. fragilis (levornidazole MIC ≤ 1 mg/l), levornidazole tablets 500 mg q12h or 750 mg q24h for 7 consecutive days will achieve the desired clinical efficacy. In addition to PK/PD analysis targeting B. fragilis, we also calculated the PK/PD indices for both dosing regimens of levornidazole against common anaerobes using the single point estimation method. Both dosing regimens of levornidazole tablets resulted in high PK/PD indices (Cmax/MIC90 ≥ 23.7, AUC0–24/MIC90 ≥ 293.4, Table 5) for other Bacteroides spp., Clostridium difficile, and Peptostreptococcus, but not Prevotella and other Clostridium spp. Therefore, levornidazole tablets of either 500 mg q12h or 750 mg q24h can be recommended for treatment of the infections caused by common anaerobes. The dosing regimen of 750 mg q24h is especially preferred for lower accumulation and good compliance. Additionally, we found in a previous study that injection of levornidazole and NaCl showed similar PK profiles in both elderly and young healthy subjects [4]. The finding may inform that the dosing regimen of levornidazole tablets 500 mg q12h or 750 mg q24h is also indicated for elderly patients. Levornidazole tablets provide additional treatment options for managing anaerobic infections in the elderly.
Adverse drug reactions may occur more frequently in the elderly because of physiological dysfunction and atrophy of tissues and organs [16]. Our previous studies did not find drug-related adverse events in healthy elderly subjects and patients of different ages after intravenous injection of levornidazole [4, 5]. The results of this study also showed that levornidazole was well tolerated with a good safety profile. The incidence of adverse reactions of levornidazole did not vary significantly with age.
Antimicrobial resistance is a global issue threatening public safety. All healthcare professionals should be aware of the knowledge on antimicrobial resistance and the rational use of antimicrobial agents [17]. The potential and emergence of levornidazole resistance in pathogenic anaerobes should be monitored closely in future trials and clinical practice.
The proposed dosing regimens of levornidazole tablets in this study are based on the results of PK data and PK/PD studies in healthy subjects. They should be further verified in well-designed clinical trials in real patients with anerobic infection. These simulated results should also be confirmed in real-world patients.
Conclusion
Levornidazole is absorbed rapidly and completely, distributed extensively in the body with a long half-life and low urinary excretion rate after single and multiple doses of levornidazole tablets in healthy Chinese subjects. Oral levornidazole treatment is safe and well tolerated. Levornidazole tablets can be taken with or without food. The dosing regimen of levornidazole tablets 500 mg q12h or 750 mg q24h is expected to achieve satisfactory clinical efficacy for the infections caused by B. fragilis and other common anaerobic pathogens.
References
Sun JH, Wang ZQ, Gu XL, Mu R. Comparative study of L-and D-ornidazole in terms of central nervous system toxicity in mice. J Chin Pharm Univ. 2008;4:343–7.
Hu J, Zhang J, Wu S, et al. Evaluation of the in vitro activity of levornidazole, its metabolites and comparators against clinical anaerobic bacteria. Int J Antimicrob Agents. 2014;44:514–9.
Hu J, Zhang J, Chen Y, et al. In vitro bactericidal property of levornidazole against Bacteroides fragilis studied by time-kill assay and sigmoid Emax model analysis. Int J Antimicrob Agents. 2015;45:673–5.
Guo B, He G, Wu X, et al. Clinical pharmacokinetics of levornidazole in elderly subjects and dosing regimen evaluation using pharmacokinetic/pharmacodynamic analysis. Clin Ther. 2017;39:1336–46.
Wu H, Xie S, Yu J, et al. Pharmacokinetics and pharmacodynamics of levornidazole in patients with intra-abdominal anaerobic infection. Clin Ther. 2018;40:1548–55.
Zhao YN, Wu P, Sun H. Human tolerability and pharmacokinetic studies of levornidazole by dose escalation. Chin Pharm J. 2011;46:454457 ((in Chinese)).
Mu LL, Cheng ZN, Guo X, Luo X, Yu P. Investigation of chiral inversion and pharmacokinetics of laevo-ornidazole by high-performance liquid chromatography. J Clin Pharm Ther. 2013;38:31–5.
Asín-Prieto E, Rodríguez-Gascón A, Isla A. Applications of the pharmacokinetic/pharmacodynamic (PK/PD) analysis of antimicrobial agents. J Infect Chemother. 2015;21:319–29.
Hu J, Zhang J, Chen Y, Liang W, Wu S. In vitro anaerobic pharmacokinetic/ pharmacodynamic model to simulate the bactericidal activity of levornidazole against Bacteroides fragilis. Clini Ther. 2017;39:828–36.
Cao Y, Wu X, Chen Y, et al. Improved pharmacokinetic profile of levornidazole following intravenous infusion of 750 mg every 24h compared with 500 mg every 12h in healthy Chinese volunteers. Int J Antimicrob Agents. 2016;47:224–8.
Cao Y, Zhao M, Wu X, et al. Quantification of levornidazole and its metabolites in human plasma and urine by ultra-performance liquid chromatography-mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci. 2014;963:119–27.
He G, Guo B, Zhang J, et al. Determination of the sulfate and glucuronide conjugates of levornidazole in human plasma and urine, and levornidazole and its five metabolites in human feces by high performance liquid chromatography-tandem mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci. 2018;1081–1082:87–100.
Jensen JC, Gugler R. Single- and multiple-dose metronidazole kinetics. Clin Pharmacol Ther. 1983;34:481–7.
Tinidazole Tablets (TINDAMAX ®) Package Insert (2007 update).
Du J, Ma Z, Zhang Y, Wang T, Chen X, Zhong D. Simultaneous determination of ornidazole and its main metabolites in human plasma by LC-MS/MS: application to a pharmacokinetic study. Bioanalysis. 2014;6:2343–2256.
Gennaro FD, Vittozzi P, Gualano G, et al. Active pulmonary tuberculosis in elderly patients: a 2016–2019 retrospective analysis from an Italian Referral Hospital. Antibiotics (Basel). 2020;9:489.
Gennaro FD, Marotta C, Amicone M, et al. Italian young doctors’ knowledge, attitudes and practices on antibiotic use and resistance: A national cross-sectional survey. J Glob Antimicrob Resist. 2020;23:167–73.
Acknowledgements
We thank the participants of the study for their contribution.
Funding
This work was supported by grant from the New Drug Creation and Manufacturing Programme of the Ministry of Science and Technology of China (No. 2017ZX09304005). Sponsorship for the Rapid Service Fee was funded by Nanjing Sanhome Pharmaceutical Co., Ltd.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Nanjing Sanhome Pharmaceutical Co., Ltd., provided the study drug levornidazole and the matching placebo used in this study. The authors have no conflicts of interest regarding the content and publication of this article. Hailan Wu, Zhiqiang Wang, Yu Wang, Jicheng Yu, Yaxin Fan, Yi Li, Jingjing Wang, Guoying Cao, Beining Guo, Yuancheng Chen, Xiaofen Liu, Xingchen Bian, Jufang Wu, Hongtao Li, Xiaojie Wu, and Jing Zhang have nothing to disclose.
Compliance with Ethics Guidelines
This study was reviewed and approved by Huashan Hospital Institutional Review Board of Fudan University (IRB# 2016-349) and conducted in accordance with the ethical principles of the Declaration of Helsinki and Good Clinical Practice. All subjects provided informed consent to participate in the study.
Data Availability
The data sets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wu, H., Wang, Z., Wang, Y. et al. Pharmacokinetics of Levornidazole Tablet in Healthy Chinese Subjects and Proposed Dosing Regimen Based on Pharmacokinetic/Pharmacodynamic Analysis. Infect Dis Ther 10, 911–923 (2021). https://doi.org/10.1007/s40121-021-00428-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-021-00428-4