Abstract
Purpose
Vanishing bile duct syndrome (VBDS) is a rare, but potentially fatal adverse reaction triggered by certain medications. Few real-world studies have shown association between antibiotics and VBDS. We sought to quantify the risk and evaluate the clinical features of VBDS associated with antibiotics.
Methods
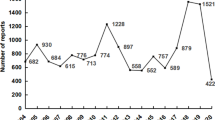
Data from 2004 to 2022 on VBDS events induced by antibiotics were retrieved from the FDA Adverse Event Reporting System (FAERS) database and disproportionality analyses were conducted. Furthermore, case reports from 2000 to 31 December 2022 on antibiotics-induced VBDS were retrieved for retrospective analysis.
Results
We collected 132 VBDS reports from the FAERS database. Fluoroquinolones had the greatest proportion and highest positive signal values of VBDS. The RORs (95% CIs) for antibiotics were fluoroquinolones 23.68 (18.12–30.95), macrolides 19.37 (13.58–27.62), carbapenems 17.39 (7.77–38.96), beta-lactam 13.28 (9.69–18.20), trimethoprim/sulfamethoxazole 9.05 (5.57–14.7), and tetracycline 4.02 (1.50–10.77). Twenty-three cases from 22 studies showed evidence of VBDS, beta-lactam (52.2%) was the most frequently reported agent. The median age was 45 years, the typical initial symptoms included rash (30.4%), fatigue/asthenia (26.1%), dark urine (21.7%) and Stevens–Johnson syndrome (SJS)/toxic epidermal necrolysis (TEN) (21.7%). The median time to onset of VBDS was 2 weeks. All cases had abnormal liver function test, and the median level of total bilirubin was 23.6 mg/dl (range 3.2–80 mg/dl). Cessation of culprit drugs and treatment with ursodeoxycholic acid (83.3%) were not associated with improved outcomes (57.1%).
Conclusion
This study identified thirteen antibacterial agents with significant reporting associations with VBDS. Fluoroquinolones may be a neglected agent of inducing VBDS.

Similar content being viewed by others
References
Desmet VJ. Vanishing bile duct syndrome in drug-induced liver disease. J Hepatol. 1997;26(Suppl 1):31–5.
Reau NS, Jensen DM. Vanishing bile duct syndrome. Clin Liver Dis. 2008;12:203–17.
Ahmad J, Barnhart HX, Bonacini M, et al. Value of liver biopsy in the diagnosis of drug-induced liver injury. J Hepatol. 2022;76:1070–8.
Rockey DC, Caldwell SH, Goodman ZD, Nelson RC, Smith AD. Liver Biopsy Hepatol. 2009;49:1017–44.
Geubel AP, Sempoux CL. Drug and toxin-induced bile duct disorders. J Gastroenterol Hepatol. 2000;15:1232–8.
Bessone F, Hernandez N, Tanno M, Roma MG. Drug-induced vanishing bile duct syndrome: from pathogenesis to diagnosis and therapeutics. Semin Liver Dis. 2021;41:331–48.
Padda MS, Sanchez M, Akhtar AJ, Boyer JL. Drug-induced cholestasis. Hepatology. 2011;53:1377–87.
Moradpour D, Altorfer J, Flury R, et al. Chlorpromazine-induced vanishing bile duct syndrome leading to biliary cirrhosis. Hepatology. 1994;20:1437–41.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases, 2012
Bonkovsky HL, Kleiner DE, Gu J, et al. Clinical presentations and outcomes of bile duct loss caused by drugs and herbal and dietary supplements. Hepatology. 2017;65:1267–77.
Schwarze C, Schmitz V, Fischer HP, Sauerbruch T, Spengler U. Vanishing bile duct syndrome associated with elevated pancreatic enzymes after short-term administration of amoxicillin. Eur J Gastroenterol Hepatol. 2002;14:1275–7.
Kim JS, Jang YR, Lee JW, et al. A case of amoxicillin-induced hepatocellular liver injury with bile-duct damage. Korean J Hepatol. 2011;17:229–32.
Li L, Zheng S, Chen Y. Stevens–Johnson syndrome and acute vanishing bile duct syndrome after the use of amoxicillin and naproxen in a child. J Int Med Res. 2019;47:4537–43.
Smith LA, Ignacio JR, Winesett MP, et al. Vanishing bile duct syndrome: amoxicillin–clavulanic acid associated intra-hepatic cholestasis responsive to ursodeoxycholic acid. J Pediatr Gastroenterol Nutr. 2005;41:469–73.
Li H, Li X, Liao XX, et al. Drug associated vanishing bile duct syndrome combined with hemophagocytic lymphohistiocytosis. World J Gastrointest Endosc. 2012;4:376–8.
Hashim A, Barnabas A, Miquel R, Agarwal K. Successful liver transplantation for drug-induced vanishing bile duct syndrome. BMJ Case Rep. 2020;13:e233052.
Faragalla K, Lau H, Wang HL, Liu J. Cloxacillin-induced acute vanishing bile duct syndrome: a case study and literature review. Br J Clin Pharmacol. 2022;88:4633–8.
Tajiri H, Etani Y, Mushiake S, Ozono K, Nakayama M. A favorable response to steroid therapy in a child with drug-associated acute vanishing bile duct syndrome and skin disorder. J Paediatr Child Health. 2008;44:234–6.
Zhao Z, Bao L, Yu X, et al. Acute vanishing bile duct syndrome after therapy with cephalosporin, metronidazole, and clotrimazole: a case report. Medicine (Baltimore). 2017;96:e8009.
Momen S, Dangiosse C, Wedgeworth E, Walsh S, Creamer D. A case of toxic epidermal necrolysis and vanishing bile duct syndrome, requiring liver transplantation. J Eur Acad Dermatol Venereol. 2017;31:e450–2.
Okan G, Yaylaci S, Peker O, Kaymakoglu S, Saruc M. Vanishing bile duct and Stevens–Johnson syndrome associated with ciprofloxacin treated with tacrolimus. World J Gastroenterol. 2008;14:4697–700.
Robinson W, Habr F, Manlolo J, Bhattacharya B. Moxifloxacin associated vanishing bile duct syndrome. J Clin Gastroenterol. 2010;44:72–3.
Bataille L, Rahier J, Geubel A. Delayed and prolonged cholestatic hepatitis with ductopenia after long-term ciprofloxacin therapy for Crohn’s disease. J Hepatol. 2002;37:696–9.
Levine C, Trivedi A, Thung SN, Perumalswami PV. Severe ductopenia and cholestasis from levofloxacin drug-induced liver injury: a case report and review. Semin Liver Dis. 2014;34:246–51.
Karnsakul W, Arkachaisri T, Atisook K, Wisuthsarewong W, Sattawatthamrong Y, Aanpreung P. Vanishing bile duct syndrome in a child with toxic epidermal necrolysis: an interplay of unbalanced immune regulatory mechanisms. Ann Hepatol. 2006;5:116–9.
Juricic D, Hrstic I, Radic D, et al. Vanishing bile duct syndrome associated with azithromycin in a 62-year-old man. Basic Clin Pharmacol Toxicol. 2010;106:62–5.
Silberstein SD. Migraine preventive treatment. Handb Clin Neurol. 2010;97:337–54.
Zubarev A, Haji K, Li M, Tiruvoipati R, Botha J. Meropenem-induced vanishing bile duct syndrome: a case report. J Int Med Res. 2020;48:1220737394.
Cho HJ, Jwa HJ, Kim KS, Gang DY, Kim JY. Urosodeoxycholic acid therapy in a child with trimethoprim-sulfamethoxazole-induced vanishing bile duct syndrome. Pediatr Gastroenterol Hepatol Nutr. 2013;16:273–8.
Kathi PR, Tama M, Ehrinpreis M, et al. Vanishing bile duct syndrome arising in a patient with HIV infection sequentially treated with trimethoprim/sulfamethoxazole and dapsone. Clin J Gastroenterol. 2020;13:276–80.
Lu MQ, Gong JY, Li CY, et al. A case of drug-associated vanishing bile duct syndrome. Chin J Pediatr. 2020;58(5):430–1 (in Chinese).
Li J, Zhao LL, Ye LH, et al. Two cases of drug⁃induced vanishing bile duct syndrome. Anhui Med Pharm J. 2019;23(5):1051–3 (in Chinese).
Chalasani N, Bonkovsky HL, Fontana R, et al. Features and outcomes of 899 patients with drug-induced liver injury: the DILIN prospective study. Gastroenterology. 2015;148:1340–52.
Wasuwanich P, Choudry H, So JM, Lowry S, Karnsakul W. Vanishing bile duct syndrome after drug-induced liver injury. Clin Res Hepatol Gastroenterol. 2022;46:102015.
Lakehal F, Dansette PM, Becquemont L, et al. Indirect cytotoxicity of flucloxacillin toward human biliary epithelium via metabolite formation in hepatocytes. Chem Res Toxicol. 2001;14:694–701.
Carey MA, van Pelt FN. Immunochemical detection of flucloxacillin adduct formation in livers of treated rats. Toxicology. 2005;216:41–8.
Meng X, Earnshaw CJ, Tailor A, et al. Amoxicillin and clavulanate form chemically and immunologically distinct multiple haptenic structures in patients. Chem Res Toxicol. 2016;29:1762–72.
Naisbitt DJ, Farrell J, Gordon SF, et al. Covalent binding of the nitroso metabolite of sulfamethoxazole leads to toxicity and major histocompatibility complex-restricted antigen presentation. Mol Pharmacol. 2002;62:628–37.
Liu ZX, Kaplowitz N. Immune-mediated drug-induced liver disease. Clin Liver Dis. 2002;6:755–74.
Levy C, Lindor KD. Drug-induced cholestasis. Clin Liver Dis. 2003;7:311–30.
Hautekeete ML, Horsmans Y, Van Waeyenberge C, et al. HLA association of amoxicillin–clavulanate—induced hepatitis. Gastroenterology. 1999;117:1181–6.
Amaral JD, Viana RJ, Ramalho RM, Steer CJ, Rodrigues CM. Bile acids: regulation of apoptosis by ursodeoxycholic acid. J Lipid Res. 2009;50:1721–34.
Paumgartner G, Beuers U. Ursodeoxycholic acid in cholestatic liver disease: mechanisms of action and therapeutic use revisited. Hepatology. 2002;36:525–31.
Lazaridis KN, Gores GJ, Lindor KD. Ursodeoxycholic acid mechanisms of action and clinical use in hepatobiliary disorders. J Hepatol. 2001;35:134–46.
White JC, Appleman S. Infliximab/plasmapheresis in vanishing bile duct syndrome secondary to toxic epidermal necrolysis. Pediatrics. 2014;134:e1194–8.
Kawasaki Y, Matsubara K, Hashimoto K, et al. Nonsteroidal anti-inflammatory drug-induced vanishing bile duct syndrome treated with plasmapheresis. J Pediatr Gastroenterol Nutr. 2013;57:e30–1.
Funding
None.
Author information
Authors and Affiliations
Contributions
JlW and ZD conceived of the study; JlW and ZD drafted and revised the manuscript; and JlW and SfW made data elaboration and performed statistical analyses. All authors contributed to the final manuscript and approved the submitted version.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest/competing interest to disclose with this manuscript.
Ethical approval
Ethical approval was not required.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, J., Wang, S., Wu, C. et al. Antibiotic-associated vanishing bile duct syndrome: a real-world retrospective and pharmacovigilance database analysis. Infection (2023). https://doi.org/10.1007/s15010-023-02132-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s15010-023-02132-6