Abstract
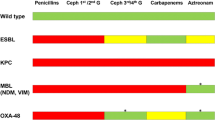
Ceftazidime–avibactam (CZA), meropenem–vaborbactam (MVB) and imipenem–relebactam (I–R) are combinations of old ß-lactams with novel non-ß-lactam ß-lactamase inhibitors (BLBLIs) able to inhibit some carbapenemases, such as the KPC-type, thus are becoming the standard for difficult-to-treat carbapenemase-producing Enterobacterales (CPE); a practical question is whether these novel BLBLIs should be used as monotherapy or as part of a combination regimen with other antibiotics, and if so, with which ones, to reduce the emergence of resistant strains and to optimize their efficacy. In this short review, we assessed clinical outcomes in patients with CPE-infections treated with the novel BLBLIs as mono- or combo-regimens, and laboratory studies on the synergistic effects with other antimicrobials. Available evidence on combination therapy is scarce and mainly limited to retrospective studies involving 630 patients treated with CZA: aminoglycosides were used in 39.6% of 336 patients treated with combo-regimens, followed by polymyxin B/colistin (24.4%), tigecycline (24.1%), carbapenems (13.4%) and fosfomycin (5.4%). Aminoglycosides could be useful in case of bloodstream and severe urinary infections. Pneumonia is a risk factor for CZA-resistance emergence: fosfomycin, due to favorable lung pharmacokinetics/pharmacodynamics, could represent an interesting partner; fosfomycin could be added also for osteomyelitis. Tigecycline could be preferred for intrabdominal and skin-soft tissue infections. Due to nephrotoxicity and lack of in vitro synergy, the association CZA/colistin seems not optimal. MVB and I–R were mostly used as monotherapies. Currently, there is no definitive evidence whether combinations are more effective than monotherapies; further studies are warranted, and to date only personal opinions can be provided.
Similar content being viewed by others
Change history
19 March 2021
A Correction to this paper has been published: https://doi.org/10.1007/s15010-021-01596-8
References
Stewart A, Harris P, Henderson A, Paterson D. Treatment of infections by OXA-48-producing Enterobacteriaceae. Antimicrob Agents Chemother. 2018;62:e01195-e1218.
Crass RL, Pai MP. Pharmacokinetics and Pharmacodynamics of β-Lactamase Inhibitors. Pharmacotherapy. 2019;39:182–95.
Yahav D, Giske CG, Grāmatniece A, Abodakpi H, Tam VH, Leibovici L. New β-Lactam-β-Lactamase inhibitor combinations. Clin Microbiol Rev. 2020;34:e00115-e120.
David 2019) David S, Reuter S, Harris SR, Glasner C, Feltwell T, Argimon S, et al. EuSCAPE Working Group; ESGEM Study Group, Feil EJ, Rossolini GM, Aanensen DM, Grundmann H. Epidemic of carbapenem-resistant Klebsiella pneumoniae in Europe is driven by nosocomial spread. Nat Microbiol. 2019;4:1919–1929
Gutiérrez-Gutiérrez B, Salamanca E, de Cueto M, et al; REIPI/ESGBIS/ INCREMENT Investigators. Effect of appropriate combination therapy on mortality of patients with bloodstream infections due to carbapenemase-producing Enterobacteriaceae (INCREMENT): a retrospective cohort study. Lancet Infect Dis 2017;17:726–34
Tumbarello M, Trecarichi EM, Corona A, De Rosa FG, Bassetti M, Mussini C, et al. Efficacy of Ceftazidime–avibactam Salvage Therapy in Patients With Infections Caused by Klebsiella pneumoniae Carbapenemase-producing K. pneumoniae. Clin Infect Dis. 2019;68:355–64.
Tavoschi L, Forni S, Porretta A, Righi L, Pieralli F, Menichetti F, et al. On Behalf Of The Tuscan Clinical Microbiology Laboratory Network. Prolonged outbreak of New Delhi metallo-beta-lactamase-producing carbapenem-resistant Enterobacterales (NDM-CRE), Tuscany, Italy, 2018 to 2019. Euro Surveill. 2020;25:2000085.
Bassetti M, Giacobbe DR, Giamarellou H, Viscoli C, Daikos GL, Dimopoulos G, et al.; Critically Ill Patients Study Group of the European Society of Clinical Microbiology and Infectious Disease (ESCMID); Hellenic Society of Chemotherapy (HSC) and Società Italiana di Terapia Antinfettiva (SITA). Management of KPC-producing Klebsiella pneumoniae infections. Clin Microbiol Infect. 2018;24:133–144
Rodríguez-Baño J, Gutiérrez-Gutiérrez B, Machuca I, Pascual A. Treatment of infections caused by extended-spectrum-beta-lactamase-, AmpC-, and Carbapenemase-producing Enterobacteriaceae. Clin Microbiol Rev. 2018;31:e00079-e117.
Doi Y. Treatment Options for Carbapenem-resistant Gram-negative Bacterial Infections. Clin Infect Dis. 2019;9:565-575
Shields RK, Potoski BA, Haidar G, Hao B, Doi Y, Chen L, et al. Clinical outcomes, drug toxicity, and emergence of ceftazidime–avibactam resistance among patients treated for carbapenem-resistant enterobacteriaceae infections. Clin Infect Dis. 2016;63:1615–8.
Shields RK, Nguyen MH, Chen L, Press EG, Potoski BA, Marini RV, et al. Ceftazidime–avibactam Is Superior to Other Treatment Regimens against Carbapenem-Resistant Klebsiella pneumoniae Bacteremia. Antimicrob Agents Chemother. 2017;61:e00883-e917.
Krapp F, Grant JL, Sutton SH, Ozer EA, Barr VO. Treating complicated carbapenem-resistant enterobacteriaceae infections with ceftazidime/avibactam: a retrospective study with molecular strain characterisation. Int J Antimicrob Agents. 2017;49:770–3.
Castón JJ, Lacort-Peralta I, Martín-Dávila P, Loeches B, Tabares S, Temkin L, et al. Clinical efficacy of ceftazidime/avibactam versus other active agents for the treatment of bacteremia due to carbapenemase-producing Enterobacteriaceae in hematologic patients. Int J Infect Dis. 2017;59:118–23.
Temkin E, Torre-Cisneros J, Beovic B, Benito N, Giannella M, Gilarranz R, et al. Ceftazidime–avibactam as Salvage Therapy for Infections Caused by Carbapenem-Resistant Organisms. Antimicrob Agents Chemother. 2017;61
King M, Heil E, Kuriakose S, Bias T, Huang V, El-Beyrouty C, et al. Multicenter Study of Outcomes with Ceftazidime–avibactam in Patients with Carbapenem-Resistant Enterobacteriaceae Infections. Antimicrob Agents Chemother. 2017;61
Shields RK, Nguyen MH, Chen L, Press EG, Kreiswirth BN, Clancy CJ. Pneumonia and renal replacement therapy are risk factors for ceftazidime–avibactam treatment failures and resistance among patients with carbapenem-resistant Enterobacteriaceae infections. Antimicrob Agents Chemother 2018; 62. pii: e02497–17
Sousa A, Pérez-Rodríguez MT, Soto A, Rodríguez L, Pérez-Landeiro A, Martínez-Lamas L, et al. Effectiveness of ceftazidime/avibactam as salvage therapy for treatment of infections due to OXA-48 carbapenemase-producing Enterobacteriaceae. J Antimicrob Chemother. 2018;73:3170–5.
De la Calle C, Rodríguez O, Morata L, Marco F, Cardozo C, García-Vidal C, et al. Clinical characteristics and prognosis of infections caused by OXA-48 carbapenemase-producing Enterobacteriaceae in patients treated with ceftazidime–avibactam. Int J Antimicrob Agents. 2019;53:520–4.
Ackley R, Roshdy D, Meredith J, Minor S, Anderson WE, Capraro GA, Polk C. Meropenem–vaborbactam versus ceftazidime–avibactam for treatment of carbapenem-resistant enterobacteriaceae infections. Antimicrob Agents Chemother. 2020;64:e02313-e2319.
van Duin D, Lok JJ, Earley M, Cober E, Richter SS, Perez F, et al. Antibacterial Resistance Leadership Group. Colistin Versus Ceftazidime–avibactam in the Treatment of Infections Due to Carbapenem-Resistant Enterobacteriaceae. Clin Infect Dis. 2018; 66:163–171
Guimarães T, Nouér SA, Martins RCR, Perdigão Neto LV, Martins WMBS, et al. Ceftazidime/avibactam as salvage therapy for infections caused by Enterobacteriales co-resistant to carbapenems and polymyxins. Antimicrob Agents Chemother. 2019;63:e00528-e619.
Onorato L, Di Caprio G, Signoriello S, Coppola N. Efficacy of ceftazidime/avibactam in monotherapy or combination therapy against carbapenem-resistant Gram-negative bacteria: A meta-analysis. Int J Antimicrob Agents. 2019;54:735–40.
Wunderink RG, Giamarellos-Bourboulis EJ, Rahav G, Mathers AJ, Bassetti M, Vazquez J, et al. Effect and safety of meropenem–vaborbactam versus best-available therapy in patients with carbapenem-resistant Enterobacteriaceae infections: The TANGO II Randomized Clinical Trial. Infect Dis Ther. 2018;7:439–55.
Motsch J, Murta de Oliveira C, Stus V, Köksal I, Lyulko O, Boucher HW, et al. RESTORE-IMI 1: A multicenter, randomized, double-blind trial comparing efficacy and safety of imipenem/relebactam vs colistin plus imipenem in patients with imipenem-nonsusceptible bacterial infections. Clin Infect Dis. 2020;70:1799–1808.
Gaibani P, Lewis RE, Volpe SL, Giannella M, Campoli C, Landini MP, et al. In vitro interaction of ceftazidime–avibactam in combination with different antimicrobials against KPC-producing Klebsiella pneumoniae clinical isolates. Int J Infect Dis. 2017;65:1–3.
Shields RK, Nguyen MH, Hao B, Kline EG, Clancy CJ. Colistin Does Not Potentiate Ceftazidime–avibactam Killing of Carbapenem-Resistant Enterobacteriaceae In Vitro or Suppress Emergence of Ceftazidime–avibactam Resistance. Antimicrob Agents Chemother. 2018;62
Chew KL, Tay MKL, Cheng B, Lin RTP, Octavia S, Teo JWP. Aztreonam-Avibactam Combination Restores Susceptibility of Aztreonam in Dual-Carbapenemase-Producing Enterobacteriaceae. Antimicrob Agents Chemother. 2018; 27;62:18
Biagi M, Wu T, Lee M, Patel S, Butler D, Wenzler E. Searching for the Optimal Treatment for Metallo- and Serine-β-Lactamase Producing Enterobacteriaceae: Aztreonam in Combination with Ceftazidime–avibactam or Meropenem–vaborbactam. Antimicrob Agents Chemother. 2019;63:e01426-e1519.
Jayol A, Nordmann P, Poirel L, Dubois V. Ceftazidime/avibactam alone or in combination with aztreonam against colistin-resistant and carbapenemase-producing Klebsiella pneumoniae. J Antimicrob Chemother. 2018;73:542–4.
Nath S, Moussavi F, Abraham D, Landman D, Quale J. In vitro and in vivo activity of single and dual antimicrobial agents against KPC-producing Klebsiella pneumoniae. J Antimicrob Chemother. 2018;73:431–6.
Göttig S, Frank D, Mungo E, Nolte A, Hogardt M, Besier S, Wichelhaus TA. Emergence of ceftazidime/avibactam resistance in KPC-3-producing Klebsiella pneumoniae in vivo. J Antimicrob Chemother. 2019;74:3211–6.
Ojdana D, Gutowska A, Sacha P, Majewski P, Wieczorek P, Tryniszewska E. Activity of ceftazidime–avibactam alone and in combination with ertapenem, fosfomycin, and tigecycline against carbapenemase-producing Klebsiella pneumoniae. Microb Drug Resist. 2019;25:1357–64.
Mikhail S, Singh NB, Kebriaei R, Rice SA, Stamper KC, Castanheira M, Rybak MJ. Evaluation of the Synergy of Ceftazidime–avibactam in Combination with Meropenem, Amikacin, Aztreonam, Colistin, or Fosfomycin against Well-Characterized Multidrug-Resistant Klebsiella pneumoniae and Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2019;63. pii: e00779–19
Borjan J, Meyer KA, Shields RK, Wenzler E. Activity of ceftazidime–avibactam alone and in combination with polymyxin B against carbapenem-resistant Klebsiella pneumoniae in a tandem in vitro time-kill/in vivo Galleria mellonella survival model analysis. Int J Antimicrob Agents. 2020;55:105852.
Liu J, Gefen O, Ronin I, Bar-Meir M, Balaban NQ. Effect of tolerance on the evolution of antibiotic resistance under drug combinations. Science. 2020;367:200–4.
Shields RK, Clancy CJ, Press EG, Nguyen MH. Aminoglycosides for Treatment of bacteremia due to carbapenem-resistant Klebsiella pneumoniae. Antimicrob Agents Chemother. 2016;60:3187–92.
Wang Y, Wang J, Wang R, Cai Y. Resistance to ceftazidime–avibactam and underlying mechanisms. J Glob Antimicrob Resist. 2020;22:18–27.
Nichols WW, Stone GG, Newell P, Broadhurst H, Wardman A, MacPherson M, et al. Ceftazidime- Avibactam Susceptibility Breakpoints against Enterobacteriaceae and Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2018;62:e02590-e2617.
Gaudereto JJ, Perdigão Neto LV, Leite GC, Ruedas Martins R, Boas do Prado GV, Rossi F, et al. Synergistic Effect of Ceftazidime–avibactam with Meropenem against Panresistant, Carbapenemase-Harboring Acinetobacter baumannii and Serratia marcescens Investigated Using Time-Kill and Disk Approximation Assays. Antimicrob Agents Chemother. 2019;63. pii: e02367–18
Shields RK, Chen L, Cheng S, Chavda KD, Press EG, Snyder A, et al. Emergence of Ceftazidime–avibactam Resistance Due to Plasmid-Borne blaKPC-3 Mutations during Treatment of Carbapenem-Resistant Klebsiella pneumoniae Infections. Antimicrob Agents Chemother. 2017;61
Marshall S, Hujer AM, Rojas LJ, Papp-Wallace KM, Humphries RM, Spellberg B et al. Can Ceftazidime–avibactam and Aztreonam Overcome β-Lactam Resistance Conferred by Metallo-β-Lactamases in Enterobacteriaceae? Antimicrob Agents Chemother. 2017;61. pii: e02243–16.
Khan AU, Maryam L, Zarrilli R. Structure, Genetics and Worldwide Spread of New Delhi Metallo-β-lactamase (NDM): a threat to public health. BMC Microbiol. 2017;17:101.
Meini S, Tascini C, Cei M, Sozio E, Rossolini GM. AmpC β-lactamase-producing Enterobacterales: what a clinician should know. Infection. 2019;47:363–75.
Funding
No funding has been received for this work. This study was carried out as part of our routine work.
Author information
Authors and Affiliations
Corresponding author
Additional information
The original online version of this article was revised: The presentation of Table 1 was incorrect. The corrected table is given below.
Rights and permissions
About this article
Cite this article
Meini, S., Viaggi, B. & Tascini, C. Mono vs. combo regimens with novel beta-lactam/beta-lactamase inhibitor combinations for the treatment of infections due to carbapenemase-producing Enterobacterales: insights from the literature. Infection 49, 411–421 (2021). https://doi.org/10.1007/s15010-021-01577-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-021-01577-x