Abstract
Purpose
To assess the relationship between high vancomycin minimum inhibitory concentrations (MIC), in patients with methicillin-resistant Staphylococcus aureus bacteremia (MRSAB), and both mortality and complicated bacteremia.
Methods
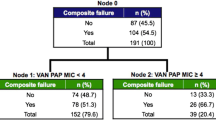
Embase, Medline, EBM, Scopus and Web of Science were searched for studies published from January 1st 2014 to February 29th 2020. “High” vancomycin MIC cut off was defined as ≥ 1.5 mg/L. Three referees independently reviewed studies that compared outcomes in patients with MRSAB stratified by vancomycin MIC. Subgroup analyses were performed for rates of mortality and complicated bacteremia.
Results
A total of 13 studies with 2089 patients were included. Overall, mortality was 27.7% and 23.3% in the high and low vancomycin MIC group, respectively. No significant difference was found between vancomycin MIC groups for overall mortality, in-hospital mortality, late mortality, persistent bacteremia, severe sepsis or septic shock, acute renal failure, septic emboli or endocarditis, and osteomyelitis or septic arthritis. Early mortality was significantly associated with low vancomycin MIC. Mortality in studies using broth microdilution method (BMD) and need for mechanical ventilation were significantly associated with high vancomycin MIC.
Conclusion
Overall mortality and complicated bacteremia were not significantly associated with high vancomycin MICs in a patient with MRSAB. Randomized controlled trials to assess the utility of vancomycin MIC values in predicting mortality and other adverse clinical outcomes are warranted.




Similar content being viewed by others
Availability of data and materials
Not applicable.
Code availability
Not applicable.
References
Hassoun A, Linden PK, Friedman B. Incidence, prevalence, and management of MRSA bacteremia across patient populations-a review of recent developments in MRSA management and treatment. Crit Care. 2017;21:211.
Boucher HW, Corey GR. Epidemiology of methicillin-resistant Staphylococcus aureus. Clin Infect Dis. 2008;46:S344–9.
Yasmin M, El Hage H, Obeid R, El Haddad H, Zaarour M, Khalil A. Epidemiology of bloodstream infections caused by methicillin-resistant Staphylococcusaureus at a tertiary care hospital in New York. Am J Infect Control. 2016;44:41–6.
Hawkshead JJ 3rd, Patel NB, Steele RW, Heinrich SD. Comparative severity of pediatric osteomyelitis attributable to methicillin-resistant versus methicillin-sensitive Staphylococcusaureus. J Pediatr Orthop. 2009;29:85–90.
Chen CP, Liu MF, Lin CF, Lin SP, Shi ZY. The association of molecular typing, vancomycin MIC, and clinical outcome for patients with methicillin-resistant Staphylococcusaureus infections. J Microbiol Immunol Infect. 2017;50:619–26.
Zhang Y, Wang Y, Van Driel ML, McGuire TM, Zhang T, Dong Y, et al. Network meta-analysis and pharmacoeconomic evaluation of antibiotics for the treatment of patients infected with complicated skin and soft structure infection and hospital-acquired or ventilator-associated pneumonia. Antimicrobial Resist Infect Control. 2019;8:72.
Hasan R, Acharjee M, Noor R. Prevalence of vancomycin resistant Staphylococcusaureus (VRSA) in methicillin resistant S. aureus (MRSA) strains isolated from burn wound infections. Ci Ji Yi Xue Za Zhi. 2016;28:49–53.
Habib A, Irfan M, Baddour LM, Le KY, Anavekar NS, Lohse CM, et al. Impact of prior aspirin therapy on clinical manifestations of cardiovascular implantable electronic device infections. Europace. 2013;15:227–35.
Wang JL, Wang JT, Sheng WH, Chen YC, Chang SC. Nosocomial methicillin-resistant Staphylococcusaureus (MRSA) bacteremia in Taiwan: mortality analyses and the impact of vancomycin, MIC = 2 mg/L, by the broth microdilution method. BMC Infect Dis. 2010;10:159.
Holmes NE, Turnidge JD, Munckhof WJ, Robinson JO, Korman TM, O’Sullivan MV, et al. Antibiotic choice may not explain poorer outcomes in patients with Staphylococcusaureus bacteremia and high vancomycin minimum inhibitory concentrations. J Infect Dis. 2011;204:340–7.
Yoon YK, Park DW, Sohn JW, Kim HY, Kim YS, Lee CS, et al. Multicenter prospective observational study of the comparative efficacy and safety of vancomycin versus teicoplanin in patients with health care-associated methicillin-resistant Staphylococcusaureus bacteremia. Antimicrob Agents Chemother. 2014;58:17–324.
van Hal SJ, Jones M, Gosbell IB, Paterson DL. Vancomycin heteroresistance is associated with reduced mortality in ST239 methicillin-resistant Staphylococcusaureus blood stream infections. PLoS ONE. 2011;6:e21217.
Kalil AC, Van Schooneveld TC, Fey PD, Rupp ME. Association between vancomycin minimum inhibitory concentration and mortality among patients with Staphylococcusaureus bloodstream infections: a systematic review and meta-analysis. JAMA. 2014;312:1552–64.
Liu C, Bayer A, Cosgrove SE, Daum RS, Fridkin SK, Gorwitz RJ, et al. Clinical practice guidelines by the infectious diseases society of america for the treatment of methicillin-resistant Staphylococcusaureus infections in adults and children. Clin Infect Dis. 2011;52:e18-55.
Marik PE, Taeb AM. SIRS, qSOFA and new sepsis definition. J Thorac Dis. 2017;9:943–5.
Lo CK-L, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. 2014;14:45.
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–94.
DerSimonian R, Laird N. Meta-analysis in clinical trials revisited. Contemp Clin Trials. 2015;45:139–45.
Page MJ, Shamseer L, Tricco AC. Registration of systematic reviews in PROSPERO: 30,000 records and counting. Syst Rev. 2018;7:32.
Kale-Pradhan PB, Mariani NP, Wilhelm SM, Johnson LB. Meta-analysis: vancomycin treatment failures for MRSA bacteremia based on MIC determined by E-test. J Pharm Technol. 2016;32:65–70.
McCallum N, Karauzum H, Getzmann R, Bischoff M, Majcherczyk P, Berger-Bächi B, et al. In vivo survival of teicoplanin-resistant Staphylococcusaureus and fitness cost of teicoplanin resistance. Antimicrob Agents Chemother. 2006;50(7):2352–60.
Peleg AY, Monga D, Pillai S, Mylonakis E, Moellering RC Jr, Eliopoulos GM. Reduced susceptibility to vancomycin influences pathogenicity in Staphylococcusaureus infection. J Infect Dis. 2009;199:532–6.
Rybak M, Lomaestro B, Rotschafer JC, Moellering R Jr, Craig W, Billeter M, et al. Therapeutic monitoring of vancomycin in adult patients: a consensus review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists. Am J Health Syst Pharm. 2009;66:82–98.
Moise PA, Forrest A, Bhavnani SM, Birmingham MC, Schentag JJ. Area under the inhibitory curve and a pneumonia scoring system for predicting outcomes of vancomycin therapy for respiratory infections by Staphylococcusaureus. Am J Health Syst Pharm. 2000;57:S4-9.
Cresti A, Chiavarelli M, Scalese M, Nencioni C, Valentini S, Guerrini F, et al. Epidemiological and mortality trends in infective endocarditis, a 17-year population-based prospective study. Cardiovasc Diagn Ther. 2017;7:27–35.
Gasch O, Camoez M, Dominguez MA, Padilla B, Pintado V, Almirante B, et al. Predictive factors for mortality in patients with methicillin-resistant Staphylococcusaureus bloodstream infection: impact on outcome of host, microorganism and therapy. Clin Microbiol Infect. 2013;19:1049–57.
van Hal SJ, Lodise TP, Paterson DL. The clinical significance of vancomycin minimum inhibitory concentration in Staphylococcusaureus infections: a systematic review and meta-analysis. Clin Infect Dis. 2012;54:755–71.
Jacob JT, DiazGranados CA. High vancomycin minimum inhibitory concentration and clinical outcomes in adults with methicillin-resistant Staphylococcusaureus infections: a meta-analysis. Int J Infect Dis. 2013;17:e93–100.
Chen SY, Hsueh PR, Chiang WC, Huang EP, Lin CF, Chang CH, et al. Predicting high vancomycin minimum inhibitory concentration isolate infection among patients with community-onset methicillin-resistant Staphylococcusaureus bacteraemia. J Infect. 2014;69:259–65.
Ye C, Wang Z, Hu Y, Deng C, Liao L, Sun L, et al. Systematic review and meta-analysis of the efficacy and safety of vancomycin combined with β-lactam antibiotics in the treatment of methicillin-resistant Staphylococcusaureus bloodstream infections. J Global Antimicrob Resist. 2020;23:303–10.
Kan LP, Lin JC, Chiu SK, Yeh YC, Lin TY, Yang YS, et al. Methicillin-resistant Staphylococcusaureus bacteremia in hemodialysis and nondialysis patients. J Microbiol Immunol Infect. 2014;47:15–22.
Wingler MJB, Childress D, Maldonado RA. Comparison of vancomycin treatment failures for methicillin-resistant Staphylococcusaureus bacteremia stratified by minimum inhibitory concentration. J Pharm Technol. 2019;35(5):203–7.
Watkins RR, Lemonovich TL, File TM Jr. An evidence-based review of linezolid for the treatment of methicillin-resistant Staphylococcusaureus (MRSA): place in therapy. Core Evid. 2012;7:131–43.
Abdelhady W, Bayer AS, Seidl K, Nast CC, Kiedrowski MR, Horswill AR, et al. Reduced vancomycin susceptibility in an in vitro catheter-related biofilm model correlates with poor therapeutic outcomes in experimental endocarditis due to methicillin-resistant Staphylococcusaureus. Antimicrob Agents Chemother. 2013;57:1447–54.
Aminzadeh Z, Yadegarynia D, Fatemi A, Tahmasebian Dehkordi E, Azad AS. Vancomycin minimum inhibitory concentration for methicillin-resistant Staphylococcusaureus infections; is there difference in mortality between patients? Jundishapur J Microbiol. 2014;7:e12831.
Wong H, Watt C, Elsayed S, John M, Johnson G, Katz K, et al. Characterization of methicillin-resistant Staphylococcusaureus isolates from patients with persistent or recurrent bacteremia. Can J Infect Dis Med Microbiol. 2014;25:83–6.
Lee HY, Chen CL, Liu SY, Yan YS, Chang CJ, Chiu CH. Impact of molecular epidemiology and reduced susceptibility to glycopeptides and daptomycin on outcomes of patients with methicillin-resistant Staphylococcusaureus Bacteremia. PLoS ONE. 2015;10:e0136171.
Shoji H, Maeda M, Shirakura T, Takuma T, Ugajin K, Fukuchi K, et al. More accurate measurement of vancomycin minimum inhibitory concentration indicates poor outcomes in meticillin-resistant Staphylococcusaureus bacteraemia. Int J Antimicrob Agents. 2015;46:532–7.
Hos NJ, Jazmati N, Stefanik D, Hellmich M, AlSael H, Kern WV, et al. Determining vancomycin Etest MICs in patients with MRSA bloodstream infection does not support switching antimicrobials. J Infect. 2017;74:248–59.
Moise PA, Culshaw DL, Wong-Beringer A, Bensman J, Lamp KC, Smith WJ, et al. Comparative effectiveness of vancomycin versus daptomycin for MRSA bacteremia with vancomycin MIC >1 mg/L: a multicenter evaluation. Clin Ther. 2016;38:16–30.
Fernández-Hidalgo N, Ribera A, Larrosa MN, Viedma E, Origüen J, de Alarcón A, et al. Impact of Staphylococcusaureus phenotype and genotype on the clinical characteristics and outcome of infective endocarditis. A multicentre, longitudinal, prospective, observational study. Clin Microbiol Infect. 2018;24:985–91.
Adani S, Bhowmick T, Weinstein MP, Narayanan N. Impact of vancomycin MIC on clinical outcomes of patients with methicillin-resistant Staphylococcusaureus bacteremia treated with vancomycin at an institution with suppressed MIC reporting. Antimicrob Agents Chemother. 2018;62:e02512-e2517.
Ruiz J, Ramirez P, Concha P, Salavert-Lletí M, Villarreal E, Gordon M, et al. Vancomycin and daptomycin minimum inhibitory concentrations as a predictor of outcome of methicillin-resistant Staphylococcusaureus bacteraemia. J Glob Antimicrob Resist. 2018;14:141–4.
Kim T, Chong YP, Park KH, Bang KM, Park SJ, Kim SH, Jeong JY, Lee SO, Choi SH, Woo JH, Kim YS. Clinical and microbiological factors associated with early patient mortality from methicillin-resistant Staphylococcusaureus bacteremia. Korean J Intern Med. 2019;34:184–94.
Funding
The authors are extremely grateful for the philanthropic support provided by a gift from Eva and Gene Lane (L.M.B.) which was paramount in our work to advance the science of cardiovascular infections, which has been an ongoing focus of the investigation at Mayo Clinic for over 60 years.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Larry M. Baddour, MD reports Boston Scientific, consultant duties; UpToDate, royalty payments (authorship duties); Botanix Pharmaceuticals, consulting duties; Roivant Sciences Inc., consultant duties. Dr. M. Rizwan Sohail reports receiving funds from TYRX Inc. and Medtronic for prior research unrelated to this study administered according to a sponsored research agreement between Mayo Clinic and study sponsor that prospectively defined the scope of the research effort and corresponding budget; and honoraria/consulting fees from Medtronic Inc., Philips, and Aziyo Biologics, Inc. Research Grant: Medtronic (significant—$40 K), Honoraria: Medtronic (significant $20 K), and Aziyo Biologics (modest $5 K). The other authors report no financial support or conflict of interest.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ishaq, H., Tariq, W., Talha, K.M. et al. Association between high vancomycin minimum inhibitory concentration and clinical outcomes in patients with methicillin-resistant Staphylococcus aureus bacteremia: a meta-analysis. Infection 49, 803–811 (2021). https://doi.org/10.1007/s15010-020-01568-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-020-01568-4