Abstract
Purpose
This study aimed to determine the proportion of people living with HIV with anti-SARS-CoV-2 IgG antibodies in a sample from a large single HIV center in Munich, Germany, after the first phase of the coronavirus pandemic and to infer the prevalence of SARS-CoV-2 co-infection in people living with HIV.
Methods
Prospective sub-study of the ongoing ArcHIV cohort between May and July 2020. Anti-SARS-CoV-2 IgG antibodies were measured using the recomWell SARS-CoV-2 IgG ELISA (Mikrogen, Neuried, Germany); positive and borderline results were re-tested using the recomLine SARS-CoV-2 IgG immunoassay (Mikrogen, Neuried, Germany). Demographic and medical data were extracted from the electronic patient files.
Results
Overall, 500 people living with HIV were included in the study (83% male, median age 51 years). Three participants had been diagnosed with COVID-19 prior to study inclusion. Of those, nine were confirmed positive for SARS-CoV-2 IgG antibodies, resulting in an estimated seroprevalence (accounting for sensitivity and specificity of the test) of 1.5% (CI 95%: 0.69; 3.13) for the entire study sample, and 2.2% (CI 95%: 1.1; 3.9) for the subset of the Munich citizens. There were no marked differences for people living with HIV with and without SARS-CoV-2 co-infection.
Conclusion
The seroprevalence of SARS-CoV-2 co-infection in people living with HIV as found in our study does not seem to exceed previous reports from general populations of ‘hot-sport’ areas; comparative data from the Munich population can be expected to be published soon. Our data also highlight, once more, the need to do confirmatory testing on positive samples to minimize the impact of false-positive results.
Similar content being viewed by others
Introduction
The global spread of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) beginning in December 2019 was declared a pandemic by the World Health Organization (WHO) in early 2020 and has infected more than 35,000,000 people worldwide and caused more than 1,000,000 deaths as of October 2020 [1]. The Munich area played a particular role in the global spread of the disease, with the first patient—the first in Germany—being diagnosed with the coronavirus disease 2019 (COVID-19) as early as January 2020, therefore becoming an early ‘hotspot’ of the disease outside China. It was also here that first evidence for the transmission of the disease via asymptomatic carriers emerged [2], which had not been considered before. While the risk of transmission was generally assumed to be high in SARS-CoV-2, it became clear that certain risk factors might contribute to acquisition or a more severe course of the disease: male sex, age, and pulmonary and cardiovascular comorbidities have been identified as potential risk factors [3], among others. In contrast, the role of HIV-1 infection remains controversial due to the lack of data on this subject. As an immunodeficiency disease, HIV infection could be associated with a higher risk of acquiring COVID-19 and/or worse outcomes. However, due to the high efficacy of current antiretroviral therapies (ART), most people living with HIV (PLWH) are virologically suppressed and often show normal or only slightly diminished CD4 cell counts. Furthermore, several antiretroviral agents directed against the reverse transcriptase (RT) exhibit structural analogy to the novel nucleotide analogue remdesivir that has demonstrated moderate positive effects on the course of COVID-19 [4]. However, data on potential effects of modern ART regimens on the course of COVID-19 are inconclusive [5,6,7]. Based on current knowledge, it is hence unclear if data about the prevalence of SARS-CoV-2 infection from general populations can be extrapolated to PLWH. Better understanding would yet be important to obtain an impression about a potential contribution of HIV to an excess risk of SARS-CoV-2 co-infection in PLWH.
The seroprevalence, defined as a prevalence derived from the number of positive serologic tests in a representative study sample after accounting for sensitivity and specificity of the test used, can give a deeper insight into the spread of SARS-CoV-2 between the outbreak and a defined time during the pandemic.
Therefore, the objective of our study was to determine the proportion of PLWH with anti-SARS-CoV-2 IgG antibodies in a sample from a large single HIV center in Munich after the first phase of the corona pandemic in Germany. We aimed to establish the prevalence of SARS-CoV-2 co-infection in a population of PLWH at this site and sought to investigate into factors associated with positive SARS-CoV-2 serology.
Methods
This study was performed as a prospective, cross-sectional sub-study of the observational Munich ArcHIV cohort, an ongoing cohort in PLWH in Munich, Germany, with approval of the local ethics committee dating May 28th, 2020. Patients attending the center for routine laboratory controls for chronic HIV-1 infection (with or without treatment) between May 29th and July 15th, 2020 were consecutively asked to participate in the study. There were no exclusion criteria except for the unwillingness or inability to give written informed consent. After obtaining informed consent, an additional 8 ml blood sample was drawn. All patients were asked if they had been diagnosed with SARS-CoV-2 infection before, and if they were in contact with a person with confirmed SARS-CoV-2 infection. Physicians were asked to determine the ethnicity of each participating patient. Data on demographics, laboratory results, and ART were obtained from the electronic patient files. Anti-SARS-CoV-2 IgG antibodies were determined using the recomWell SARS-CoV-2 IgG ELISA (Mikrogen, Neuried, Germany). Results of the ELISA were reported as ‘positive’, ‘negative’, or ‘borderline’. ‘Positive’ and ‘borderline’ results were re-tested using the recomLine SARS-CoV-2 IgG immunoassay (Mikrogen, Neuried, Germany). The specificity of this sequential approach was found to be at least 99.5% [8], while the sensitivity is determined by the initial test (recomWell), that was found to have a sensitivity of 86.4% [9]. Results from re-testing of the initially ‘positive’ or ‘borderline’ samples using two additional ELISA test systems (Euroimmun [Lübeck, Germany] and Roche [Basel, Switzerland]) were used for a sensitivity analysis; only those samples with a positive result in all tests were used for a very conservative estimation of anti-SARS-CoV-2 antibody prevalence. The specificity for this approach when estimating the population prevalence was assumed to be 100%.
Other predefined variables of interest in the study were age, sex, ethnicity, HIV-RNA level, and CD4 cell count. The primary outcome was the seroprevalence of SARS-CoV-2 co-infection in PLWH, approximated by the number of PLWH tested positive for anti-SARS-CoV-2 IgG antibodies (in both, the recomWell and the recomLine test):
Assuming that the number of PLWH tested positive is the sum of ‘true’ positive (T+ D+) and ‘false’ positive (T+ D) results, with conditional probabilities p(T D) = sensitivity and p(T D) = 1-specificity, the.
seroprevalence was estimated using the following equation derived from Bayes’ theorem:
where SP = seroprevalence, n = number of patients tested, npos = number of patients tested positive, sens = sensitivity of the test, and spec = specificity of the test. Exact 95% confidence intervals (CI 95%) were calculated as described by Clopper and Pearson.
As many PLWH at the study site are living outside Munich, the analyses were performed for the overall study sample as well as only for those participants living in Munich separately. To investigate possible bias due to the study design, a comparison to the overall population of PLWH under permanent medical care of the study site (referred to as PLWH population subsequently) was performed, including all PLWH attending the study site within the last year prior to termination of the current study.
As enrollment of 500 PLWH would allow for detection of a seroprevalence of up to 15% with a precision of a maximum of about 3%. We therefore planned to enroll 500 PLWH. Statistical analysis was performed in an explorative manner using R 4.0.0. Descriptive statistics were performed using means with standard deviations (SD) (for the comparisons of the study sample with the overall PLWH population of the study site) or medians with interquartile ranges (IQR) (for the comparison of PLWH with positive and negative SARS-CoV-2 serology) for continuous variables; frequencies (absolute and relative) were used for categorical variables. T test and Mann–Whitney test were used for comparison of continuous variables, and Fisher’s exact test for categorical variables. Unless otherwise declared, p values < 0.05 were considered to be statistically significant without adjusting for multiple testing. The manuscript was written in accordance with the ‘Strengthening the Reporting of Observational Studies in Epidemiology’ (STROBE) statement [10].
Results
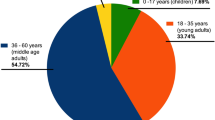
In total, 500 PLWH were included in this study. The baseline characteristics of the study sample together with a comparison to the overall PLWH population can be found in Table 1. 75.2%, 6.6%, 29.4%, and 10% of the study sample were on integrase inhibitor-, protease inhibitor-, non-nucleoside reverse transcriptase inhibitor-, and TDF-containing regimens, respectively; 172 (34.4%) were on a two-drug regimen. In the study sample, 437 (87.4%) and 28 (5.6%) were of Caucasian and African ethnicity, respectively. Three patients (0.6%) reported having been tested positive for SARS-CoV-2 before (all of them living in Munich) and 29 (5.8%) reported prior contact to a person with confirmed COVID-19.
Entire study sample
Overall, 22 PLWH were tested positive for anti-SARS-CoV-2 IgG antibodies using the recomWell test, with nine confirmed to be positive using the recomLine immunoassay, corresponding to a fraction of positive test results in the study sample of 0.018 (CI 95%:0.008; 0.034). These results showed high agreement with test results obtained from the alternative confirmation tests (Fig. 2). A comparison of PLWH with positive and negative serology can be found in Table 2. From the nine PLWH confirmed positive, only two had been diagnosed with COVID-19 before (22.2%); one additional subject that reported positive testing for COVID-19 before was found to be antibody negative.
Assuming a sensitivity of 86.4% and a specificity of 99.5% (using the two-step approach), the estimated seroprevalence in a PLWH population as represented in our study was 1.5% (CI 95%: 0.7; 3.1).
Munich subset of the study sample
A subgroup analysis was performed for the Munich residents (n = 292). Within Munich, 13 PLWH were tested positive using the recomWell test (fraction of positive results: 0.045), with seven confirmed positive tests in the recomLine, corresponding to a fraction of 0.024 (CI 95%: 0.010; 0.049) of positive test results from the Munich study sample.
Assuming a sensitivity of 86.4% and a specificity of 99.5%, the estimated seroprevalence in a PLWH population in Munich as represented in our study was 2.2% (CI 95%: 1.1; 3.9). The geographic representativeness of the Munich study sample when compared to all PLWH from Munich in clinical care at the study site is shown in Fig. 1. All three study participants with confirmed history of COVID-19 were living in Munich, therefore, the proportion of PLWH tested positive (by means of PCR from oro-pharyngeal swabs) in the Munich sample was 0.010, while the city of Munich reported a proportion of 0.004 (6964 cases tested positive in a population of 1,561,720 residents) at the end of our study (p = 0.142).
Comparison of the percentage of PLWH in each district from (a) the study sample and (b) the overall PLWH population from the study site in Munich. Red dots in (a) are indicating the residence of PLWH with confirmed positive tests for anti-SARS-CoV-2 antibodies in the study sample. Numbers in (b) are referring to the different districts
Sensitivity analysis
To account for the variability of results according to the choice of the confirmatory test, for a sensitivity analysis, only those samples that were positive for anti-SARS-CoV-2 antibodies in all of the three confirmatory tests (i.e., the recomLine SARS-CoV-2 IgG immunoassay (Mikrogen) and the ELISA test systems of Euroimmun [Lübeck, Germany] and Roche [Basel, Switzerland]) were considered as ‘truly’ positive (Fig. 2). This approach resulted in six positive tests and therefore a prevalence of 1.4% (CI95: 0.4; 2.6). For the Munich study sample, this resulted in five positive tests and therefore a prevalence of 2.0% (CI95: 0.6; 4.0).
Results of the re-test of the initially positive (n = 22) or borderline (n = 8) results in the recomWellassay. While 27 tests yielded in positive results, two were found to be borderline in re-testing, with another one being negative. For the primary endpoint, all confirmed positive results in the recomLine test were considered’truly’ positive (highlighted in gray)
Discussion
To the best of our knowledge, we herein present the first data on the seroprevalence of SARS-CoV-2 co- infection in a representative sample of PLWH, derived from a large single HIV center in Munich, Germany, one of the first European ‘hotspots’ in the SARS-CoV-2 pandemic outside China. Based on the number of confirmed positive test results (n = 9), the seroprevalence of SARS-CoV-2 co-infection in a population of PLWH as represented by the sample from our center is estimated to be 1.5% (CI 95%: 0.7; 3.1).
As many of the participating PLWH were not from Munich, the subset with residency in Munich was analyzed separately for a more homogeneous baseline risk of acquiring SARS-CoV-2 co-infection. From the Munich-only study sample, seven PLWH had confirmed positive tests for SARS-CoV-2 antibodies, resulting in a seroprevalence of 2.2% (CI 95%: 1.1; 3.9). The estimates for the overall and the Munich prevalence in PLWH were robust in sensitivity analysis, which used a conservative approach for the underlying specificity. The estimated prevalence for the Munich population of PLWH exceeded the cumulative prevalence derived from the number of reported cases for the city substantially: in Munich, at the time of the end of our study, overall 6964 people out of a population of 1,561,720 had been tested positive by SARS-CoV-2 nucleic acid amplification technique, resulting in a cumulative prevalence of only 0.45% [11]. Yet, this finding is neither surprising nor attributable to HIV infection. This discrepancy has been found before, with the seroprevalence being more than tenfold higher than estimated by the confirmed cases [12, 13], inherent to the different methods and underlying motivations of capturing (cumulative) prevalence. Of note, among all 500 PLWH included in this study, three had been diagnosed with COVID-19 (by PCR) before (two with positive, one with negative serology, all living in Munich). Therefore, deriving a cumulative prevalence from positive swabs in the Munich subset of the sample resulted in 1.0%, which did not differ significantly from the proportion of reported cases within the entire city of Munich (p = 0.142).
While there are no comparative data about the seroprevalence of SARS-CoV-2 infection in the general population of Munich yet, there are limited data from other regions in Germany, some of which were also considered having high infection rates. However, while one study (from convenience sampling from blood donors from different states of Germany) reported a lower proportion of people with SARS-CoV-2 antibodies [14], Streeck and colleagues, who systematically investigated a small German town that became a hotspot area after a ‘super-spreading’ event, reported a proportion as high as 15.5% [12]. However, in the latter study, enormous clustering might limit the generalizability.
When comparing findings from PLWH with positive and negative SARS-CoV-2 serology, there were trends that failed to achieve statistical significance, probably due to the overall low number of events. Therefore, we were not able to identify risk factors for co-infection with SARS-CoV-2 in PLWH.
Our data highlight, once more, the influence of false-positive results in a low-prevalence disease. Using confirmed versus unconfirmed positive samples reduced the proportion of PLWH with SARS-CoV-2 antibodies significantly from 0.044 to 0.018% (p = 0.003). Of note, even though ‘only’ 9 out of 22 being confirmed positive might sound intuitively little, it means that (assuming perfect sensitivity) out of 491 ‘truly’ negative PLWH, 478 were classified correctly as being negative by the initial ‘screening’ test (recomWell), resulting in a specificity of 97.4%. This estimate did not change relevantly when modifying sensitivity over a wide range, going as low as 80% (data not shown). Similarly, using the most conservative approach to estimate the specificity of the sequential approach by only considering samples ‘truely’ positive, that were also confirmed by the two other confirmation tests (n = 7), led to an approximation of the specificity of 99.6%, which is in perfect line with the expectations of the performance [8].
Our study has several limitations. Most importantly, as demonstrated by our results, there can be a high degree of uncertainty with serologic tests, with issues about specificity being of high impact on the overall results in a low-prevalence disease. However, we could address this issue by performing several confirmatory tests as suggested before in this setting [15]. On the other hand, while remaining unaddressed, sensitivity is of less impact under these conditions and might, therefore, not have led to substantial impact on the results for a wide range of assumptions of sensitivity. Adding to the uncertainty of serologic testing, it is important to keep in mind that the sole use of IgG antibodies by the recomWell test, which was used for a pre-selection of ‘positive’ or ‘borderline’ samples, could have missed COVID-19 infections in their early phases. However, at the time the study was carried out, infection rates were low, and therefore, this should not have been of substantial impact on the overall results. On the other hand, not every subject with a history of SARS-CoV-2 infection seems to develop specific antibodies and also at least in some subjects, specific antibodies could disappear as early as 3 months after an infection [16]. The results of our study derived from convenience sampling, limited to PLWH attending the clinic for routine clinical care during a short period of time, which might have resulted in a selection bias. However, comparing the study sample with the overall PLWH population yielded in very similar characteristics (Table 2), and we therefore assume no major bias in our sample. However, it has to be kept in mind that the prevalence in our study sample might be driven by the biggest ‘group’ namely men having sex with men. With the lack of knowledge about differences in prevalence throughout the ‘subgroups’ of the heterogeneous community of PLWH (e.g., people of color, intravenous drug users, and trans people), the estimated prevalence might change with increasing sample size. This was also true for the geographic representativeness within in the Munich study subset (Fig. 1), with the percentage of PLWH in our study sample from each of the Munich neighborhoods being close to the distribution in the overall population of PLWH under permanent medical care at the study site. Unfortunately, we were not able to adequately compare ART status and the distribution of different ART regimens within the PLWH population. Also, ethnicity was not available for the whole PLWH population. It is reasonable to assume overdispersion for our data due to the partly clustered nature (on several levels, from couples and people tested from the same household, to similar exposures within the MSM community or probably within certain ethnic groups) that we did not account for. Given the low overall prevalence, these clusters might though be highly important when establishing the population prevalence. Among the PLWH tested positive, we were, however, not able to detect any kind of obvious clustering.
The generalizability of our data might be limited by a different epidemiology of SARS-CoV-2 infection in different areas in the world, but also within Germany itself. However, it might offer the possibility to compare data from PLWH to a representative sample from Munich as a whole with the results from the prospective Munich COVID-19 cohort (KoCo19) [17], expected to be published soon. This comparison, in turn, could serve as the first of its kind and help us to understand whether or not PLWH are at excess risk of (co-)infection with SARS-CoV-2. However, it has to be clear that in a rapidly evolving pandemic, our results can only be seen as a snapshot and repeated studies are necessary for valid estimates of a cumulative prevalence (Fig. 2).
Conclusion
The seroprevalence of SARS-CoV-2 co-infection in a population of PLWH in a large single HIV center in Munich, Germany, is estimated to be 1.5% based on our results, with a higher prevalence (2.2%) when only considering participants with residency in Munich. In the latter group, three subjects reported having been diagnosed with COVID-19 prior to entering the study (1.0%), which is a proportion that is not significantly different from the proportion reported from the overall Munich population at the same time (0.4%). With the prospect of data on the seroprevalence of SARS-CoV-2 infection from over 3000 random Munich households being available soon from the prospective Munich COVID-19 cohort [17], our data will offer the possibility for a first head-to-head comparison of people living with and without HIV from representative samples of the same city.
Availability of data and materials
Raw data can be made available by the corresponding author upon reasonable request.
References
Johns Hopkins University and Medicine. Covid-19 dashboard by the center for systems science and engineering (csse) at johns hopkins university (jhu). 2020. https://coronavirus.jhu.edu/map.html. Accessed 27 Jul 2020.
Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, Wallrauch C, Zimmer T, Thiel V, Janke C, Guggemos W, et al. Transmission of 2019-ncov infection from an asymptomatic contact in germany. N Engl J Med. 2020;382:970–81.
Zheng Z, Peng F, Xu B, Zhao J, Liu H, Peng J, Li Q, Jiang C, Zhou Y, Liu S, et al. Risk factors of critical & mortal covid-19 cases: a systematic literature review and meta-analysis. J Infect. 2020.
Beigel JH, Tomashek KM, Dodd LE, Mehta AK, Zingman BS, Kalil AC, Hohmann E, Chu HY, Luetkemeyer A, Kline S, et al. Remdesivir for the treatment of covid-19—preliminary report. New England J Med. 2020.
Vizcarra P, Pérez-Elías MJ, Quereda C, Moreno A, Vivancos MJ, Dronda F, Casado JL, Moreno S, Pérez-Elías MJ, Fortún J, Navas E, Quereda C, Dronda F, Campo Del S, López-Vélez R, Reinoso JC, Casado JL, Moreno A, Norman F, Martín-Dávila P, Hermida JM, Molina JAP, Monge B, Pintado V, Serrano-Villar S, Sánchez-Conde M, Chamorro S, Escudero R, Gioia F, Comeche B, Crespillo C, Herrera S,Ron R, Martínez-Sanz J, Pons-Guillén M, Vivancos MJ, Vizcarra P. Description of COVID-19 in HIV-infected individuals: a single-centre, prospective cohort. Lancet HIV. 2020.
Amo Del J , Polo R, Moreno S, Díaz A, Martínez E, Arribas JR, Jarrín I, Hernán MA. Incidence and severity of covid-19 in hiv-positive persons receiving antiretroviral therapy: A cohort study. 2020.
Gervasoni C, Meraviglia P, Riva A, Giacomelli A, Oreni L, Minisci D, Atzori C, Ridolfo A, Cattaneo D. Clinical features and outcomes of hiv patients with coronavirus disease 2019. Clin Infect Dis. 2020.
Diagnostik M. Recomline sars-cov-2 igg. Product Description. 2020.
Stroemer A, Grobe O, Rose R, Fickenscher H, Lorentz T, Krumb- holz A. Diagnostic accuracy of six commercial sars-cov-2 igg/total antibody assays and identification of sars-cov-2 neutralizing antibodies in convalescent sera. medRxiv. 2020.
Elm VonE, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vanden- broucke JP, Initiative S, et al. The strengthening the reporting of observational studies in epidemiology (strobe) statement: guidelines for reporting observational studies. Internat J Surg. 2020;12:1495–499.
Stadtportal de Das MO. Coronavirus-fälle in münchen: Aktuelle zahlen. 2020. https://www.muenchen.de/rathaus/Stadtinfos/Coronavirus-Fallzahlen.html. Accessed 12 Jul 2020.
Streeck H, Schulte B, Kuemmerer B, Richter E, Hoeller T, Fuhrmann C, Bartok E, Dolscheid R, Berger M, Wessendorf L, Eschbach-Bludau M, Kellings A, Schwaiger A, Coenen M, Hoffmann P, Noethen M, Eis-Huebinger A-M, Exner M, Schmithausen R, Schmid M, Kuemmerer B. Infection fatality rate of sars-cov-2 infection in a german community with a super-spreading event. medRxiv. 2020.
Stringhini S, Wisniak A, Piumatti G, AS Azman, Lauer SA, Baysson H, De Ridder D, Petrovic D, Schrempft S, Marcus K, et al. Seroprevalence of anti-sars-cov-2 igg antibodies in geneva, switzerland (serocov-pop): a population-based study. Lancet. 2020.
Fischer B, Knabbe C, Vollmer T. Sars-cov-2 igg seroprevalence in blood donors located in three different federal states, germany, march to June 2020. Eurosurveillance. 2020;25:2001285.
Behrens GMN, Cossmann A, Stankov MV, Schulte B, Streeck H, Förster R, Bosnjak B, Willenzon S, Boeck A-L, Tran AT, et al. Strategic anti- sars-cov-2 serology testing in a low prevalence setting: the covid-19 contact (coco) study in healthcare professionals. Infect Dis Ther. 2020;2:1–13.
Liu A, Wang W, Zhao X, Zhou X, Yang D, Lu M, Lv Y. Disappearance of antibodies to sars-cov-2 in a covid-19 patient after recovery. Clin Microbiol Infect. 2020.
Radon K, Saathoff E, Pritsch M, Noller JMG, Kroidl I, Olbrich L, Thiel V, Diefenbach M, Riess F, Forster F, et al. Protocol of a population-based prospective COVID-19 cohort study munich, germany (koco19). medRxiv. 2020.
Acknowledgements
We thank Mikrogen GmbH (Neuried, Germany) for providing the test kits used in this study and support with confirmatory testing. We thank all employees at MVZ Karlsplatz for the support in conducting the study. We also thank Mrs. Zapf for carrying out the anti-SARS-CoV-2 antibody measurements. We highly thank Dr. Andreas Wieser and Mrs. Heike Fensterseifer for providing the possibility of analysis of the ‘positive’ and ‘borderline’ samples with two additional tests (Euroimmun and Roche).
Funding
Mikrogen GmbH (Neuried, Germany) provided the test kits used in this study and performed confirmatory testing. The funding source was not involved in any other aspects of the study, particularly not in data analysis and interpretation.
Author information
Authors and Affiliations
Consortia
Contributions
SN was engaged in developing the study idea and protocol, recruiting patients, data collection and organization, statistical analysis, writing, and revising the manuscript. FS, SH, KR, AK, and CW were engaged in patient recruitment and revising the manuscript. WM and FT were responsible for laboratory analysis and revising the manuscript. AB and EG was engaged in data collection, organization, preparation, and analysis. CJ and HJ were engaged in developing the study idea and protocol, recruiting patients, writing, and revising the manuscript. EW was engaged in developing the study idea and protocol, data collection and organization, statistical analysis, writing, and revising the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors report no conflicts of interest.
Ethics approval
Approval of the local ethic’s committee (“Ethikkommission der Bayerischen Landesärztekammer”) dating May 28th, 2020 was obtained.
Consent to participate
Written informed consent was obtained from each participant prior to any study-specific measures.
Rights and permissions
About this article
Cite this article
Noe, S., Schabaz, F., Heldwein, S. et al. HIV and SARS-CoV-2 co-infection: cross-sectional findings from a German ‘hotspot’. Infection 49, 313–320 (2021). https://doi.org/10.1007/s15010-020-01564-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-020-01564-8