Abstract
Background
The aim of this study was to analyse temporal changes in the epidemiology of candidemia assessing patient’s characteristics, risk factors, diagnostic management, treatment, and outcome in a tertiary care hospital in South Eastern Germany.
Methods
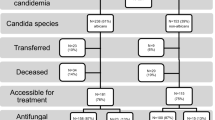
In this retrospective cohort study patients with blood cultures positive for Candida spp. were identified from the microbiological database in the years 2006–2018. A detailed collection of patients’ characteristics was obtained for the time periods 2006–2008 and 2016–2018. Risk factors for survival were analysed in a logistic regression analysis.
Results
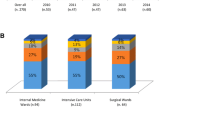
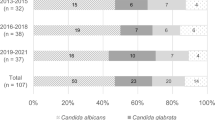
In the years 2006–2018, a total of 465 episodes of candidemia were identified. An increase in candidemia cases was evident in the period of 2016–2018 compared to 2006–2015 and to 2006–2008 in absolute numbers and adjusted to patient-days. C. albicans was responsible for 62.8% of cases in 2006–2008 and 51.2% of all cases in the years 2016–2018, respectively, whereas there was a significant increase of C. glabrata in the latter period (16.3–31.5%). Overall mortality was not significantly different in the two periods. Infectious diseases consultation led to a lower mortality of patients with candidemia and to a higher adherence to guidelines. In multivariate analysis, only complete change or extraction of intravascular indwelling material and female gender were independent predictors for survival.
Conclusion
We observed an increase in candidemia rates and rates of non-albicans spp. over time. A complete change of all catheters and/or indwelling devices improved survival. ID consultation led to a better guideline adherence.


Similar content being viewed by others
References
de Pauw B, Walsh TJ, Donnelly JP, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008;46:1813–21.
Wey SB, Mori M, Pfaller MA, Woolson RF, Wenzel RP. Hospital-acquired candidemia. The attributable mortality and excess length of stay. Arch Intern Med. 1988;148:2642–5.
Gudlaugsson O, Gillespie S, Lee K, et al. Attributable mortality of nosocomial candidemia, revisited. Clin Infect Dis. 2003;37:1172–7.
Arendrup MC, Sulim S, Holm A, et al. Diagnostic issues, clinical characteristics, and outcomes for patients with fungemia. J Clin Microbiol. 2011;49:3300–8.
Cornely OA, Gachot B, Akan H, et al. Epidemiology and outcome of fungemia in a cancer Cohort of the Infectious Diseases Group (IDG) of the European Organization for Research and Treatment of Cancer (EORTC 65031). Clin Infect Dis. 2015;61:324–31.
Messer SA, Jones RN, Fritsche TR. International surveillance of Candida spp and Aspergillus spp: report from the SENTRY Antimicrobial Surveillance Program (2003). J Clin Microbiol. 2006;44:1782–7.
Papadimitriou-Olivgeris M, Spiliopoulou A, Kolonitsiou F, et al. Increasing incidence of candidaemia and shifting epidemiology in favor of Candida non-albicans in a 9-year period (2009–2017) in a university Greek hospital. Infection. 2019;47:209–16.
Kullberg BJ, Arendrup MC. Invasive candidiasis. N Engl J Med. 2015;373:1445–566.
Chow JK, Golan Y, Ruthazer R, et al. Risk factors for albicans and non-albicans candidemia in the intensive care unit. Crit Care Med. 2008;36:1993–8.
Blumberg HM, Jarvis WR, Soucie JM, et al. Risk factors for candidal bloodstream infections in surgical intensive care unit patients: the NEMIS prospective multicenter study The National Epidemiology of Mycosis Survey. Clin Infect Dis. 2001;33:177–86.
Wenzel RP. Nosocomial candidemia: risk factors and attributable mortality. Clin Infect Dis. 1995;20:1531–4.
Cornely OA, Bassetti M, Calandra T, et al. ESCMID* guideline for the diagnosis and management of Candida diseases 2012: non-neutropenic adult patients. Clin Microbiol Infect. 2012;18(Suppl 7):19–37.
Pappas PG, Kauffman CA, Andes DR, et al. Clinical practice guideline for the management of candidiasis: 2016 update by the infectious diseases society of America. Clin Infect Dis. 2016;62:e1–50.
Mellinghoff SC, Hoenigl M, Koehler P, et al. EQUAL Candida Score: an ECMM score derived from current guidelines to measure QUAlity of Clinical Candidaemia Management. Mycoses. 2018;61:326–30.
Arendrup MC, Perlin DS. Echinocandin resistance: an emerging clinical problem? Curr Opin Infect Dis. 2014;27:484–92.
Milazzo L, Peri AM, Mazzali C, et al. Candidaemia observed at a university hospital in Milan (northern Italy) and review of published studies from 2010 to 2014. Mycopathologia. 2014;178:227–41.
Bitar D, Lortholary O, Le Strat Y, et al. Population-based analysis of invasive fungal infections, France, 2001–2010. Emerg Infect Dis. 2014;20:1149–55.
Ishikane M, Hayakawa K, Kutsuna S, Takeshita N, Ohmagari N. The impact of infectious disease consultation in candidemia in a tertiary care hospital in Japan over 12 years. PLoS ONE. 2019;14:e0215996.
Statistische Bundesamt ZB. Diagnosedaten der Krankenhäuser ab 2000. Available at: https://www.gbe-bund.de/oowa921-install/servlet/oowa/aw92/dboowasys921.xwdevkit/xwd_init?gbe.isgbetol/xs_start_neu/&p_aid=3&p_aid=61403017&nummer=550&p_sprache=D&p_indsp=-&p_aid=15744824. Accessed 2 July 2019.
Statistisches Bundesamt. Statistisches Jahrbuch 2018. Available at: https://www.destatis.de/DE/Themen/Querschnitt/Jahrbuch/statistisches-jahrbuch-2018-dl.pdf?__blob=publicationFile&v=5. Accessed 2 July 2019.
Statistische Bundesamt ZB. Case Mix Case Mix Index und Erlösvolumen der vollstationären Patientinnen und Patienten in Krankenhäusern. Available at: https://www.gbe-bund.de/oowa921-install/servlet/oowa/aw92/dboowasys921.xwdevkit/xwd_init?gbe.isgbetol/xs_start_neu/&p_aid=i&p_aid=31681490&nummer=113&p_sprache=D&p_indsp=-&p_aid=43231210. Accessed 2 July 2019.
Colombo AL, de Almeida JN, Slavin MA, Chen SC-A, Sorrell TC. Candida and invasive mould diseases in non-neutropenic critically ill patients and patients with haematological cancer. Lancet Infect Dis. 2017;17:e344–e356356.
Lyon GM, Karatela S, Sunay S, Adiri Y. Antifungal susceptibility testing of Candida isolates from the Candida surveillance study. J Clin Microbiol. 2010;48:1270–5.
Chow JK, Golan Y, Ruthazer R, et al. Factors associated with candidemia caused by non-albicans Candida species versus Candida albicans in the intensive care unit. Clin Infect Dis. 2008;46:1206–13.
Bassetti M, Taramasso L, Nicco E, Molinari MP, Mussap M, Viscoli C. Epidemiology, species distribution, antifungal susceptibility and outcome of nosocomial candidemia in a tertiary care hospital in Italy. PLoS ONE. 2011;6:e24198.
Fischer J, Jung N, Robinson N, Lehmann C. Sex differences in immune responses to infectious diseases. Infection. 2015;43:399–403.
Lahey T, Shah R, Gittzus J, Schwartzman J, Kirkland K. Infectious diseases consultation lowers mortality from Staphylococcus aureus bacteremia. Medicine (Baltimore). 2009;88:263–7.
Bai AD, Showler A, Burry L, et al. Impact of infectious disease consultation on quality of care, mortality, and length of stay in staphylococcus aureus bacteremia: results from a large multicenter cohort study. Clin Infect Dis. 2015;60:1451–61.
Jones TM, Drew RH, Wilson DT, Sarubbi C, Anderson DJ. Impact of automatic infectious diseases consultation on the management of fungemia at a large academic medical center. Am J Health Syst Pharm. 2017;74:1997–2003.
Murri R, Giovannenze F, Camici M, et al. Systematic clinical management of patients with candidemia improves survival. J Infect. 2018;77:145–50.
Pappas PG, Rex JH, Sobel JD, et al. Guidelines for treatment of candidiasis. Clin Infect Dis. 2004;38:161–89.
Menichetti F, Bertolino G, Sozio E, et al. Impact of infectious diseases consultation as a part of an antifungal stewardship programme on candidemia outcome in an Italian tertiary-care. Univ Hosp J Chemother. 2018;30:304–9.
Rieg S, Hitzenbichler F, Hagel S, et al. Infectious disease services: a survey from four university hospitals in Germany. Infection. 2019;47:27–33.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
AM and FHi: travel grants from Gilead Sciences. BS: educational grants from Gilead Sciences. MS: lecture fee from Beckton Dickinson. FH: speaker and travel grants from Correvio, other grants (clinical study reimbursement) from Basilea and Portola.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mohr, A., Simon, M., Joha, T. et al. Epidemiology of candidemia and impact of infectious disease consultation on survival and care. Infection 48, 275–284 (2020). https://doi.org/10.1007/s15010-020-01393-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-020-01393-9