Abstract
Purpose
There is currently a paucity of published literature focused on the treatment of infections caused by NDM-producing organisms.
Methods
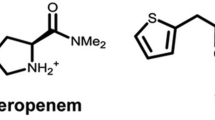
We describe a case of a bacteraemia caused by an extensively drug-resistant (XDR) New Delhi metallo-β-lactamase (NDM)-producing Serratia marcescens and review the treatment options for XDR NDM-producing Enterobacteriaceae.
Results
Infections caused by New Delhi beta-lactamase (NDM)-producing Enterobacteriaceae are becoming increasingly prevalent worldwide. The presence of the enzyme results in multidrug-resistant and extensively drug-resistant phenotypes which often pose a treatment challenge. Despite this challenge, case reports and series have demonstrated good clinical outcomes with numerous treatment options in comparison to infections due to KPC-producing Enterobacteriaceae.
Conclusions
Further good-quality research focused on the treatment of NDM-producing Enterobacteriaceae is warranted.

Similar content being viewed by others
References
Nordmann P, Poirel L, Walsh TR, Livermore DM. The emerging NDM carbapenemases. Trends Microbiol. 2011;19:588–95. doi:10.1016/j.tim.2011.09.005.
Arana DM, Saez D, García-Hierro P, Bautista V, Fernández-Romero S, Ángel de la Cal M, Alós JI, Oteo J. Concurrent interspecies and clonal dissemination of OXA-48 carbapenemase. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis. 2015;21:148.e1–4. doi:10.1016/j.cmi.2014.07.008.
Lin X, Hu Q, Zhang R, Hu Y, Xu X, Lv H. Emergence of Serratia marcescens isolates possessing carbapenem-hydrolysing β-lactamase KPC-2 from China. J Hosp Infect. 2016;94:65–7. doi:10.1016/j.jhin.2016.04.006.
Mataseje LF, Boyd DA, Delport J, Hoang L, Imperial M, Lefebvre B, Kuhn M, Van Caeseele P, Willey BM, Mulvey MR. Serratia marcescens harbouring SME-type class A carbapenemases in Canada and the presence of blaSME on a novel genomic island, SmarGI1-1. J Antimicrob Chemother. 2014;69:1825–9. doi:10.1093/jac/dku040.
Rubin JE, Peirano G, Peer AK, Govind CN, Pitout JDD. NDM-1-producing Enterobacteriaceae from South Africa: moving towards endemicity? Diagn Microbiol Infect Dis. 2014;79:378–80. doi:10.1016/j.diagmicrobio.2014.04.003.
Castanheira M, Deshpande LM, Mathai D, Bell JM, Jones RN, Mendes RE. Early dissemination of NDM-1- and OXA-181-producing Enterobacteriaceae in Indian hospitals: report from the SENTRY Antimicrobial Surveillance Program, 2006–2007. Antimicrob Agents Chemother. 2011;55:1274–8. doi:10.1128/AAC.01497-10.
Olaitan AO, Morand S, Rolain J-M. Mechanisms of polymyxin resistance: acquired and intrinsic resistance in bacteria. Front Microbiol. 2014;5:643. doi:10.3389/fmicb.2014.00643.
Magiorakos A-P, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, Harbarth S, Hindler JF, Kahlmeter G, Olsson-Liljequist B, Paterson DL, Rice LB, Stelling J, Struelens MJ, Vatopoulos A, Weber JT, Monnet DL. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis. 2012;18:268–81. doi:10.1111/j.1469-0691.2011.03570.x.
Clinical and Laboratory Standards Institute (2016) M100S, performance standards for antimicrobial susceptibility testing, 26th Edition.
Franklin C, Liolios L, Peleg AY. Phenotypic detection of carbapenem-susceptible metallo-beta-lactamase-producing gram-negative bacilli in the clinical laboratory. J Clin Microbiol. 2006;44:3139–44. doi:10.1128/JCM.00879-06.
Yong D, Toleman MA, Giske CG, Cho HS, Sundman K, Lee K, Walsh TR. Characterization of a new metallo-β-lactamase gene, blaNDM-1, and a novel erythromycin esterase gene carried on a unique genetic structure in Klebsiella pneumoniae sequence type 14 from India. Antimicrob Agents Chemother. 2009;53:5046–54. doi:10.1128/AAC.00774-09.
Poirel L, Dortet L, Bernabeu S, Nordmann P. Genetic features of blaNDM-1-positive Enterobacteriaceae. Antimicrob Agents Chemother. 2011;55:5403–7. doi:10.1128/AAC.00585-11.
Falagas ME, Lourida P, Poulikakos P, Rafailidis PI, Tansarli GS. Antibiotic treatment of infections due to carbapenem-resistant Enterobacteriaceae: systematic evaluation of the available evidence. Antimicrob Agents Chemother. 2014;58:654–63. doi:10.1128/AAC.01222-13.
Datta S, Roy S, Chatterjee S, Saha A, Sen B, Pal T, Som T, Basu S. A five-year experience of carbapenem resistance in Enterobacteriaceae causing neonatal septicaemia: predominance of NDM-1. PLoS One. 2014;9:e112101. doi:10.1371/journal.pone.0112101.
de Jager P, Chirwa T, Naidoo S, Perovic O, Thomas J. Nosocomial outbreak of New Delhi metallo-β-lactamase-1-producing Gram-negative bacteria in South Africa: a case-control study. PLoS One. 2015;10:e0123337. doi:10.1371/journal.pone.0123337.
Freire MP, Abdala E, Moura ML, de Paula FJ, Spadão F, Caiaffa-Filho HH, David-Neto E, Nahas WC, Pierrotti LC. Risk factors and outcome of infections with Klebsiella pneumoniae carbapenemase-producing K. pneumoniae in kidney transplant recipients. Infection. 2015;43:315–23. doi:10.1007/s15010-015-0743-4.
Fraenkel-Wandel Y, Raveh-Brawer D, Wiener-Well Y, Yinnon AM, Assous MV. Mortality due to blaKPC Klebsiella pneumoniae bacteraemia. J Antimicrob Chemother. 2016;71:1083–7. doi:10.1093/jac/dkv414.
Zmarlicka MT, Nailor MD, Nicolau DP. Impact of the New Delhi metallo-beta-lactamase on beta-lactam antibiotics. Infect Drug Resist. 2015;8:297–309. doi:10.2147/IDR.S39186.
Tamma PD, Goodman KE, Harris AD, Tekle T, Roberts A, Taiwo A, Simner PJ. Comparing the outcomes of patients with carbapenemase-producing and non-carbapenemase-producing carbapenem-resistant Enterobacteriaceae bacteremia. Clin Infect Dis Off Publ Infect Dis Soc Am. 2017;64:257–64. doi:10.1093/cid/ciw741.
Oteo J, Domingo-García D, Fernández-Romero S, Saez D, Guiu A, Cuevas O, Lopez-Brea M, Campos J. Abdominal abscess due to NDM-1-producing Klebsiella pneumoniae in Spain. J Med Microbiol. 2012;61:864–7. doi:10.1099/jmm.0.043190-0.
Peirano G, Ahmed-Bentley J, Woodford N, Pitout JD. New Delhi metallo-beta-lactamase from traveler returning to Canada. Emerg Infect Dis. 2011;17:242–4. doi:10.3201/eid1702.101313.
Zhang X, Li X, Wang M, Yue H, Li P, Liu Y, Cao W, Yao D, Liu L, Zhou X, Zheng R, Bo T. Outbreak of NDM-1-producing Klebsiella pneumoniae causing neonatal infection in a teaching hospital in mainland China. Antimicrob Agents Chemother. 2015;59:4349–51. doi:10.1128/AAC.03868-14.
Wiskirchen DE, Nordmann P, Crandon JL, Nicolau DP. Efficacy of humanized carbapenem exposures against New Delhi metallo-β-lactamase (NDM-1)-producing Enterobacteriaceae in a murine infection model. Antimicrob Agents Chemother. 2013;57:3936–40. doi:10.1128/AAC.00708-13.
Wiskirchen DE, Nordmann P, Crandon JL, Nicolau DP. In vivo efficacy of human simulated regimens of carbapenems and comparator agents against NDM-1-producing Enterobacteriaceae. Antimicrob Agents Chemother. 2014;58:1671–7. doi:10.1128/AAC.01946-13.
Gutiérrez-Gutiérrez B, Salamanca E, de Cueto M, Hsueh P-R, Viale P, Paño-Pardo JR, Venditti M, Tumbarello M, Daikos G, Cantón R, Doi Y, Tuon FF, Karaiskos I, Pérez-Nadales E, Schwaber MJ, Azap ÖK, Souli M, Roilides E, Pournaras S, Akova M, Pérez F, Bermejo J, Oliver A, Almela M, Lowman W, Almirante B, Bonomo RA, Carmeli Y, Paterson DL, Pascual A, Rodríguez-Baño J, REIPI, ESGBIS, INCREMENT Investigators. Effect of appropriate combination therapy on mortality of patients with bloodstream infections due to carbapenemase-producing Enterobacteriaceae (INCREMENT): a retrospective cohort study. Lancet Infect Dis. 2017;17:726–34. doi:10.1016/S1473-3099(17)30228-1.
Giamarellou H, Galani L, Baziaka F, Karaiskos I. Effectiveness of a double-carbapenem regimen for infections in humans due to carbapenemase-producing pandrug-resistant Klebsiella pneumoniae. Antimicrob Agents Chemother. 2013;57:2388–90. doi:10.1128/AAC.02399-12.
Oliva A, D’Abramo A, D’Agostino C, Iannetta M, Mascellino MT, Gallinelli C, Mastroianni CM, Vullo V. Synergistic activity and effectiveness of a double-carbapenem regimen in pandrug-resistant Klebsiella pneumoniae bloodstream infections. J Antimicrob Chemother. 2014;69:1718–20. doi:10.1093/jac/dku027.
Poirel L, Kieffer N, Nordmann P. In vitro evaluation of dual carbapenem combinations against carbapenemase-producing Enterobacteriaceae. J Antimicrob Chemother. 2016;71:156–61. doi:10.1093/jac/dkv294.
Tängdén T, Hickman RA, Forsberg P, Lagerbäck P, Giske CG, Cars O. Evaluation of double- and triple-antibiotic combinations for VIM- and NDM-producing Klebsiella pneumoniae by in vitro time-kill experiments. Antimicrob Agents Chemother. 2014;58:1757–62. doi:10.1128/AAC.00741-13.
Dortet L, Poirel L, Nordmann P. Worldwide dissemination of the NDM-type carbapenemases in Gram-negative bacteria. Biomed Res Int. 2014;2014:e249856. doi:10.1155/2014/249856.
Biedenbach D, Bouchillon S, Hackel M, Hoban D, Kazmierczak K, Hawser S, Badal R. Dissemination of NDM Metallo-β-lactamase genes among clinical isolates of Enterobacteriaceae collected during the SMART global surveillance study from 2008 to 2012. Antimicrob Agents Chemother. 2015;59:826–30. doi:10.1128/AAC.03938-14.
Berçot B, Poirel L, Nordmann P. Updated multiplex polymerase chain reaction for detection of 16S rRNA methylases: high prevalence among NDM-1 producers. Diagn Microbiol Infect Dis. 2011;71:442–5. doi:10.1016/j.diagmicrobio.2011.08.016.
Berçot B, Poirel L, Dortet L, Nordmann P. In vitro evaluation of antibiotic synergy for NDM-1-producing Enterobacteriaceae. J Antimicrob Chemother. 2011;66:2295–7. doi:10.1093/jac/dkr296.
Albur M, Noel A, Bowker K, MacGowan A. Bactericidal activity of multiple combinations of tigecycline and colistin against NDM-1-producing Enterobacteriaceae. Antimicrob Agents Chemother. 2012;56:3441–3. doi:10.1128/AAC.05682-11.
Albur MS, Noel A, Bowker K, MacGowan A. The combination of colistin and fosfomycin is synergistic against NDM-1-producing Enterobacteriaceae in in vitro pharmacokinetic/pharmacodynamic model experiments. Int J Antimicrob Agents. 2015;46:560–7. doi:10.1016/j.ijantimicag.2015.07.019.
Neuner EA, Sekeres J, Hall GS, van Duin D. Experience with fosfomycin for treatment of urinary tract infections due to multidrug-resistant organisms. Antimicrob Agents Chemother. 2012;56:5744–8. doi:10.1128/AAC.00402-12.
Lavigne J-P, Cuzon G, Combescure C, Bourg G, Sotto A, Nordmann P. Virulence of Klebsiella pneumoniae Isolates Harboring blaKPC-2 Carbapenemase Gene in a Caenorhabditis elegans Model. PLoS One. 2013;8:e67847. doi:10.1371/journal.pone.0067847.
McLaughlin MM, Advincula MR, Malczynski M, Barajas G, Qi C, Scheetz MH. Quantifying the clinical virulence of Klebsiella pneumoniae producing carbapenemase Klebsiella pneumoniae with a Galleria mellonellamodel and a pilot study to translate to patient outcomes. BMC Infect Dis. 2014;. doi:10.1186/1471-2334-14-31.
Göttig S, Riedel-Christ S, Saleh A, Kempf VAJ, Hamprecht A. Impact of blaNDM-1 on fitness and pathogenicity of Escherichia coli and Klebsiella pneumoniae. Int J Antimicrob Agents. 2016;47:430–5. doi:10.1016/j.ijantimicag.2016.02.019.
Mouton JW, Brown DFJ, Apfalter P, Cantón R, Giske CG, Ivanova M, MacGowan AP, Rodloff A, Soussy C-J, Steinbakk M, Kahlmeter G. The role of pharmacokinetics/pharmacodynamics in setting clinical MIC breakpoints: the EUCAST approach. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis. 2012;18:E37–45. doi:10.1111/j.1469-0691.2011.03752.x.
Sime FB, Roberts MS, Roberts JA. Optimization of dosing regimens and dosing in special populations. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis. 2015;21:886–93. doi:10.1016/j.cmi.2015.05.002.
Lowman W, Schleicher G. Antimicrobial treatment and outcomes of critically ill patients with OXA-48like carbapenemase-producing Enterobacteriaceae infections. Diagn Microbiol Infect Dis. 2015;81:138–40. doi:10.1016/j.diagmicrobio.2014.09.023.
Tzouvelekis LS, Markogiannakis A, Piperaki E, Souli M, Daikos GL. Treating infections caused by carbapenemase-producing Enterobacteriaceae. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis. 2014;20:862–72. doi:10.1111/1469-0691.12697.
Lodise TP, Lomaestro BM, Drusano GL, Society of Infectious Diseases Pharmacists. Application of antimicrobial pharmacodynamic concepts into clinical practice: focus on beta-lactam antibiotics: insights from the Society of Infectious Diseases Pharmacists. Pharmacotherapy. 2006;26:1320–32. doi:10.1592/phco.26.9.1320.
Roberts JA, Abdul-Aziz MH, Lipman J, Mouton JW, Vinks AA, Felton TW, Hope WW, Farkas A, Neely MN, Schentag JJ, Drusano G, Frey OR, Theuretzbacher U, Kuti JL, International Society of Anti-Infective Pharmacology and the Pharmacokinetics and Pharmacodynamics Study Group of the European Society of Clinical Microbiology and Infectious Diseases. Individualised antibiotic dosing for patients who are critically ill: challenges and potential solutions. Lancet Infect Dis. 2014;14:498–509. doi:10.1016/S1473-3099(14)70036-2.
Barbhaiya RH, Forgue ST, Gleason CR, Knupp CA, Pittman KA, Weidler DJ, Movahhed H, Tenney J, Martin RR. Pharmacokinetics of cefepime after single and multiple intravenous administrations in healthy subjects. Antimicrob Agents Chemother. 1992;36:552–7.
MacGowan AP. Tigecycline pharmacokinetic/pharmacodynamic update. J Antimicrob Chemother. 2008;62(Suppl 1):i11–6. doi:10.1093/jac/dkn242.
Westphal JF, Brogard JM, Caro-Sampara F, Adloff M, Blicklé JF, Monteil H, Jehl F. Assessment of biliary excretion of piperacillin-tazobactam in humans. Antimicrob Agents Chemother. 1997;41:1636–40.
Bassetti M, Righi E. New antibiotics and antimicrobial combination therapy for the treatment of gram-negative bacterial infections. Curr Opin Crit Care. 2015;21:402–11. doi:10.1097/MCC.0000000000000235.
Thaden JT, Pogue JM, Kaye KS. Role of newer and re-emerging older agents in the treatment of infections caused by carbapenem-resistant Enterobacteriaceae. Virulence. 2016;8:1–14. doi:10.1080/21505594.2016.1207834.
Biedenbach DJ, Kazmierczak K, Bouchillon SK, Sahm DF, Bradford PA. In vitro activity of aztreonam-avibactam against a global collection of Gram-negative pathogens from 2012 and 2013. Antimicrob Agents Chemother. 2015;59:4239–48. doi:10.1128/AAC.00206-15.
http://investors.achaogen.com/releasedetail.cfm?releaseid=987442. Accessed 18 Jan 2017.
Escobar Pérez JA, Olarte Escobar NM, Castro-Cardozo B, Valderrama Márquez IA, Garzón Aguilar MI, Martinez de la Barrera L, Barrero Barreto ER, Marquez-Ortiz RA, Moncada Guayazán MV, Vanegas Gómez N. Outbreak of NDM-1-producing Klebsiella pneumoniae in a neonatal unit in Colombia. Antimicrob Agents Chemother. 2013;57:1957–60. doi:10.1128/AAC.01447-12.
Seija V, Medina Presentado JC, Bado I, Papa Ezdra R, Batista N, Gutierrez C, Guirado M, Vidal M, Nin M, Vignoli R. Sepsis caused by New Delhi metallo-β-lactamase (blaNDM-1) and qnrD-producing Morganella morganii, treated successfully with fosfomycin and meropenem: case report and literature review. Int J Infect Dis IJID Off Publ Int Soc Infect Dis. 2015;30:20–6. doi:10.1016/j.ijid.2014.09.010.
Torres-González P, Bobadilla-del Valle M, Tovar-Calderón E, Leal-Vega F, Hernández-Cruz A, Martínez-Gamboa A, Niembro-Ortega MD, Sifuentes-Osornio J, Ponce-de-León A. Outbreak Caused by Enterobacteriaceae harboring NDM-1 metallo-β-lactamase carried in an IncFII plasmid in a tertiary care hospital in Mexico city. Antimicrob Agents Chemother. 2015;59:7080–3. doi:10.1128/AAC.00055-15.
Chien JMF, Koh TH, Chan KS, Chuah THC, Tan TT. Successful treatment of NDM-1 Klebsiella pneumoniae bacteraemia in a neutropenic patient. Scand J Infect Dis. 2012;44:312–4. doi:10.3109/00365548.2011.633549.
Pannaraj PS, Bard JD, Cerini C, Weissman SJ. Pediatric Carbapenem-resistant Enterobacteriaceae in Los Angeles, California, a high-prevalence region in the United States. Pediatr Infect Dis J. 2015;34:11–6. doi:10.1097/INF.0000000000000471.
Wilkowski P, Ciszek M, Dobrzaniecka K, Sańko-Resmer J, Łabuś A, Grygiel K, Grochowiecki T, Młynarczyk G, Pączek L. Successful treatment of urinary tract infection in kidney transplant recipients caused by multiresistant Klebsiella pneumoniae producing New Delhi Metallo-beta-lactamase (NDM-1) with strains genotyping. Transplant Proc. 2016;48:1576–9. doi:10.1016/j.transproceed.2016.01.060.
Tran HH, Ehsani S, Shibayama K, Matsui M, Suzuki S, Nguyen MB, Tran DN, Tran VP, Tran DL, Nguyen HT, Dang DA, Trinh HS, Nguyen TH, Wertheim HFL. Common isolation of New Delhi metallo-beta-lactamase 1-producing Enterobacteriaceae in a large surgical hospital in Vietnam. Eur J Clin Microbiol Infect Dis. 2015;34:1247–54. doi:10.1007/s10096-015-2345-6.
Barrios H, Silva-Sanchez J, Reyna-Flores F, Sanchez-Perez A, Sanchez-Francia D, Aguirre-Torres JA, Sánchez-Rogel J, Garza-Ramos U. Detection of a NDM-1-producing Klebsiella pneumoniae (ST22) clinical isolate at a pediatric hospital in Mexico. Pediatr Infect Dis J. 2014;33:335. doi:10.1097/INF.0000000000000173.
Poirel L, Ros A, Carricajo A, Berthelot P, Pozzetto B, Bernabeu S, Nordmann P. Extremely drug-resistant Citrobacter freundii isolate producing NDM-1 and other carbapenemases identified in a patient returning from India. Antimicrob Agents Chemother. 2011;55:447–8. doi:10.1128/AAC.01305-10.
Rogers BA, Sidjabat HE, Silvey A, Anderson TL, Perera S, Li J, Paterson DL. Treatment options for New Delhi metallo-beta-lactamase-harboring enterobacteriaceae. Microb Drug Resist Larchmt N. 2013;19:100–3. doi:10.1089/mdr.2012.0063.
Chan HLE, Poon LM, Chan SG, Teo JWP. The perils of medical tourism: NDM-1-positive Escherichia coli causing febrile neutropenia in a medical tourist. Singap Med J. 2011;52:299–302.
Stone NRH, Woodford N, Livermore DM, Howard J, Pike R, Mushtaq S, Perry C, Hopkins S (2011) Breakthrough bacteraemia due to tigecycline-resistant Escherichia coli with New Delhi metallo-β-lactamase (NDM)-1 successfully treated with colistin in a patient with calciphylaxis. J Antimicrob Chemother dkr337. doi:10.1093/jac/dkr337.
Carvalho-Assef APD, Pereira PS, Albano RM, Berião GC, Chagas TPG, Timm LN, Da Silva RCF, Falci DR, Asensi MD. Isolation of NDM-producing Providencia rettgeri in Brazil. J Antimicrob Chemother. 2013;68:2956–7. doi:10.1093/jac/dkt298.
Lai C-C, Lin T-L, Tseng S-P, Huang Y-T, Wang J-T, Chang S-C, Teng L-J, Wang J-T, Hsueh P-R. Pelvic abscess caused by New Delhi metallo-β-lactamase-1-producing Klebsiella oxytoca in Taiwan in a patient who underwent renal transplantation in China. Diagn Microbiol Infect Dis. 2011;71:474–5. doi:10.1016/j.diagmicrobio.2011.09.004.
Hoang TH, Wertheim H, Minh NB, Duong TN, Anh DD, Phuong TTL, Son TH, Izumiya H, Ohnishi M, Shibayama K, Hien NT. Carbapenem-resistant Escherichia coli and Klebsiella pneumoniae strains containing New Delhi metallo-beta-lactamase isolated from two patients in Vietnam. J Clin Microbiol. 2013;51:373–4. doi:10.1128/JCM.02322-12.
De Pascale G, Martucci G, Montini L, Panarello G, Cutuli SL, Di Carlo D, Di Gravio V, Di Stefano R, Capitanio G, Vallecoccia MS, Polidori P, Spanu T, Arcadipane A, Antonelli M. Double carbapenem as a rescue strategy for the treatment of severe carbapenemase-producing Klebsiella pneumoniae infections: a two-center, matched case-control study. Crit Care. 2017;21:173. doi:10.1186/s13054-017-1769-z.
Doi Y, Paterson DL. Carbapenemase-producing enterobacteriaceae. Semin Respir Crit Care Med. 2015;36:74–4.
Kumarasamy KK, Toleman MA, Walsh TR, Bagaria J, Butt F, Balakrishnan R, Chaudhary U, Doumith M, Giske CG, Irfan S, Krishnan P, Kumar AV, Maharjan S, Mushtaq S, Noorie T, Paterson DL, Pearson A, Perry C, Pike R, Rao B, Ray U, Sarma JB, Sharma M, Sheridan E, Thirunarayan MA, Turton J, Upadhyay S, Warner M, Welfare W, Livermore DM, Woodford N. Emergence of a new antibiotic resistance mechanism in India, Pakistan, and the UK: a molecular, biological, and epidemiological study. Lancet Infect Dis. 2010;10:597–02. doi:10.1016/S1473-3099(10)70143-2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was sought for this paper.
Conflict of interest
All authors declare no conflicts of interest.
Informed consent
Informed consent has been obtained from the concerned case.
Rights and permissions
About this article
Cite this article
Chibabhai, V., Nana, T., Bosman, N. et al. Were all carbapenemases created equal? Treatment of NDM-producing extensively drug-resistant Enterobacteriaceae: a case report and literature review. Infection 46, 1–13 (2018). https://doi.org/10.1007/s15010-017-1070-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-017-1070-8