Abstract
Purpose
Tuberculous pleural effusion (TPE) and parapneumonic effusion (PPE) are usually distinguished by cellular predominance and pleural fluid adenosine deaminase (ADA) levels. However, both diseases may occasionally show similar neutrophilic predominance and high ADA levels. In such cases, the differential diagnosis between TPE and PPE is challenging and has been rarely investigated.
Methods
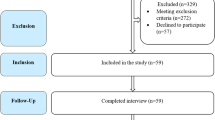
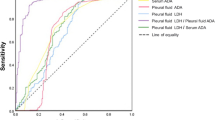
A retrospective study was conducted on TPE and PPE patients with neutrophilic exudate and pleural fluid ADA levels ≥40 U/L. Individual and combined parameters of routine blood and pleural fluid tests were compared between the two groups, and receiver operating characteristic (ROC) curves were constructed for identifying TPE.
Results
Thirty-six TPE and 41 PPE patients were included. White blood cell counts, serum C-reactive protein (S-CRP), and pleural fluid pH, lactate dehydrogenase, and ADA levels showed significant difference between the two groups (p < 0.001). Among multiple parameters, pleural fluid ADA/S-CRP ratio, which best reflected different local and systemic characteristics between TPE and PPE, provided the highest diagnostic accuracy with an area under the ROC curve of 0.93. At a cutoff value of 5.62, ADA/S-CRP ratio had a sensitivity of 89 %, specificity of 88 %, positive likelihood ratio of 7.29, and negative likelihood ratio of 0.13 for identifying TPE. Additionally, more than half of TPE patients had a ratio above 15.82, while none of PPE patients showed such findings.
Conclusions
Pleural fluid ADA/S-CRP ratio, as a simple method using routine laboratory tests, may be helpful in discriminating between TPE and PPE patients with neutrophilic predominance and ADA ≥40 U/L.


Similar content being viewed by others
References
Porcel JM, Vives M. Etiology and pleural fluid characteristics of large and massive effusions. Chest. 2003;124:978–83.
Maji A, Maikap MK, Jash D, Saha K, Kundu A, Saha D, et al. Role of common investigations in aetiological evaluation of exudative pleural effusions. J Clin Diagn Res. 2013;7:2223–6.
Lin MT, Wang JY, Yu CJ, Lee LN, Yang PC. Mycobacterium tuberculosis and polymorphonuclear pleural effusion: incidence and clinical pointers. Respir Med. 2009;103:820–6.
Colice GL, Curtis A, Deslauriers J, Heffner J, Light R, Littenberg B, et al. Medical and surgical treatment of parapneumonic effusions: an evidence-based guideline. Chest. 2000;118:1158–71.
Liang QL, Shi HZ, Wang K, Qin SM, Qin XJ. Diagnostic accuracy of adenosine deaminase in tuberculous pleurisy: a meta-analysis. Respir Med. 2008;102:744–54.
Krenke R, Korczynski P. Use of pleural fluid levels of adenosine deaminase and interferon gamma in the diagnosis of tuberculous pleuritis. Curr Opin Pulm Med. 2010;16:367–75.
Ruan SY, Chuang YC, Wang JY, Lin JW, Chien JY, Huang CT, et al. Revisiting tuberculous pleurisy: pleural fluid characteristics and diagnostic yield of mycobacterial culture in an endemic area. Thorax. 2012;67:822–7.
Porcel JM, Vives M, Esquerda A, Ruiz A. Usefulness of the British Thoracic Society and the American College of Chest Physicians guidelines in predicting pleural drainage of non-purulent parapneumonic effusions. Respir Med. 2006;100:933–7.
Porcel JM, Esquerda A, Bielsa S. Diagnostic performance of adenosine deaminase activity in pleural fluid: a single-center experience with over 2100 consecutive patients. Eur J Intern Med. 2010;21:419–23.
Trajman A, da Silva Santos Kleiz de Oliveira EF, Bastos ML, Belo Neto E, Silva EM, da Silva Lourenco MC, et al. Accuracy of polymerase chain reaction for the diagnosis of pleural tuberculosis. Respir Med 2014;108:918–23.
Kiropoulos TS, Kostikas K, Oikonomidi S, Tsilioni I, Nikoulis D, Germenis A, et al. Acute phase markers for the differentiation of infectious and malignant pleural effusions. Respir Med. 2007;101:910–8.
Lee J, Lee SY, Lim JK, Yoo SS, Cha SI, Park JY, et al. Radiologic and laboratory differences in patients with tuberculous and parapneumonic pleural effusions showing non-lymphocytic predominance and high adenosine deaminase levels. Infection. 2015;43:65–71.
Lee J, Lim JK, Lee SY, Yoo SS, Cha SI, Park JY, et al. Neutrophilic loculated tuberculous pleural effusion: incidence, characteristics and differentiation from complicated parapneumonic effusion. Am J Med Sci. 2016;351:153–9.
Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med. 1999;340:448–54.
Bielsa S, Valencia H, Ruiz-Gonzalez A, Esquerda A, Porcel JM. Serum C-reactive protein as an adjunct for identifying complicated parapneumonic effusions. Lung. 2014;192:577–81.
Daniil ZD, Zintzaras E, Kiropoulos T, Papaioannou AI, Koutsokera A, Kastanis A, et al. Discrimination of exudative pleural effusions based on multiple biological parameters. Eur Respir J. 2007;30:957–64.
Porcel JM, Vives M, Cao G, Bielsa S, Ruiz-Gonzalez A, Martinez-Iribarren A, et al. Biomarkers of infection for the differential diagnosis of pleural effusions. Eur Respir J. 2009;34:1383–9.
World Health Organization. Global tuberculosis report 2015. http://www.who.int/tb/data.
Bielsa S, Palma R, Pardina M, Esquerda A, Light RW, Porcel JM. Comparison of polymorphonuclear- and lymphocyte-rich tuberculous pleural effusions. Int J Tuberc Lung Dis. 2013;17:85–9.
Jeon D. Tuberculous pleurisy: an update. Tuberc Respir Dis (Seoul). 2014;76:153–9.
Morley JJ, Kushner I. Serum C-reactive protein levels in disease. Ann N Y Acad Sci. 1982;389:406–18.
Porcel JM. Pleural fluid tests to identify complicated parapneumonic effusions. Curr Opin Pulm Med. 2010;16:357–61.
Porcel JM. Tuberculous pleural effusion. Lung. 2009;187:263–70.
Acknowledgments
This research was supported by Kyungpook National University Research Fund, 2016 and by Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Science, ICT & Future Planning (2015R1C1A2A01052502).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lee, J., Yoo, S.S., Lee, S.Y. et al. Pleural fluid adenosine deaminase/serum C-reactive protein ratio for the differentiation of tuberculous and parapneumonic effusions with neutrophilic predominance and high adenosine deaminase levels. Infection 45, 59–65 (2017). https://doi.org/10.1007/s15010-016-0928-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-016-0928-5