Abstract
Background:
The aim of this paper was to enlarge the available knowledge on clinical and etiological aspects of patients affected by spondylodiscitis.
Patients and Methods:
All patients with spondylodiscitis admitted between January 2001 and December 2007 at the 1,300-bed University Hospital "Policlinico Umberto I" of Rome, Italy, were followed. Demographic characteristics, underlying diseases, invasive procedures, imaging studies, isolated microorganisms, treatment, complications, and outcome were recorded.
Results:
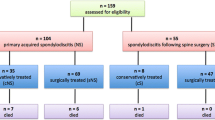
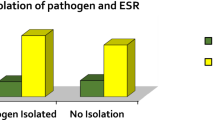
Eighty-one patients of mean age 57.7 ± 14.7 years with lumbosacral (72.8%), thoracic (14.8%), and cervical tract (12.3%) site of infection were included, of which 38 developed communityacquired (CA) spondylodiscitis and 43 developed hospital-acquired (HA) spondylodiscitis. Underlying disease was present in 49.4% of patients. HA spondylodiscitis was diagnosed earlier (46.8 ± 49.7 days) than CA spondylodiscitis (65.0 ± 55.4 days) (P < 0.05). The most frequently isolated microorganisms were Staphylococcus aureus (28 strains, 43.1%), coagulase-negative staphylococci (CNS) (eight strains, 12.3%), Pseudomonas aeruginosa (eight strains, 12.3%), and three methicillin-resistant S. aureus (MRSA) strains were isolated in CA spondylodiscitis. Fungi and yeasts, isolated in six patients, represented 9.2% of all strains but 17.6% when considering only HA spondylodiscitis. Over 85% of patients were managed by conservative treatment alone, and the treatment time depended on clinical and laboratory evidence. Poor outcome was recorded in 12 (14.8%) patients, and was associated with neurological deficit symptoms (relative risk [RR] 2.87; 95% confidence interval [CI] 1.02–8.07; P < 0.05) and the time between diagnosis and the onset of symptoms ≥ 60 days (RR 2.65; 95% CI 0.92–7.59; P < 0.05).
Conclusions:
Infectious spondylodiscitis affects most frequently the elderly population, who are more exposed to healthcare contacts. Consequently, the infection etiology includes a growing proportion of multi-resistant bacteria and fungi.
Similar content being viewed by others
References
Acosta FL Jr, Chin CT, Quiñones H, Ames CP, Weinstein PR, Chou D: Diagnosis and management of adult pyogenic osteomyelitis of the cervical spine. Neurosurg Focus 2004; 17: E2.
Butler JS, Shelly MJ, Timlin M, Powderly WG, O’Byrne JM: Nontuberculous pyogenic spinal infection in adults: a 12-year experience from a tertiary referral center. Spine 2006; 31: 2695–2700.
Acosta FL Jr, Galvez LF, Aryan HE, Ames CP: Recent advances: infections of the spine. Curr Infect Dis Rep 2006; 8: 390–393.
Cottle L, Riordan T: Infectious spondylodiscitis. J Infect 2008; 56: 401–412.
O’Daly BJ, Morris SF, O’Rourke SK: Long-term functional outcome in pyogenic spinal infection. Spine 2008; 33: E246–E253.
McHenry MC, Easley KA, Locker GA: Vertebral osteomyelitis: long-term outcome for 253 patients from 7 Cleveland-area hospitals. Clin Infect Dis 2002; 34: 1342–1350.
Solis Garcia del Pozo J, Vives Soto M, Solera J: Vertebral osteomyelitis: long-term disability assessment and prognostic factors. J Infect 2007; 54: 129–134.
Bettini N, Girardo M, Dema E, Cervellati S: Evaluation of conservative treatment of non specific spondylodiscitis. Eur Spine J 2009; 18: 143–150.
Carragee EJ: Pyogenic vertebral osteomyelitis. J Bone Joint Surg Am 1997; 79: 874–880.
Hadjipavlou AG, Mader JT, Necessary JT, Muffoletto AJ: Hematogenous pyogenic spinal infections and their surgical management. Spine 2000; 25: 1668–1679.
Karadimas EJ, Bunger C, Lindblad BE, Hansen ES, Høy K, Helmig P, Kannerup AS, Niedermann B: Spondylodiscitis. A retrospective study of 163 patients. Acta Orthop 2008; 79: 650–659.
Kowalski TJ, Berbari EF, Huddleston PM, Steckelberg JM, Osmon DR: Do follow-up imaging examinations provide useful prognostic information in patients with spine infection?. Clin Infect Dis 2006; 43: 172–179.
Luzzati R, Giacomazzi D, Danzi MC, Tacconi L, Concia E, Vento S: Diagnosis, management and outcome of clinically-suspected spinal infection. J Infect 2009; 58: 259–265.
Roblot F, Besnier JM, Juhel L, Vidal C, Ragot S, Bastides F, Le Moal G, Godet C, Mulleman D, Azaïs I, Becq-Giraudon B, Choutet P: Optimal duration of antibiotic therapy in vertebral osteomyelitis. Semin Arthritis Rheum 2007; 36: 269–277.
Kowalski TJ, Layton KF, Berbari EF, Steckelberg JM, Huddleston PM, Wald JT, Osmon DR: Follow-up MR imaging in patients with pyogenic spine infections: lack of correlation with clinical features. Am J Neuroradiol 2007; 28: 693–699.
Govender S: Spinal infections. J Bone Joint Surg Br 2005; 87: 1454–1458.
Jiménez-Mejías ME, de Dios Colmenero J, Sánchez-Lora FJ, Palomino-Nicás J, Reguera JM, García de la Heras J, García-Ordoñez MA, Pachón J: Postoperative spondylodiskitis: etiology, clinical findings, prognosis, and comparison with nonoperative pyogenic spondylodiskitis. Clin Infect Dis 1999; 29: 339–345.
Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, Lamm W, Clark C, MacFarquhar J, Walton AL, Reller LB, Sexton DJ: Healthcare-associated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections. Ann Intern Med 2002; 137: 791–797.
Venditti M, Falcone M, Corrao S, Licata G, Serra P: Outcomes of patients hospitalized with community-acquired, health careassociated and hospital-acquired pneumonia. Ann Intern Med 2009; 150: 19–26.
Lam KS, Webb JK: Discitis. Hosp Med 2004; 65: 280–286.
Le Moal G, Roblot F, Paccalin M, Sosner P, Burucoa C, Roblot P, Becq-Giraudon B: Clinical and laboratory characteristics of infective endocarditis when associated with spondylodiscitis. Eur J Clin Microbiol Infect Dis 2002; 21: 671–675.
Pigrau C, Almirante B, Flores X, Falco V, Rodríguez D, Gasser I, Villanueva C, Pahissa A: Spontaneous pyogenic vertebral osteomyelitis and endocarditis: incidence, risk factors, and outcome. Am J Med 2005; 118: 1287.e17–1287.e24.
Chia SL, Tan BH, Tan CT, Tan SB: Candida spondylodiscitis and epidural abscess: management with shorter courses of antifungal therapy in combination with surgical debridement. J Infect 2005; 51: 17–23.
Garcia-Vidal C, Cabellos C, Ayats J, Font F, Ferran E, Fernandez-Viladrich P: Fungal postoperative spondylodiscitis due to Scedosporium prolificans. Spine J 2009; 9: e1–e7.
Johnson MD, Perfect JR: Fungal infections of the bones and joints. Curr Infect Dis Rep 2001; 3: 450–460.
Hendrickx L, Van Wijngaerden E, Samson I, Peetermans WE: Candidal vertebral osteomyelitis: report of 6 patients, and a review. Clin Infect Dis 2001; 32: 527–533.
Parry MF, Grant B, Yukna M, Adler-Klein D, McLeod GX, Taddonio R, Rosenstein C: Candida osteomyelitis and diskitis after spinal surgery: an outbreak that implicates artificial nail use. Clin Infect Dis 2001; 32: 352–357.
Grados F, Lescure FX, Senneville E, Flipo RM, Schmit JL, Fardellone P: Suggestions for managing pyogenic (non-tuberculous) discitis in adults. Joint Bone Spine 2007; 74: 133–139.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
D’Agostino, C., Scorzolini, L., Massetti, A.P. et al. A Seven-Year Prospective Study on Spondylodiscitis: Epidemiological and Microbiological Features. Infection 38, 102–107 (2010). https://doi.org/10.1007/s15010-009-9340-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-009-9340-8