Abstract
Background:
Beta-tricalcium phosphate (β-TCP) has been employed successfully as a synthetic graft material in maxillary sinus floor augmentation (MSFA) for placing dental implants. However, the lack of osteogenic and osteoinductive properties of this substitute invariably results in bone regeneration of low quality and quantity. The purpose of this study was to determine whether loading dentin matrix protein-1 (DMP1) gene-modified bone marrow mesenchymal stem cells (BMSCs) onto β-TCP promoted bone regeneration and osteointegration of dental implants in MSFA of dogs.
Methods:
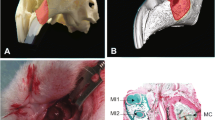
BMSCs were transduced with a lentiviral vector overexpressing the DMP1 gene (Lenti-DMP1) and with a lentiviral vector overexpressing enhanced green fluorescent protein (Lenti-EGFP) in vitro and were loaded into β-TCP scaffolds for autologous sinus grafting. Beagles received bilateral MSFA with four biomaterials (① Lenti-DMP1-transduced BMSCs/β-TCP, ② Lenti-EGFP-transduced BMSCs/β-TCP, ③ BMSCs/β-TCP, ④ β-TCP) and simultaneous implant placement at each sinus. Twelve weeks post operation, the maxillae were explanted, and every sinus was evaluated by radiographic observation, micro-CT and histological analysis. The osteogenic outcomes of bone regeneration and osseointegration were compared between the four groups.
Results:
The sinuses grafted with Lenti-DMP1-transduced BMSCs/β-TCP constructs presented a significantly higher increase in compact radiopaque area, higher local bone mineral densities, greater bone-implant contact and greater bone density when compared to other three groups.
Conclusion:
These results demonstrated that combinations of β-TCP and DMP1 gene-modified BMSCs could be used to construct tissue-engineered bone to enhance mineralization of the regenerated bone and osseointegration of dental implants in MSFA.









Similar content being viewed by others
References
Sverzut AT, Rodrigues DC, Lauria A, Armando RS, de Oliveira PT, Moreira RW. Clinical, radiographic, and histological analyses of calcium phosphate cement as filling material in maxillary sinus lift surgery. Clin Oral Implants Res. 2015;26:633–8.
Aludden HC, Mordenfeld A, Hallman M, Dahlin C, Jensen T. Lateral ridge augmentation with Bio-Oss alone or Bio-Oss mixed with particulate autogenous bone graft: a systematic review. Int J Oral Maxillofac Surg. 2017;46:1030–8.
Starch-Jensen T, Aludden H, Hallman M, Dahlin C, Christensen AE, Mordenfeld A. A systematic review and meta-analysis of long-term studies (five or more years) assessing maxillary sinus floor augmentation. Int J Oral Maxillofac Surg. 2018;47:103–16.
Alayan J, Ivanovski S. A prospective controlled trial comparing xenograft/autogenous bone and collagen-stabilized xenograft for maxillary sinus augmentation-complications, patient-reported outcomes and volumetric analysis. Clin Oral Implants Res. 2018;29:248–62.
Niño-Sandoval TC, Vasconcelos BC, Moraes SLD, Lemos CAA, Pellizzer EP. Efficacy of stem cells in maxillary sinus floor augmentation: systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2019;48:1355–66.
Kurkcu M, Benlidayi ME, Cam B, Sertdemir Y. Anorganic bovine-derived hydroxyapatite vs β-tricalcium phosphate in sinus augmentation: a comparative histomorphometric study. J Oral Implant. 2012;38:519–26.
Mangano C, Perrotti V, Shibli JA, Mangano F, Ricci L, Piattelli A, et al. Maxillary sinus grafting with biphasic calcium phosphate ceramics: clinical and histologic evaluation in man. Int J Oral Maxillofac Implants. 2013;28:51–6.
Jensen OT, Kuhlke KL, Leopardi A, Adams MW, Ringeman JL. BMP-2/ACS/Allograft for combined maxillary alveolar split/sinus floor grafting with and without simultaneous dental implant placement: report of 21 implants placed into 7 alveolar split sites followed for up to 3 years. Int J Oral Maxillofac Implants. 2014;29:e81–94.
Nizam N, Eren G, Akcalı A, Donos N. Maxillary sinus augmentation with leukocyte and platelet-rich fibrin and deproteinized bovine bone mineral: a split-mouth histological and histomorphometric study. Clin Oral Implants Res. 2018;29:67–75.
Stavropoulos A, Becker J, Capsius B, Açil Y, Wagner W, Terheyden H. Histological evaluation of maxillary sinus floor augmentation with recombinant human growth and differentiation factor-5-coated β-tricalcium phosphate: results of a multicenter randomized clinical trial. J Clin Periodontol. 2011;38:966–74.
Gutwald R, Haberstroh J, Stricker A, Rüther E, Otto F, Xavier SP, et al. Influence of rhBMP-2 on bone formation and osseointegration in different implant systems after sinus-floor elevation. An in vivo study on sheep. J Craniomaxillofac Surg. 2010;38:571–9.
Liu X, Li Q, Wang F, Wang Z. Maxillary sinus floor augmentation and dental implant placement using dentin matrix protein-1 gene-modified bone marrow stromal cells mixed with deproteinized boving bone: a comparative study in beagles. Arch Oral Biol. 2016;64:102–8.
Xia L, Xu Y, Chang Q, Sun X, Zeng D, Zhang W, et al. Maxillary sinus floor elevation using BMP-2 and nell-1 gene-modified bone marrow stromal cells and TCP in rabbits. Calcif Tissue Int. 2011;89:53–64.
Lu Y, Ye L, Yu S, Zhang S, Xie Y, McKee MD, et al. Rescue of odontogenesis in Dmp1-deficient mice by targeted re-expression of DMP1 reveals roles for DMP1 in early odontogenesis and dentin apposition in vivo. Dev Biol. 2007;303:191–201.
Narayanan K, Srinivas R, Ramachandran A, Hao J, Quinn B, George A. Differentiation of embryonic mesenchymal cells to odontoblast-like cells by overexpression of dentin matrix protein 1. Proc Natl Acad Sci U S A. 2001;98:4516–21.
Sun Y, Jiang Y, Liu Q, Gao T, Feng JQ, Dechow P, et al. Biomimetic engineering of nanofibrous gelatin scaffolds with noncollagenous proteins for enhanced bone regeneration. Tissue Eng Part A. 2013;19:1754–63.
Skoglund A, Hising P, Young C. A clinical and histologic examination in humans of the osseous response to implanted natural bone mineral. Int J Oral Maxillofac Implants. 1997;12:194–9.
Yildirim M, Spiekermann H, Handt S, Edelhoff D. Maxillary sinus augmentation with the xenograft Bio-Oss and autogenous intraoral bone for qualitative improvement of the implant site: a histologic and histomorphometric clinical study in humans. Int J Oral Maxillofac Implants. 2001;16:23–33.
Zarb G, Lekholm U, Albrektsson T. In memoriam: Per-Ingvar Brånemark. Int J Prosthodont. 2015;28:8.
Shayesteh YS, Khojasteh A, Soleimani M, Alikhasi M, Khoshzaban A, Ahmadbeigi N. Sinus augmentation using human mesenchymal stem cells loaded into a β-tricalcium phosphate/hydroxyapatite scaffold. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:203–9.
Feng JQ, Ward LM, Liu S, Lu Y, Xie Y, Yuan B, et al. Loss of DMP1 causes rickets and osteomalacia and identifies a role for osteocytes in mineral metabolism. Nat Genet. 2006;38:1310–5.
Ye L, MacDougall M, Zhang S, Xie Y, Zhang J, Li Z, et al. Deletion of dentin matrix protein-1 leads to a partial failure of maturation of predentin into dentin, hypomineralization, and expanded cavities of pulp and root canal during postnatal tooth development. J Biol Chem. 2004;279:19141–8.
Ye L, Mishina Y, Chen D, Huang H, Dallas SL, Dallas MR, et al. Dmp1-deficient mice display severe defects in cartilage formation responsible for a chondrodysplasia-like phenotype. J Biol Chem. 2005;280:6197–203.
Gajjeraman S, Narayanan K, Hao J, Qin C, George A. Matrix macromolecules in hard tissues control the nucleation and hierarchical assembly of hydroxyapatite. J Biol Chem. 2007;282:1193–204.
Maciejewska I, Cowan C, Svoboda K, Butler WT, D’Souza R, Qin C. The NH2-terminal and COOH-terminal fragments of dentin matrix protein 1 (DMP1) localize differently in the compartments of dentin and growth plate of bone. J Histochem Cytochem. 2009;57:155–66.
Tartaix PH, Doulaverakis M, George A, Fisher LW, Butler WT, Qin C, et al. In vitro effects of dentin matrix protein-1 on hydroxyapatite formation provide insights into in vivo functions. J Biol Chem. 2004;279:18115–20.
Delpinoi A, Piselli P, Vismara D, Vendetti S, Colizzi V. Cell surface localization of the 78 kD glucose regulated protein (GRP 78) induced by thapsigargin. Mol Membr Biol. 1998;15:21–6.
Eapen A, Sundivakkam P, Song Y, Ravindran S, Ramachandran A, Tiruppathi C, et al. Calcium-mediated stress kinase activation by DMP1 promotes osteoblast differentiation. J Biol Chem. 2010;285:36339–51.
Ravindran S, Narayanan K, Eapen AS, Hao J, Ramachandran A, Blond S, et al. Endoplasmic reticulum chaperone protein GRP-78 mediates endocytosis of dentin matrix protein 1. J Biol Chem. 2008;283:29658–70.
Ravindran S, Gao Q, Ramachandran A, Blond S, Predescu SA, et al. Stress chaperone GRP-78 functions in mineralized matrix formation. J Biol Chem. 2011;286:8729–39.
Narayanan K, Ramachandran A, Hao J, He G, Park KW, Cho M, et al. Dual functional roles of dentin matrix protein 1. Implications in biomineralization and gene transcription by activation of intracellular Ca2+ store. J Biol Chem. 2003;278:17500–8.
Qin C, Brunn JC, Cook RG, Orkiszewski RS, Malone JP, Veis A, et al. Evidence for the proteolytic processing of dentin matrix protein 1. Identification and characterization of processed fragments and cleavage sites. J Biol Chem. 2003;278:34700–8.
Sun Y, Lu Y, Chen L, Gao T, D’Souza R, Feng JQ, et al. DMP1 processing is essential to dentin and jaw formation. J Dent Res. 2011;90:619–24.
Steiglitz BM, Ayala M, Narayanan K, George A, Greenspan DS. Bone morphogenetic protein-1/tolloid-like proteinases process dentin matrix protein-1. J Biol Chem. 2004;279:980–6.
Hassan AH, Evans CA, Zaki AM, George A. Use of bone morphogenetic protein-2 and dentin matrix protein-1 to enhance the osteointegration of the onplant system. Connect Tissue Res. 2003;44:30–41.
Qin C, Brunn JC, Jones J, George A, Ramachandran A, Gorski JP, et al. A comparative study of sialic acid-rich proteins in rat bone and dentin. Eur J Oral Sci. 2001;109:133–41.
Wang X, Wang J, Yuan B, Lu Y, Feng JQ, Qin C. Overexpression of Dmp1 fails to rescue the bone and dentin defects in Fam20C knockout mice. Connect Tissue Res. 2014;55:299–303.
Acknowledgements
Thanks to the lab for technical support and the support of the leaders. The study was supported by the National Natural Science Foundation of China (No. 81271162) and the Provincial Natural Science Foundation (No. 1708085MH194).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no financial conflicts of interest.
Ethical statement
The experiment was carried out after being approved by the Ethics Review Committee of Anhui Medical University (No. 20160130). All authors gave their informed consent to all matters related to the publication of this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ma, D., Wang, Y., Chen, Y. et al. Promoting Osseointegration of Dental Implants in Dog Maxillary Sinus Floor Augmentation Using Dentin Matrix Protein 1-Transduced Bone Marrow Stem Cells. Tissue Eng Regen Med 17, 705–715 (2020). https://doi.org/10.1007/s13770-020-00277-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13770-020-00277-1