Abstract
Introduction
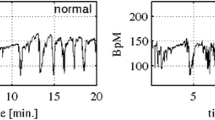
Cardiotocography (CTG) consists of two biophysical signals that are fetal heart rate (FHR) and uterine contraction (UC). In this research area, the computerized systems are usually utilized to provide more objective and repeatable results.
Materials and Methods
Feature selection algorithms are of great importance regarding the computerized systems to not only reduce the dimension of feature set but also to reveal the most relevant features without losing too much information. In this paper, three filters and two wrappers feature selection methods and machine learning models, which are artificial neural network (ANN), k-nearest neighbor (kNN), decision tree (DT), and support vector machine (SVM), are evaluated on a high dimensional feature set obtained from an open-access CTU-UHB intrapartum CTG database. The signals are divided into two classes as normal and hypoxic considering umbilical artery pH value (pH < 7.20) measured after delivery. A comprehensive diagnostic feature set forming the features obtained from morphological, linear, nonlinear, time–frequency and image-based time–frequency domains is generated first. Then, combinations of the feature selection algorithms and machine learning models are evaluated to achieve the most effective features as well as high classification performance.
Results
The experimental results show that it is possible to achieve better classification performance using lower dimensional feature set that comprises of more related features, instead of the high-dimensional feature set. The most informative feature subset was generated by considering the frequency of selection of the features by feature selection algorithms. As a result, the most efficient results were produced by selected only 12 relevant features instead of a full feature set consisting of 30 diagnostic indices and SVM model. Sensitivity and specificity were achieved as 77.40% and 93.86%, respectively.
Conclusion
Consequently, the evaluation of multiple feature selection algorithms resulted in achieving the best results.




Similar content being viewed by others
References
Grivell RM, Alfirevic Z, Gyte GM, Devane D. Antenatal cardiotocography for fetal assessment. Cochrane Database Syst Rev. 2010;9:1–48. https://doi.org/10.1002/14651858.CD007863.pub2.
Strachan BK, Sahota DS, Van Wijngaarden WJ, James DK, Chang AMZ. Computerised analysis of the fetal heart rate and relation to acidaemia at delivery. Br J Obstet Gynaecol. 2001;108:848–52. https://doi.org/10.1016/S0306-5456(00)00195-9.
Pinas A, Chandraharan E. Continuous cardiotocography during labour: analysis, classification and management. Best Pract. Res. Clin. Obstet. Gynaecol. 2016;30:33–47. https://doi.org/10.1016/j.bpobgyn.2015.03.022.
Norén H, Amer-Wåhlin I, Hagberg H, Herbst A, Kjellmer I, Marşál K, Olofsson P, Rosén KG. Fetal electrocardiography in labor and neonatal outcome: data from the Swedish randomized controlled trial on intrapartum fetal monitoring. Am J Obstet Gynecol. 2017;188:183–92. https://doi.org/10.1067/mob.2003.109.
Georgoulas G, Karvelis P, Spilka J, Chudáček V, Stylios CD, Lhotská L. Investigating pH based evaluation of fetal heart rate (FHR) recordings. Health Technol. (Berl). 2017;7:241–54. https://doi.org/10.1007/s12553-017-0201-7.
Bernardes J, Costa-Pereira A, Ayres-De-Campos D, Van Geijn HP, Pereira-Leite L. Evaluation of interobserver agreement of cardiotocograms. Int. J. Gynecol. Obstet. 1997;57:33–7. https://doi.org/10.1016/S0020-7292(97)02846-4.
Donker DK, van Geijn HP, Hasman A. Interobserver variation in the assessment of fetal heart rate recordings. Eur J Obstet Gynecol Reprod Biol. 1993;52:21–8. https://doi.org/10.1016/0028-2243(93)90220-7.
Czabanski R, Jezewski J, Matonia A, Jezewski M. Computerized analysis of fetal heart rate signals as the predictor of neonatal acidemia. Expert Syst Appl. 2012;39:11846–60. https://doi.org/10.1016/j.eswa.2012.01.196.
Ayres-de-Campos D, Spong CY, Chandraharan E. FIGO consensus guidelines on intrapartum fetal monitoring: cardiotocography. Int. J. Gynecol. Obstet. 2015;131:13–24. https://doi.org/10.1016/j.ijgo.2015.06.020.
Rhose S, Heinis AMF, Vandenbussche F, van Drongelen J, van Dillen J. Inter- and intra-observer agreement of non-reassuring cardiotocography analysis and subsequent clinical management. Acta Obstet Gynecol Scand. 2014;93:596–602. https://doi.org/10.1111/aogs.12371.
Ayres-de-Campos D, Ugwumadu A, Banfield P, Lynch P, Amin P, Horwell D, Costa A, Santos C, Bernardes J, Rosen K. A randomised clinical trial of intrapartum fetal monitoring with computer analysis and alerts versus previously available monitoring. BMC Pregnancy Childbirth. 2010;10:71. https://doi.org/10.1186/1471-2393-10-71.
Zhao Z, Zhang Y, Comert Z, Deng Y. Computer-aided diagnosis system of fetal hypoxia incorporating recurrence plot with convolutional neural network. Front. Physiol. 2019;10:255. https://doi.org/10.3389/fphys.2019.00255.
Signorini MG, Magenes G, Cerutti S, Arduini D. Linear and nonlinear parameters for the analysis of fetal heart rate signal from cardiotocographic recordings. IEEE Trans Biomed Eng. 2003;50:365–74. https://doi.org/10.1109/TBME.2003.808824.
Karin J, Hirsch M, Sagiv C, Akselrod S. Fetal autonomic nervous system activity monitoring by spectral analysis of heart rate variations. In: Proceedings of computers in cardiology; 1992. p. 479–482. https://doi.org/10.1109/cic.1992.269517.
Zarmehri MN, Castro L, Santos J, Bernardes J, Costa A, Santos CC. On the prediction of foetal acidaemia: a spectral analysis-based approach. Comput Biol Med. 2019;109:235–41. https://doi.org/10.1016/j.compbiomed.2019.04.041
Romagnoli S, Sbrollini A, Burattini L, Marcantoni I, Morettini M, Burattini L. Digital cardiotocography: what is the optimal sampling frequency? Biomed Signal Process Control. 2019;51:210–5. https://doi.org/10.1016/j.bspc.2019.02.016.
Cömert Z, Kocamaz AF. Cardiotocography analysis based on segmentation-based fractal texture decomposition and extreme learning machine. In: 25th Signal processing and communications applications conference; 2017. p. 1–4. https://doi.org/10.1109/siu.2017.7960397.
Cömert Z, Kocamaz AF, Subha V. Prognostic model based on image-based time–frequency features and genetic algorithm for fetal hypoxia assessment. Comput Biol Med. 2018. https://doi.org/10.1016/j.compbiomed.2018.06.003.
Cömert Z, Kocamaz AF. A study based on gray level co-occurrence matrix and neural network community for determination of hypoxic fetuses. In: International artificial intelligence and data processing symposium, TR, 2016. p. 569–573. https://doi.org/10.13140/rg.2.2.23901.00489.
Usha Sri A, Malini M, Chandana G. Feature extraction of cardiotocography signal. In: Satapathy SC, Raju KS, Shyamala K, Krishna DR, Favorskaya MN, editors. Advances in decision sciences, image processing, security and computer vision. Cham: Springer; 2020. p. 74–81.
Alkhasawneh MS. Hybrid cascade forward neural network with elman neural network for disease prediction. Arab J Sci. Eng. 2019. https://doi.org/10.1007/s13369-019-03829-3.
Cömert Z, Kocamaz AF. Evaluation of fetal distress diagnosis during delivery stages based on linear and nonlinear features of fetal heart rate for neural network community. Int J Comput Appl. 2016;156:26–31. https://doi.org/10.5120/ijca2016912417.
Alsayyari A. Fetal cardiotocography monitoring using Legendre neural networks. Biomed. Eng. Tech. 2019;100000:10000. https://doi.org/10.1515/bmt-2018-0074.
Uzun A, Kızıltas CE, Yılmaz E. Cardiotocography data set classification with extreme learning machine. In: International conference on advanced technologies, computer engineering and science; 2018. p. 224–230.
Cömert Z, Kocamaz AF. Comparison of machine learning techniques for fetal heart rate classification. Acta Phys Pol, A. 2017;132:451–4. https://doi.org/10.12693/aphyspola.131.451.
Stylios CD, Georgoulas G, Karvelis P, Spilka J, Chudáček V, Lhotska L. Least squares support vector machines for FHR classification and assessing the pH based categorization. In: Kyriacou E, Christofides S, Pattichis CS, editors. XIV Mediterranean conference on medical and biological engineering and computing, 2016 (MEDICON 2016), 31 March–2 April 2016, Paphos, Cyprus. Cham: Springer; 2016. p. 1211–1215. https://doi.org/10.1007/978-3-319-32703-7_234.
Spilka J, Frecon J, Leonarduzzi R, Pustelnik N, Abry P, Doret M. Sparse support vector machine for intrapartum fetal heart rate classification. IEEE J. Biomed. Heal. Inform. 2016;10000:10000. https://doi.org/10.1109/JBHI.2016.2546312.
Xu L, Georgieva A, Redman CWG, Payne SJ. Feature selection for computerized fetal heart rate analysis using genetic algorithms. In: 2013 35th Annual international conference of the IEEE Engineering in Medicine and Biology Society; 2013. pp. 445–448. https://doi.org/10.1109/embc.2013.6609532.
Cömert Z, Kocamaz AF. Novel software for comprehensive analysis of cardiotocography signals CTG-OAS. In: Karci A, editor. International conference on artificial intelligence and data processing. Malatya: IEEE; 2017. p. 1–6. https://doi.org/10.1109/idap.2017.8090210.
Chudacek V, Spilka J, Rubackova B, Koucky M, Georgoulas G, Lhotska L, Stylios C. Evaluation of feature subsets for classification of cardiotocographic recordings. In: 35th Annual conference on computers in cardiology 2008. Piscataway, NJ: IEEE; 2008. p. 845–848. https://doi.org/10.1109/cic.2008.4749174.
Menai MEB, Mohder FJ. Al-mutairi, Influence of feature selection on naïve Bayes classifier for recognizing patterns in cardiotocograms. J. Med. Bioeng. 2013;2:66–70. https://doi.org/10.12720/jomb.2.1.66-70.
Chudáček V, Spilka J, Burša M, Janků P, Hruban L, Huptych M, Lhotská L. Open access intrapartum CTG database. BMC Pregnancy Childbirth. 2014;14:16. https://doi.org/10.1186/1471-2393-14-16.
Gonçalves H, Bernardes J, Paula Rocha A, Ayres-de-Campos D. Linear and nonlinear analysis of heart rate patterns associated with fetal behavioral states in the antepartum period. Early Hum Dev. 2007;83:585–91. https://doi.org/10.1016/j.earlhumdev.2006.12.006.
Spilka J, Chudáček V, Koucký M, Lhotská L, Huptych M, Janků P, Georgoulas G, Stylios C. Using nonlinear features for fetal heart rate classification. Biomed Signal Process Control. 2012;7:350–7. https://doi.org/10.1016/j.bspc.2011.06.008.
Huang M-L, Yung-Yan H. Fetal distress prediction using discriminant analysis, decision tree, and artificial neural network. J. Biomed. Sci. Eng. 2012;05:526–33. https://doi.org/10.4236/jbise.2012.59065.
Sahin H, Subasi A. Classification of the cardiotocogram data for anticipation of fetal risks using machine learning techniques. Appl. Soft Comput. 2015;33:231–8. https://doi.org/10.1016/j.asoc.2015.04.038.
Aha DW, Kibler D, Albert MK. Instance-based learning algorithms. Mach. Learn. 1991;6:37–66. https://doi.org/10.1007/BF00153759.
Akbulut Y, Sengur A, Guo Y, Smarandache F. NS-k-NN: neutrosophic set-based k-nearest neighbors classifier. Symmetry (Basel). 2017;9:179.
Safavian SR, Landgrebe D. A survey of decision tree classifier methodology. IEEE Trans. Syst. Man. Cybern. 1991;21:660–74.
Altuntaş Y, Kocamaz AF, Cömert Z, Cengiz R, Esmeray M. Identification of haploid maize seeds using gray level co-occurrence matrix and machine learning techniques. In: 2018 International conference on artificial intelligence and data Processing, Malatya, Turkey; 2018. p. 1–5. https://doi.org/10.1109/idap.2018.8620740
Cömert Z, Kocamaz AF. Fetal hypoxia detection based on deep convolutional neural network with transfer learning approach. In: Silhavy R, editor. Software engineering and algorithms in intelligent systems. Cham: Springer; 2019. p. 239–248. https://doi.org/10.1007/978-3-319-91186-1_25.
Subha V, Murugan D, Boopathi AM, Velappan S, Murugan D, Boopathi M. A hybrid filter-wrapper attribute reduction approach for fetal risk anticipation. Asian J. Res. Soc. Sci. Humanit. 2017;7:1094–106.
Velappan S, Murugan D, Prabha S, Boopathi M. Genetic Algorithm based feature subset selection for fetal state classification. J. Commun. Technol. Electron. Comput. Sci. 2015;2:13–7.
Ayres-de-campos D, Bernardes J, Garrido A, Marques-de-sá J, Pereira-leite L. SisPorto 2.0: a program for automated analysis of cardiotocograms. J. Matern. Fetal. Med. 2000;9:311–8. https://doi.org/10.3109/14767050009053454.
Spilka J, Georgoulas G, Karvelis P, Oikonomou VP, Chudáček V, Stylios C, Lhotská L, Jankru P. Automatic evaluation of FHR recordings from CTU-UHB CTG database. In: Bursa M, Khuri S, Renda ME, editors. Proceedings of 4th international conference on information technology in bio- and medical informatics (ITBAM 2013), Prague, Czech Republic, 28 August 2013. Berlin: Springer, 2013, pp. 47–61. https://doi.org/10.1007/978-3-642-40093-3_4.
Acknowledgements
We would like to thanks to Dr. Sami Güngör due to its comments on the medical background.
Funding
There is no funding source for this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that there is no conflict to interest related to this paper.
Ethical approval
This article does not contain any data, or other information from studies or experimentation, with the involvement of human or animal subjects.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cömert, Z., Şengür, A., Budak, Ü. et al. Prediction of intrapartum fetal hypoxia considering feature selection algorithms and machine learning models. Health Inf Sci Syst 7, 17 (2019). https://doi.org/10.1007/s13755-019-0079-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13755-019-0079-z