Abstract
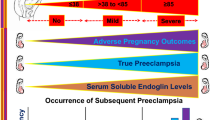
There are few case reports in which circulating levels of soluble fms-like tyrosine kinase 1 (sFlt-1), placental growth factor (PlGF), and soluble endoglin (sEng) were measured before the onset of super-imposed preeclampsia in women with hemodialysis. A 40-year-old Japanese nulliparous women with hemodialysis due to diabetic nephropathy became pregnant by frozen embryo transfer. Intensive hemodialysis was started at 5 weeks of gestation. Her blood pressure (BP) in the first trimester was around 130/80 mmHg. At 20+3 weeks, she was admitted for close monitoring; her BP was 137/75 mmHg. Her BP increased to 157/88 mmHg at 31+2 weeks, and nifedipine at 20 mg/day was started at 31+6 weeks. However, the serial longitudinal measurements of sFlt-1, PlGF, and sEng did not predict the onset of super-imposed preeclampsia. Cesarean section was performed at 33+6 weeks due to uncontrollable hypertension. A healthy female infant weighing 2138 g was delivered. As for the changes of biomarkers between just before and just after hemodialysis, sFlt-1 was significantly higher just after compared with just before hemodialysis (5774 ± 1875 pg/mL vs. 2960 ± 905 pg/mL, respectively, p < 0.001). PlGF was also significantly higher just after compared with just before hemodialysis (2227 ± 1038 pg/mL vs. 1377 ± 614 pg/mL, respectively, p < 0.001). However, the sFlt-1/PlGF ratio and sEng levels were not significantly different between just before and just after hemodialysis (p = 0.115, p = 0.672, respectively). In conclusion, prediction of early-onset super-imposed preeclampsia using angiogenic and anti-angiogenic markers in pregnant women with hemodialysis might be difficult.


Similar content being viewed by others
References
Hirose N, Ohkuchi A, Usui R, Matsubara S, Suzuki M. Risk of preeclampsia in women with CKD, dialysis or kidney transplantation. Med J Obstet Gynecol. 2014;2:1028.
Luders C, Castro MC, Titan SM, De Castro I, Elias RM, Abensur H, Romão JE Jr. Obstetric outcome in pregnant women on long-term dialysis: a case series. Am J Kidney Dis. 2010;56:77–85.
Shahir AK, Briggs N, Katsoulis J, Levidiotis V. An observational outcomes study from 1966–2008, examining pregnancy and neonatal outcomes from dialysed women using data from the ANZDATA Registry. Nephrol (Carlton). 2013;18:276–84.
Eroğlu D, Lembet A, Ozdemir FN, Ergin T, Kazanci F, Kuşcu E, Haberal M. Pregnancy during hemodialysis: perinatal outcome in our cases. Transplant Proc. 2004;36:53–5.
Malik GH, Al-Harbi A, Al-Mohaya S, Dohaimi H, Kechrid M, Shetaia MS, Al-Hassan AO, Quiapos LS. Pregnancy in patients on dialysis–experience at a referral center. J Assoc Phys India. 2005;53:937–41.
Piccoli GB, Conijn A, Consiglio V, Vasario E, Attini R, Deagostini MC, Bontempo S, Todros T. Pregnancy in dialysis patients: is the evidence strong enough to lead us to change our counseling policy? Clin J Am Soc Nephrol. 2010;5:62–71.
Piccoli GB, Minelli F, Versino E, Cabiddu G, Attini R, Vigotti FN, Rolfo A, Giuffrida D, Colombi N, Pani A, Todros T. Pregnancy in dialysis patients in the new millennium: a systematic review and meta-regression analysis correlating dialysis schedules and pregnancy outcomes. Nephrol Dial Transplant. 2016;31:1915–34.
Wiles K, de Oliveira L. Dialysis in pregnancy. Best Pract Res Clin Obstet Gynaecol. 2019;57:33–46.
Levine RJ, Maynard SE, Qian C, Lim KH, England LJ, Yu KF, Schisterman EF, Thadhani R, Sachs BP, Epstein FH, Sibai BM, Sukhatme VP, Karumanchi SA. Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med. 2004;350:672–83.
Levine RJ, Lam C, Qian C, Yu KF, Maynard SE, Sachs BP, Sibai BM, Epstein FH, Romero R, Thadhani R, Karumanchi SA, CPEP Study Group. Soluble endoglin and other circulating antiangiogenic factors in preeclampsia. N Engl J Med. 2006;355:992–1005.
Ohkuchi A, Hirashima C, Matsubara S, Takahashi K, Matsuda Y, Suzuki M. Threshold of soluble fms-like tyrosine kinase 1/placental growth factor ratio for the imminent onset of preeclampsia. Hypertension. 2011;58:859–66.
Ohkuchi A, Hirashima C, Takahashi K, Suzuki H, Matsubara S, Suzuki M. Onset threshold of the plasma levels of soluble fms-like tyrosine kinase 1/placental growth factor ratio for predicting the imminent onset of preeclampsia within 4 weeks after blood sampling at 19-31 weeks of gestation. Hypertens Res. 2013;36:1073–80.
Shan HY, Rana S, Epstein FH, Stillman IE, Karumanchi SA, Williams ME. Use of circulating antiangiogenic factors to differentiate other hypertensive disorders from preeclampsia in a pregnant woman on dialysis. Am J Kidney Dis. 2008;51:1029–32.
Cornelis T, Spaanderman M, Beerenhout C, Perschel FH, Verlohren S, Schalkwijk CG, van der Sande FM, Kooman JP, Hladunewich M. Antiangiogenic factors and maternal hemodynamics during intensive hemodialysis in pregnancy. Hemodial Int. 2013;17:639–43.
Akbari A, Hladunewich M, Burns K, Moretti F, Arkoub RA, Brown P, Hiremath S. Circulating angiogenic factors in a pregnant woman on intensive hemodialysis: a case report. Can J Kidney Health Dis. 2016;3:7.
Lavainne F, Meffray E, Pepper RJ, Néel M, Delcroix C, Salama AD, Fakhouri F. Heparin use during dialysis sessions induces an increase in the antiangiogenic factor soluble Flt1. Nephrol Dial Transplant. 2014;29:1225–31.
Hagmann H, Bossung V, Belaidi AA, Fridman A, Karumanchi SA, Thadhani R, Schermer B, Mallmann P, Schwarz G, Benzing T, Brinkkoetter PT. Low-molecular weight heparin increases circulating sFlt-1 levels and enhances urinary elimination. PLoS ONE. 2014;9:e85258.
Hirashima C, Ohkuchi A, Takahashi K, Suzuki H, Yoshida M, Ohmaru T, Eguchi K, Ariga H, Matsubara S, Suzuki M. Gestational hypertension as a subclinical preeclampsia in view of serum levels of angiogenesis-related factors. Hypertens Res. 2011;34:212–7.
Yinon Y, Ben Meir E, Margolis L, Lipitz S, Schiff E, Mazaki-Tovi S, Simchen MJ. Low molecular weight heparin therapy during pregnancy is associated with elevated circulatory levels of placental growth factor. Placenta. 2015;36:121–4.
Drewlo S, Levytska K, Sobel M, Baczyk D, Lye SJ, Kingdom JC. Heparin promotes soluble VEGF receptor expression in human placental villi to impair endothelial VEGF signaling. J Thromb Haemost. 2011;9:2486–97.
Acknowledgements
This work was supported by Grants-in-Aid (24592482 and 17K11247 to A.O.) from the Ministry of Education, Culture, Sports, Science and Technology, Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that there are no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Human and animal rights
This is a research involving a human being. All procedures performed in this study were in accordance with the ethical standards of the institutional research committee at which the studies were conducted (IRB approval number: Dai-I-17-Hen-29-Gou) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
A written informed consent was gained from the patient.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Morisawa, H., Hirashima, C., Sano, M. et al. Difficulty of predicting early-onset super-imposed preeclampsia in pregnant women with hemodialysis due to diabetic nephropathy by serum levels of sFlt-1, PlGF, and sEng. CEN Case Rep 9, 101–105 (2020). https://doi.org/10.1007/s13730-019-00435-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13730-019-00435-y