Abstract
Purpose of Review
To improve recognition of skin and soft tissue infections caused by nontuberculous mycobacteria (NTM) and provide guidance on diagnostic work-up and treatment for the inpatient dermatologist, with a focus on recent literature (2018–2023).
Recent Findings
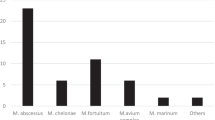
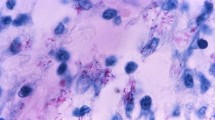
The prevalence of NTM skin and soft tissue infections has increased in the last few decades. Histopathology and tissue culture are imperative to make a diagnosis. Matrix-assisted laser deionization-time of flight mass spectrometry (MALDI-TOF MS) is used with increasing frequency to accelerate diagnosis of NTM. Dual antibiotic therapy is recommended to decrease resistance, particularly in rapidly growing bacteria (RGM).
Summary
NTM, particularly RGM, are rare sources of skin and soft tissue infections in hospitalized patients that have high morbidity and mortality. The inpatient dermatologist must maintain a high index of suspicion for NTM cutaneous lesions to initiate work-up and treatment.



Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Misch EA, Saddler C, Davis JM. Skin and soft tissue infections due to nontuberculous mycobacteria. Curr Infect Dis Rep. 2018 Mar 19;20(4):6. https://doi.org/10.1007/s11908-018-0611-3. PMID: 29556857. This review highlights advances in NTM diagnosis and treatment with a focus on M. chimaera and M. abscessus.
•• Sepulcri C, Vena A, Bassetti M. Skin and soft tissue infections due to rapidly growing mycobacteria. Curr Opin Infect Dis. 2023 Apr 1;36(2):74–80. https://doi.org/10.1097/QCO.0000000000000905. Epub 2023 Jan 30. PMID: 36718980. This review highlights literature on NTM SSTI from 2021 to 2022 with a focus on RGM species.
• Johansen MD, Herrmann JL, Kremer L. Non-tuberculous mycobacteria and the rise of Mycobacterium abscessus. Nat Rev Microbiol. 2020 Jul;18(7):392–407. https://doi.org/10.1038/s41579-020-0331-1. Epub 2020 Feb 21. PMID: 32086501. This paper focuses on virulence factors, mechanisms of drug resistance, and future therapeutic options in M. abscessus.
•• Chung J, Ince D, Ford BA, Wanat KA. Cutaneous infections due to nontuberculosis Mycobacterium: recognition and management. Am J Clin Dermatol. 2018 Dec;19(6):867–78. https://doi.org/10.1007/s40257-018-0382-5. PMID: 30168084. This review highlights the heterogenous presentation of cutaneous NTM based on species and provides guidelines for diagnosis and treatment.
• Daniau C, Lecorche E, Mougari F, Benmansour H, Bernet C, Blanchard H, et al. Association of healthcare and aesthetic procedures with infections caused by nontuberculous mycobacteria, France, 2012–2020. Emerg Infect Dis. 2022 Mar;28(3):518–26. https://doi.org/10.3201/eid2803.211791. PMID: 35195516; PMCID: PMC8888244. This paper discusses NTM infections associated with healthcare and aesthetic procedures in France during 2012–2020.
•• Ricotta EE, Adjemian J, Blakney RA, Lai YL, Kadri SS, Prevots DR. Extrapulmonary nontuberculous mycobacteria infections in hospitalized patients, United States, 2009–2014. Emerg Infect Dis. 2021 Mar;27(3):845–52. https://doi.org/10.3201/eid2703.201087. PMID: 33622461; PMCID: PMC7920686. The paper found modestly increased rates of SSTIs after studying 831 extrapulmonary NTM infections from 2009 to 2014.
Vongthilath-Moeung R, Plojoux J, Poncet A, Renzi G, Veziris N, Schrenzel J, et al. Nontuberculous mycobacteria under scrutiny in the Geneva area (2015–2020). Respiration. 2022;101(4):367–75. https://doi.org/10.1159/000520033. Epub 2021 Dec 7. PMID: 34875659.
• Tokunaga DS, Siu AM, Lim SY. Nontuberculous mycobacterial skin and soft tissue infection in Hawai’i. BMC Infect Dis. 2022 Apr 11;22(1):360. https://doi.org/10.1186/s12879-022-07345-y. PMID: 35410188; PMCID: PMC9004129. This study presents demographics, clinical course, and treatment outcomes of NTM SSTIs in Hawaiʻi.
•• Philips RC, Hoyer PE, White SM, Tinkey KT, Loeffelholz M, Andersen CR, et al. Cutaneous nontuberculous myobacteria infections: a retrospective case series of 78 patients from the Texas Gulf Coast region. J Am Acad Dermatol. 2019 Sep;81(3):730–9. https://doi.org/10.1016/j.jaad.2019.04.022. Epub 2019 Apr 16. PMID: 31002850. A study on NTM SSTIs in 78 patients found that immunosuppressed patients and M. abscessus had more persistent disease.
Chai J, Han X, Mei Q, Liu T, Walline JH, Xu J, et al. Clinical characteristics and mortality of non-tuberculous mycobacterial infection in immunocompromised vs. immunocompetent hosts. Front Med. 2022;9. https://doi.org/10.3389/fmed.2022.884446.
Chen H-H, Lin C-H, Chao W-C. Mortality association of nontuberculous mycobacterial infection requiring treatment in Taiwan: a population-based study. Ther Adv Respir Dis. 2022;16:17534666221103212. https://doi.org/10.1177/17534666221103213.
Sharma SK, Upadhyay V. Epidemiology, diagnosis & treatment of non-tuberculous mycobacterial diseases. Indian J Med Res. 2020 Sep;152(3):185–226. https://doi.org/10.4103/ijmr.IJMR_902_20. PMID: 33107481; PMCID: PMC7881820.
Longworth SA, Daly JS. Management of infections due to nontuberculous mycobacteria in solid organ transplant recipients-guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant. 2019 Sep;33(9):e13588. https://doi.org/10.1111/ctr.13588. Epub 2019 Jun 25. PMID: 31077618.
•• Hannah CE, Ford BA, Chung J, Ince D, Wanat KA. Characteristics of nontuberculous mycobacterial infections at a Midwestern tertiary hospital: a retrospective study of 365 patients. Open Forum Infect Dis. 2020 May 25;7(6):ofaa173. https://doi.org/10.1093/ofid/ofaa173. PMID: 32587875; PMCID: PMC7305701. This study provided information on the demographics, risk factors, and disease course of patients with NTM infections.
Falkinham IJO. Surrounded by mycobacteria: nontuberculous mycobacteria in the human environment. J Appl Microbiol. 2009;107(2):356–67. https://doi.org/10.1111/j.1365-2672.2009.04161.x.
Daley CL, Iaccarino JM, Lange C, Cambau E, Wallace RJ, Andrejak C, et al. Treatment of nontuberculous mycobacterial pulmonary disease: an official ATS/ERS/ESCMID/IDSA clinical practice guideline. Clin Infect Dis. 2020 Aug 14;71(4):905–13. https://doi.org/10.1093/cid/ciaa241. Erratum in: Clin Infect Dis. 2020 Dec 31;71(11):3023. PMID: 32628747; PMCID: PMC7768748.
Yeo PM, Lee SX, Tan YE, Sng LH, Ang CC. Epidemiology, risk factors, and outcomes of adult cutaneous non-tuberculous mycobacterial infection over a 10-year period in Singapore. Int J Dermatol. 2019 Jun;58(6):679–87. https://doi.org/10.1111/ijd.14356. Epub 2018 Dec 25. PMID: 30585309.
Atkins BL, Gottlieb T. Skin and soft tissue infections caused by nontuberculous mycobacteria. Curr Opin Infect Dis. 2014;27(2):137–45. https://doi.org/10.1097/qco.0000000000000041.
Sander MA, Isaac-Renton JL, Tyrrell GJ. Cutaneous nontuberculous mycobacterial infections in Alberta, Canada: an epidemiologic study and review. J Cutan Med Surg. 2018 Sep/Oct;22(5):479–83. https://doi.org/10.1177/1203475418776945. Epub 2018 May 17. PMID: 29772918.
Sitenga J, Patel N, Rainwater A. Cutaneous Mycobacterium haemophilum infection involving the upper extremities: diagnosis and management guidelines. Cutis. 2019 Oct;104(4):238–41. PMID: 31774883.
Forbes BA, Hall GS, Miller MB, Novak SM, Rowlinson M-C, Salfinger M, et al. Practical guidance for clinical microbiology laboratories: mycobacteria. Clin Microbiol Rev. 2018;31(2):e00038-e117. https://doi.org/10.1128/CMR.00038-17.
Li JJ, Beresford R, Fyfe J, Henderson C. Clinical and histopathological features of cutaneous nontuberculous mycobacterial infection: a review of 13 cases. J Cutan Pathol. 2017;44(5):433–43. https://doi.org/10.1111/cup.12903.
Choi HY, Lee MH, Lee JS, Song IH, Cho KJ. Isolated subcutaneous nontuberculous mycobacterial infection: a rare case initially mischaracterized as a soft tissue malignancy. Skeletal Radiol. 2018 May;47(5):735–42. https://doi.org/10.1007/s00256-017-2851-y. Epub 2017 Dec 22. PMID: 29273829.
Tyner HL, Wilson JW. Fifteen-year clinical experience with Mycobacterium haemophilum at the Mayo Clinic: a case series. J Clin Tuberc Other Mycobact Dis. 2017 Jun 28;8:26–32. https://doi.org/10.1016/j.jctube.2017.06.002. PMID: 31723708; PMCID: PMC6850245.
Lyman MM, Grigg C, Kinsey CB, Keckler MS, Moulton-Meissner H, Cooper E, et al. Invasive nontuberculous mycobacterial infections among cardiothoracic surgical patients exposed to heater-cooler devices. Emerg Infect Dis. 2017;23(5):796–805. https://doi.org/10.3201/eid2305.161899.
World Health Organization: Buruli ulcer (Mycobacterium ulcerans infection). https://www.who.int/news-room/fact-sheets/detail/buruli-ulcer-(mycobacterium-ulcerans-infection) (2023). Accessed 14 May 2023.
van der Werf TS, van der Graaf WT, Tappero JW, Asiedu K. Mycobacterium ulcerans infection. Lancet. 1999;354(9183):1013–8. https://doi.org/10.1016/s0140-6736(99)01156-3.
O’Brien RJ, Geiter LJ, Snider DE, Jr. The epidemiology of nontuberculous mycobacterial diseases in the United States. Results from a national survey. Am Review of Respir Dis. 1987 May;135(5):1007–14. https://doi.org/10.1164/arrd.1987.135.5.1007. PMID: 3579001.
Winthrop KL, McNelley E, Kendall B, Marshall-Olson A, Morris C, Cassidy M, et al. Pulmonary nontuberculous mycobacterial disease prevalence and clinical features: an emerging public health disease. Am J Respir Crit Care Med. 2010 Oct 1;182(7):977–82. https://doi.org/10.1164/rccm.201003-0503OC. Epub 2010 May 27. PMID: 20508209.
Marras TK, Chedore P, Ying AM, Jamieson F. Isolation prevalence of pulmonary non-tuberculous mycobacteria in Ontario, 1997 2003. Thorax. 2007;62(8):661–6. https://doi.org/10.1136/thx.2006.070797.
Wentworth AB, Drage LA, Wengenack NL, Wilson JW, Lohse CM. Increased incidence of cutaneous nontuberculous mycobacterial infection, 1980 to 2009: a population-based study. Mayo Clin Proc. 2013;88(1):38–45. https://doi.org/10.1016/j.mayocp.2012.06.029.
Hsueh JH, Fang SY, Hsieh YH, Chen LW, Lee SS. Failure among patients with non-tuberculous mycobacterial infections in skin, soft tissue, and musculoskeletal system in Southern Taiwan, 2012–2015. Surg Infect. 2019 Sep;20(6):492–8. https://doi.org/10.1089/sur.2018.314. Epub 2019 May 8. PMID: 31066636.
Moreno G, Minocha R, Choy B, Jelfs P, Watts M, Fernandez-Penas P. Cutaneous non-tuberculous mycobacteria in Western Sydney, Australia. Population study 1996–2013. Australas J Dermatol. 2018 Nov;59(4):343–5. https://doi.org/10.1111/ajd.12783. Epub 2018 Jan 26. PMID: 29372556.
Stienstra Y, van Roest MH, van Wezel MJ, Wiersma IC, Hospers IC, Dijkstra PU, et al. Factors associated with functional limitations and subsequent employment or schooling in Buruli ulcer patients. Trop Med Int Health. 2005;10(12):1251–7. https://doi.org/10.1111/j.1365-3156.2005.01519.x.
• Crothers JW, Laga AC, Solomon IH. Clinical performance of mycobacterial immunohistochemistry in anatomic pathology specimens: the beginning of the end for Ziehl-Neelsen? Am J Clin Pathol. 2020;155(1):97–105. https://doi.org/10.1093/ajcp/aqaa119. This study found that IHC identifies RGM and SGM with similar sensitivity and can streamline evaluation for cases suspicious for NTM.
Hooper J, Beltrami EJ, Santoro F, Murphy MJ. Remember the fite: a case of cutaneous Mycobacterium fortuitum infection. Am J Dermatopathol. 2023 Mar 1;45(3):214–5. https://doi.org/10.1097/DAD.0000000000002336. Epub 2022 Dec 7. PMID: 36729795.
• Luo L, Liang L, Zhang R, Chen W, Yu F, Zhao Y, et al. Using Vitek MS v3.0 to identify nontuberculous mycobacteria in liquid media in a clinical microbiology laboratory. Microbiol Spectr. 2022;10(6):e0201822. https://doi.org/10.1128/spectrum.02018-22. This study evaluates the performance of the Vitek MS v3.0 MALDI-TOF MS by isolating NTM directly from automated liquid medium systems.
Gonzaleza-Santiago TM, Drage LA. Nontuberculous mycobacteria: skin and soft tissue infections. Dermatol Clin. 2015;33(3):563–77. https://doi.org/10.1016/j.det.2015.03.017.
Piersimoni C, Scarparo C. Extrapulmonary infections associated with nontuberculous mycobacteria in immunocompetent persons. Emerg Infect Dis. 2009;15(9):1351–8; quiz 544. https://doi.org/10.3201/eid1509.081259.
Leto Barone AA, Grzelak MJ, Frost C, Ngaage LM, Ge S, Kolegraff K, et al. Atypical mycobacterial infections after plastic surgery procedures abroad: a multidisciplinary algorithm for diagnosis and treatment. Ann Plast Surg. 2020;84(3):257–62. https://doi.org/10.1097/sap.0000000000002061.
Gaudêncio M, Carvalho A, Bertão MI, Barreiro I, Bessa MI, Gonçalves A. Mycobacterium chelonae cutaneous infection: a challenge for an internist. Eur J Case Rep Intern Med. 2021;8(11):003013. https://doi.org/10.12890/2021_003013.
Akram SM, Rathish B, Saleh D. Mycobacterium Chelonae. StatPearls. Treasure Island (FL): StatPearls Publishing. Copyright© 2023, StatPearls Publishing LLC; 2023.
Han VX, Loke KY, Chan SM. Recurrent Mycobacterium fortuitum insulin injection site abscesses. J Paediatr Child Health. 2018 Mar;54(3):316–8. https://doi.org/10.1111/jpc.13788. Epub 2017 Nov 23. PMID: 29168906.
Stewart A. Disseminated Mycobacterium intracellulare from a deep cutaneous infection. Int J Mycobacteriol. 2019;8(1):98–100. https://doi.org/10.4103/ijmy.ijmy_17_19.
•• Hunkins JJ, de-Moura VC, Eddy JJ, Daley CL, Khare R. In vitro susceptibility patterns for rapidly growing nontuberculous mycobacteria in the United States. Diagn Microbiol Infect Dis. 2023 Mar;105(3):115882. https://doi.org/10.1016/j.diagmicrobio.2022.115882. Epub 2022 Dec 15. PMID: 36610383. This study developed a cumulative antibiogram for 14 RGM species.
Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007;175(4):367–416. https://doi.org/10.1164/rccm.200604-571ST.
O’Brien DP, Jenkin G, Buntine J, Steffen CM, McDonald A, Horne S, et al. Treatment and prevention of Mycobacterium ulcerans infection (Buruli ulcer) in Australia: guideline update. Med J Aust. 2014;200(5):267–70. https://doi.org/10.5694/mja13.11331.
Strobel K, Sickenberger C, Schoen C, Kneitz H, Kolb-Maurer A, Goebeler M. Diagnosis and therapy of Mycobacterium marinum: a single-center 21-year retrospective analysis. J Dtsch Dermatol Ges. 2022 Sep;20(9):1211–8. https://doi.org/10.1111/ddg.14847. Epub 2022 Aug 24. PMID: 36000770.
Author information
Authors and Affiliations
Contributions
Amber Bo and Laura Goeser were responsible for the primary writing of the manuscript, and all 3 authors prepared figures. Karolyn Wanat was responsible for critical review and appraisal. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bo, A.Y., Goeser, L.E. & Wanat, K.A. Nontuberculous Mycobacterial Infections and Management for the Inpatient Dermatologist. Curr Derm Rep 12, 204–214 (2023). https://doi.org/10.1007/s13671-023-00417-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13671-023-00417-5