Abstract
Purpose of Review
The purpose of this narrative review article is to describe the current literature on the psoriasis inpatient population, discuss considerations for admission, and provide updated recommendations for inpatient psoriasis workup, management, and post-discharge follow-up.
Recent Findings
Studies report variable rates of psoriasis hospitalizations in the last decade even with the advent of highly efficacious outpatient therapies. Inequities in access to these therapies have resulted in disparities in the psoriasis inpatient population. Patients with severe variants of psoriasis, including generalized pustular and erythrodermic psoriasis, often have severe systemic complications and require immediate stabilization and supportive care. Traditional, rapid acting systemic therapies, including cyclosporine and infliximab, are efficacious, though the interleukin-17 inhibitors, secukinumab, ixekizumab, and brodalumab, may represent reasonable options. The interleukin-36 inhibitor, spesolimab, is a new and promising therapy under investigation for generalized pustular psoriasis.
Summary
Psoriasis patients presenting with severe variants of disease, including pustular and erythrodermic psoriasis, in combination with systemic findings such as infection or compromised hemodynamic status, require hospitalization. Supportive measures to address systemic signs and complications are needed. Topical treatments with rapid acting systemic therapies should be employed to improve skin symptoms. Racial, ethnic, and insurance disparities exist in the hospitalized psoriasis patient population, highlighting the need for providers to obtain thorough sociodemographic histories and establish strong therapeutic alliances with these patients, identifying stable treatment options to prevent future exacerbations and hospitalizations.
Similar content being viewed by others

References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Zachariae R, Zachariae C, Ibsen HHW, Mortensen JT, Wulf HC. Psychological symptoms and quality of life of dermatology outpatients and hospitalized dermatology patients. Acta Derm Venereol. 2004;84(3):205–12. https://doi.org/10.1080/00015550410023284.
Vensel E, Hilley T, Trent J, et al. Sustained improvement of the quality of life of patients with psoriasis after hospitalization. J Am Acad Dermatol. 2000;43(5 Pt 1):858–60. https://doi.org/10.1067/mjd.2000.106512.
Ayyalaraju RS, Finlay AY, Dykes PJ, Trent JT, Kirsner RS, Kerdel FA. Hospitalization for severe skin disease improves quality of life in the United Kingdom and the United States: a comparative study. J Am Acad Dermatol. 2003;49(2):249–54. https://doi.org/10.1067/s0190-9622(03)00897-1.
• Polivka L, Oubaya N, Bachelez H, et al. Trends in hospitalization rates for psoriasis flares since the introduction of biologics: a time series in France between 2005 and 2015. J Eur Acad Dermatol Venereol. 2018;32(11):1920–9. https://doi.org/10.1111/jdv.15044. (Importance: This study reviewed all inpatient stays for psoriasis flares in nine French hospitals between 2005 and 2015 and used segmented linear regression models to determine the impact of new biologic therapies on hospitalization rates in patients with psoriasis, showing a positive change in the level of the psoriasis hospitalization rate after 2010.)
Hsu DY, Gordon K, Silverberg JI. The inpatient burden of psoriasis in the United States. J Am Acad Dermatol. 2016;75(1):33–41. https://doi.org/10.1016/j.jaad.2016.03.048.
Nelson AA, Pearce DJ, Fleischer AB, Balkrishnan R, Feldman SR. Inpatient management of severe psoriasis. J Drugs Dermatol. 2005;4(5):564–70.
Stern RS, PUVA Follow-up Study. Inpatient hospital care for psoriasis: a vanishing practice in the United States. J Am Acad Dermatol. 2003;49(3):445–450. https://doi.org/10.1067/s0190-9622(03)00858-2.
Hsu DY, Gordon K, Silverberg JI. Serious infections in hospitalized patients with psoriasis in the United States. J Am Acad Dermatol. 2016;75(2):287–96. https://doi.org/10.1016/j.jaad.2016.04.005.
Varman KM, Namias N, Schulman CI, Pizano LR. Acute generalized pustular psoriasis, von Zumbusch type, treated in the burn unit. A review of clinical features and new therapeutics. Burns. 2014;40(4):e35–39. https://doi.org/10.1016/j.burns.2014.01.003.
Choon SE, Lai NM, Mohammad NA, Nanu NM, Tey KE, Chew SF. Clinical profile, morbidity, and outcome of adult-onset generalized pustular psoriasis: analysis of 102 cases seen in a tertiary hospital in Johor. Malaysia Int J Dermatol. 2014;53(6):676–84. https://doi.org/10.1111/ijd.12070.
Shuster S. High-output cardiac failure from skin disease. Lancet. 1963;1(7295):1338–40. https://doi.org/10.1016/s0140-6736(63)91921-4.
Voigt GC, Kronthal HL, Crounse RG. Cardiac output in erythrodermic skin disease. Am Heart J. 1966;72(5):615–20. https://doi.org/10.1016/0002-8703(66)90344-9.
Boyd AS, Menter A. Erythrodermic psoriasis. Precipitating factors, course, and prognosis in 50 patients. J Am Acad Dermatol. 1989;21(5 Pt 1):985–991.
Saeki H, Watanabe A, Tada Y, et al. Juvenile pustular psoriasis associated with steroid withdrawal syndrome due to topical corticosteroid. J Dermatol. 2008;35(9):601–3. https://doi.org/10.1111/j.1346-8138.2008.00531.x.
Heinrich M, Cook E, Roach J, et al. Erythrodermic psoriasis secondary to systemic corticosteroids. Proc (Bayl Univ Med Cent). 2020;33(1):113–4. https://doi.org/10.1080/08998280.2019.1686911.
Gregoire ARF, DeRuyter BK, Stratman EJ. Psoriasis flares following systemic glucocorticoid exposure in patients with a history of psoriasis. JAMA Dermatol. 2021;157(2):198. https://doi.org/10.1001/jamadermatol.2020.4219.
Rosenbach M, Hsu S, Korman NJ, et al. Treatment of erythrodermic psoriasis: from the medical board of the National Psoriasis Foundation. J Am Acad Dermatol. 2010;62(4):655–62. https://doi.org/10.1016/j.jaad.2009.05.048.
Esposito M, Saraceno R, Schipani C, Di Marcantonio D, Bianchi L, Chimenti S. Trimethoprim-sulfamethoxazole induced erythrodermic psoriasis. J Infect. 2008;57(1):90–2. https://doi.org/10.1016/j.jinf.2008.04.005.
Lemmenmeier E, Gaus B, Schmid P, Hoffmann M. A case of erythrodermia from exacerbated psoriasis vulgaris due to treatment of acute hepatitis C. BMC Dermatol. 2016;16(1):5. https://doi.org/10.1186/s12895-016-0042-5.
Takeichi T, Akiyama M. Generalized pustular psoriasis: clinical management and update on autoinflammatory aspects. Am J Clin Dermatol. 2020;21(2):227–36. https://doi.org/10.1007/s40257-019-00492-0.
Liao W, Singh R, Lee K, et al. Erythrodermic psoriasis: pathophysiology and current treatment perspectives. PTT. 2016;6:93–104. https://doi.org/10.2147/PTT.S101232.
Mistry N, Gupta A, Alavi A, Sibbald RG. A review of the diagnosis and management of erythroderma (generalized red skin). Adv Skin Wound Care. 2015;28(5):228–36. https://doi.org/10.1097/01.ASW.0000463573.40637.73.
Tomasini C, Aloi F, Solaroli C, Pippione M. Psoriatic erythroderma: a histopathologic study of forty-five patients. Dermatology. 1997;194(2):102–6. https://doi.org/10.1159/000246075.
Twelves S, Mostafa A, Dand N, et al. Clinical and genetic differences between pustular psoriasis subtypes. J Allergy Clin Immunol. 2019;143(3):1021–6. https://doi.org/10.1016/j.jaci.2018.06.038.
Allez M, Roux ME, Bertheau P, et al. Recurrent cholestatic jaundice associated with generalized pustular psoriasis: evidence for a neutrophilic cholangitis. J Hepatol. 2000;33(1):160–2. https://doi.org/10.1016/s0168-8278(00)80174-9.
Li SP, Tang WY, Lam WY, Wong SN. Renal failure and cholestatic jaundice as unusual complications of childhood pustular psoriasis. Br J Dermatol. 2000;143(6):1292–6. https://doi.org/10.1046/j.1365-2133.2000.03904.x.
Fujita H, Terui T, Hayama K, et al. Japanese guidelines for the management and treatment of generalized pustular psoriasis: the new pathogenesis and treatment of GPP. J Dermatol. 2018;45(11):1235–70. https://doi.org/10.1111/1346-8138.14523.
Isom J, Braswell DS, Siroy A, Auerbach J, Motaparthi K. Clinical and histopathologic features differentiating acute generalized exanthematous pustulosis and pustular psoriasis: a retrospective series. J Am Acad Dermatol. 2020;83(1):265–7. https://doi.org/10.1016/j.jaad.2020.03.015.
Rakowska A, Jasińska M, Sikora M, et al. Cutaneous T-cell lymphoma in erythrodermic cases may be suspected on the basis of scalp examination with dermoscopy. Sci Rep. 2021;11(1):282. https://doi.org/10.1038/s41598-020-78233-1.
Hoegler KM, John AM, Handler MZ, Schwartz RA. Generalized pustular psoriasis: a review and update on treatment. J Eur Acad Dermatol Venereol. 2018;32(10):1645–51. https://doi.org/10.1111/jdv.14949.
Woods AL, Rutter KJ, Gardner LS, et al. Inpatient management of psoriasis: a multicentre service review to establish national admission standards: inpatient management of psoriasis. Br J Dermatol. 2007;158(2):266–72. https://doi.org/10.1111/j.1365-2133.2007.08338.x.
Navrotski BR de F, Nihi FM, Camilleri MJ, Cerci FB. Wet wrap dressings as a rescue therapy option for erythrodermic psoriasis. An Bras Dermatol. 2018;93(4):598–600. https://doi.org/10.1590/abd1806-4841.20186414.
Nagao K, Ishiko A, Yokoyama T, Tanikawa A, Amagai M. A case of generalized pustular psoriasis treated with topical tacrolimus. Arch Dermatol. 2003;139(9):1219. https://doi.org/10.1001/archderm.139.9.1219-a.
Rodríguez García F, Fagundo González E, Cabrera-Paz R, et al. Generalized pustular psoriasis successfully treated with topical tacrolimus. Br J Dermatol. 2005;152(3):587–8. https://doi.org/10.1111/j.1365-2133.2005.06468.x.
Castela E, Archier E, Devaux S, et al. Topical corticosteroids in plaque psoriasis: a systematic review of efficacy and treatment modalities. J Eur Acad Dermatol Venereol. 2012;26(Suppl 3):36–46. https://doi.org/10.1111/j.1468-3083.2012.04522.x.
Voudouri D, Nikolaou V, Laschos K, et al. Anti-PD1/PDL1 induced psoriasis. Curr Probl Cancer. 2017;41(6):407–12. https://doi.org/10.1016/j.currproblcancer.2017.10.003.
Monsour EP, Pothen J, Balaraman R. A novel approach to the treatment of pembrolizumab-induced psoriasis exacerbation: a case report. Cureus. 2019;11(10): e5824. https://doi.org/10.7759/cureus.5824.
Politi A, Angelos D, Mauri D, Zarkavelis G, Pentheroudakis G. A case report of psoriasis flare following immunotherapy: report of an important entity and literature review. SAGE Open Med Case Rep. 2020;8:2050313X19897707. https://doi.org/10.1177/2050313X19897707.
Umezawa Y, Ozawa A, Kawasima T, et al. Therapeutic guidelines for the treatment of generalized pustular psoriasis (GPP) based on a proposed classification of disease severity. Arch Dermatol Res. 2003;295(Suppl 1):S43-54. https://doi.org/10.1007/s00403-002-0371-6.
Ozawa A, Ohkido M, Haruki Y, et al. Treatments of generalized pustular psoriasis: a multicenter study in Japan. J Dermatol. 1999;26(3):141–9. https://doi.org/10.1111/j.1346-8138.1999.tb03444.x.
Viguier M. Efficacy and safety of tumor necrosis factor inhibitors in acute generalized pustular psoriasis. Arch Dermatol. 2012;148(12):1423. https://doi.org/10.1001/2013.jamadermatol.80.
Torii H, Nakagawa H, Japanese Infliximab Study Investigators. Long-term study of infliximab in Japanese patients with plaque psoriasis, psoriatic arthritis, pustular psoriasis and psoriatic erythroderma. J Dermatol. 2011;38(4):321–334. https://doi.org/10.1111/j.1346-8138.2010.00971.x.
Reynolds KA, Pithadia DJ, Lee EB, Liao W, Wu JJ. A systematic review of treatment strategies for erythrodermic psoriasis. J Dermatol Treat. 2021;32(1):49–55. https://doi.org/10.1080/09546634.2019.1689228.
Studio Italiano Multicentrico nella Psoriasis (SIMPSO). Management of erythrodermic psoriasis with low-dose cyclosporin. Dermatology. 1993;187(1):30–37. https://doi.org/10.1159/000247289.
Charbit L, Mahé E, Phan A, et al. Systemic treatments in childhood psoriasis: a French multicentre study on 154 children. Br J Dermatol. 2016;174(5):1118–21. https://doi.org/10.1111/bjd.14326.
Poulalhon N, Begon E, Lebbé C, et al. A follow-up study in 28 patients treated with infliximab for severe recalcitrant psoriasis: evidence for efficacy and high incidence of biological autoimmunity. Br J Dermatol. 2007;156(2):329–36. https://doi.org/10.1111/j.1365-2133.2006.07639.x.
Viguier M, Pagès C, Aubin F, et al. Efficacy and safety of biologics in erythrodermic psoriasis: a multicentre, retrospective study. Br J Dermatol. 2012;167(2):417–23. https://doi.org/10.1111/j.1365-2133.2012.10940.x.
Robinson A, Van Voorhees AS, Hsu S, et al. Treatment of pustular psoriasis: from the Medical Board of the National Psoriasis Foundation. J Am Acad Dermatol. 2012;67(2):279–88. https://doi.org/10.1016/j.jaad.2011.01.032.
Sandimmune (Cyclosporine) [Package Insert]. Novartis
Remicade (Infliximab) [Package Insert]. Janssen Biotech, Inc.
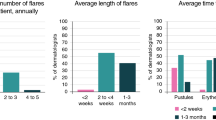
• Yao CJ, Lebwohl MG. Onset of action of antipsoriatic drugs for moderate-to-severe plaque psoriasis: an update. J Drugs Dermatol. 2019;18(3):229–33. (Importance: In this systematic review, Yao and Lebwohl used time to onset of action (TOA) to compare the efficacy rates of multiple biologic and systemic agents.)
• Egeberg A, Andersen YMF, Halling-Overgaard A-S, et al. Systematic review on rapidity of onset of action for interleukin-17 and interleukin-23 inhibitors for psoriasis. J Eur Acad Dermatol Venereol. 2020;34(1):39–46. https://doi.org/10.1111/jdv.15920. (Importance: Built upon the systematic review conducted by Yao and Lebwohl, and compared the efficacy rates between IL-17 and IL-23 inhibitors.)
Imafuku S, Honma M, Okubo Y, et al. Efficacy and safety of secukinumab in patients with generalized pustular psoriasis: a 52-week analysis from phase III open-label multicenter Japanese study. J Dermatol. 2016;43(9):1011–7. https://doi.org/10.1111/1346-8138.13306.
Mateu-Puchades A, Santos-Alarcón S, Martorell-Calatayud A, Pujol-Marco C, Sánchez-Carazo J-L. Erythrodermic psoriasis and secukinumab: our clinical experience. Dermatol Ther. 2018;31(4): e12607. https://doi.org/10.1111/dth.12607.
Mugheddu C, Atzori L, Lappi A, Pau M, Murgia S, Rongioletti F. Successful secukinumab treatment of generalized pustular psoriasis and erythrodermic psoriasis. J Eur Acad Dermatol Venereol. 2017;31(9):e420–1. https://doi.org/10.1111/jdv.14234.
Saeki H, Nakagawa H, Nakajo K, et al. Efficacy and safety of ixekizumab treatment for Japanese patients with moderate to severe plaque psoriasis, erythrodermic psoriasis and generalized pustular psoriasis: results from a 52-week, open-label, phase 3 study (UNCOVER-J). J Dermatol. 2017;44(4):355–62. https://doi.org/10.1111/1346-8138.13622.
Yamasaki K, Nakagawa H, Kubo Y, Ootaki K, Japanese Brodalumab Study Group. Efficacy and safety of brodalumab in patients with generalized pustular psoriasis and psoriatic erythroderma: results from a 52-week, open-label study. Br J Dermatol. 2017;176(3):741–751. https://doi.org/10.1111/bjd.14702.
Sano S, Kubo H, Morishima H, Goto R, Zheng R, Nakagawa H. Guselkumab, a human interleukin-23 monoclonal antibody in Japanese patients with generalized pustular psoriasis and erythrodermic psoriasis: efficacy and safety analyses of a 52-week, phase 3, multicenter, open-label study. J Dermatol. 2018;45(5):529–39. https://doi.org/10.1111/1346-8138.14294.
Zangrilli A, Papoutsaki M, Talamonti M, Chimenti S. Long-term efficacy of adalimumab in generalized pustular psoriasis. J Dermatolog Treat. 2008;19(3):185–7. https://doi.org/10.1080/09546630701759587.
Kimura U, Kinoshita A, Sekigawa I, Takamori K, Suga Y. Successful treatment with adalimumab in a patient with psoriatic arthritis and generalized pustular psoriasis. J Dermatol. 2012;39(12):1071–2. https://doi.org/10.1111/j.1346-8138.2012.01563.x.
Gkalpakiotis S, Arenberger P, Gkalpakioti P, et al. A case of acute generalized pustular psoriasis of von Zumbusch treated with adalimumab. J Eur Acad Dermatol Venereol. 2015;29(10):2063–4. https://doi.org/10.1111/jdv.12597.
Lo Schiavo A, Brancaccio G, Puca RV, Caccavale S. Etanercept in the treatment of generalized annular pustular psoriasis. Ann Dermatol. 2012;24(2):233–4. https://doi.org/10.5021/ad.2012.24.2.233.
Esposito M, Mazzotta A, Casciello C, Chimenti S. Etanercept at different dosages in the treatment of generalized pustular psoriasis: a case series. Dermatology. 2008;216(4):355–60. https://doi.org/10.1159/000117706.
Daudén E, Santiago-et-Sánchez-Mateos D, Sotomayor-López E, García-Díez A. Ustekinumab: effective in a patient with severe recalcitrant generalized pustular psoriasis. Br J Dermatol. 2010;163(6):1346–7. https://doi.org/10.1111/j.1365-2133.2010.09995.x.
Arakawa A, Ruzicka T, Prinz JC. Therapeutic efficacy of interleukin 12/interleukin 23 blockade in generalized pustular psoriasis regardless of IL36RN mutation status. JAMA Dermatol. 2016;152(7):825–8. https://doi.org/10.1001/jamadermatol.2016.0751.
Lee W-K, Kim G-W, Cho H-H, et al. Erythrodermic psoriasis treated with golimumab: a case report. Ann Dermatol. 2015;27(4):446–9. https://doi.org/10.5021/ad.2015.27.4.446.
Krishnamoorthy G, Kotecha A, Pimentel J. Complete resolution of erythrodermic psoriasis with first-line apremilast monotherapy. BMJ Case Rep. 2019;12(1). https://doi.org/10.1136/bcr-2018-226959.
Kumar B, Dhar S, Handa S, Kaur I. Methotrexate in childhood psoriasis. Pediatr Dermatol. 1994;11(3):271–3. https://doi.org/10.1111/j.1525-1470.1994.tb00602.x.
Geiger JM, Czarnetzki BM. Acitretin (Ro 10–1670, etretin): overall evaluation of clinical studies. Dermatologica. 1988;176(4):182–90. https://doi.org/10.1159/000248701.
Pescitelli L, Dini V, Gisondi P, et al. Erythrodermic psoriasis treated with ustekinumab: an Italian multicenter retrospective analysis. J Dermatol Sci. 2015;78(2):149–51. https://doi.org/10.1016/j.jdermsci.2015.01.005.
Marrakchi S, Guigue P, Renshaw BR, et al. Interleukin-36-receptor antagonist deficiency and generalized pustular psoriasis. N Engl J Med. 2011;365(7):620–8. https://doi.org/10.1056/NEJMoa1013068.
Johnston A, Xing X, Wolterink L, et al. IL-1 and IL-36 are dominant cytokines in generalized pustular psoriasis. J Allergy Clin Immunol. 2017;140(1):109–20. https://doi.org/10.1016/j.jaci.2016.08.056.
Bachelez H, Choon S-E, Marrakchi S, et al. Inhibition of the interleukin-36 pathway for the treatment of generalized pustular psoriasis. N Engl J Med. 2019;380(10):981–3. https://doi.org/10.1056/NEJMc1811317.
Judith Stewart. Enbrel FDA Approval History. https://www.drugs.com/history/enbrel.html,
Infliximab FDA Approval History. Drugs.com. https://www.drugs.com/history/remicade.html#:~:text=Remicade%20FDA%20Approval%20History&text=Remicade%20(infliximab)%20is%20a%20tumor,psoriatic%20arthritis%20and%20plaque%20psoriasis.
Humira FDA Approval History. Drugs.com. https://www.drugs.com/history/humira.html
Lingala B, Li S, Wysong A, Truong AK, Kim D, Chang ALS. Low rate of dermatology outpatient visits in Asian-Americans: an initial survey study for associated patient-related factors. BMC Dermatol. 2014;14(1):13. https://doi.org/10.1186/1471-5945-14-13.
Kerr GS, Qaiyumi S, Richards J, et al. Psoriasis and psoriatic arthritis in African-American patients–the need to measure disease burden. Clin Rheumatol. 2015;34(10):1753–9. https://doi.org/10.1007/s10067-014-2763-3.
Takeshita J, Gelfand JM, Li P, et al. Psoriasis in the US Medicare population: prevalence, treatment, and factors associated with biologic use. J Invest Dermatol. 2015;135(12):2955–63. https://doi.org/10.1038/jid.2015.296.
Takeshita J, Eriksen WT, Raziano VT, et al. Racial differences in perceptions of psoriasis therapies: implications for racial disparities in psoriasis treatment. J Investig Dermatol. 2019;139(8):1672-1679.e1. https://doi.org/10.1016/j.jid.2018.12.032.
Orenstein LAV, Nelson MM, Wolner Z, et al. Differences in outpatient dermatology encounter work relative value units and net payments by patient race, sex, and age. JAMA Dermatol. 2021;157(4):406. https://doi.org/10.1001/jamadermatol.2020.5823.
Resneck JS, Isenstein A, Kimball AB. Few Medicaid and uninsured patients are accessing dermatologists. J Am Acad Dermatol. 2006;55(6):1084–8. https://doi.org/10.1016/j.jaad.2006.07.012.
Mulcahy A, Mehrotra A, Edison K, Uscher-Pines L. Variation in dermatologist visits by sociodemographic characteristics. J Am Acad Dermatol. 2017;76(5):918–24. https://doi.org/10.1016/j.jaad.2016.10.045.
Stephen E. Wolverton and Jashin J. Wu. Comprehensive dermatologic drug therapy Fourth Edition: Elsevier; 2019.
Cosentyx (Secukinumab) [Package Insert]. Novartis Pharmaceuticals Corporation.
Taltz (Ixekizumab) [Package Insert]. Eli Lilly and Company.
Siliq (Brodalumab) [Package Insert]. Valeant Pharmaceuticals.
Tremfya (Guselkumab) [Package Insert]. Janssen Biotech, Inc.
Terui T, Kobayashi S, Okubo Y, Murakami M, Hirose K, Kubo H. Efficacy and safety of guselkumab, an anti-interleukin 23 monoclonal antibody, for palmoplantar pustulosis: a randomized clinical trial. JAMA Dermatol. 2018;154(3):309–16. https://doi.org/10.1001/jamadermatol.2017.5937.
Soriatane (Acitretin) [Package Insert]. Stiefel Laboratories, Inc.
Vun YY, Jones B, Al-Mudhaffer M, Egan C. Generalized pustular psoriasis of pregnancy treated with narrowband UVB and topical steroids. J Am Acad Dermatol. 2006;54(2 Suppl):S28-30. https://doi.org/10.1016/j.jaad.2005.04.041.
Stelara (Ustekinumab) [Package Insert]. Janssen Biotech, Inc.
Arbiser JL, Grossman K, Kaye E, Arndt KA. Use of short-course class 1 topical glucocorticoid under occlusion for the rapid control of erythrodermic psoriasis. Arch Dermatol. 1994;130(6):704–6.
Raimer SS. Occlusion of potent topical steroids. Arch Dermatol. 1995;131(2):227. https://doi.org/10.1001/archderm.1995.01690140113024.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Shinkai has nothing to disclose. Dr. Bhutani is currently an investigator for studies being sponsored by AbbVie. She has served as an advisor for Boehringer Ingelheim, Janssen, Lilly, Novartis, Sun, and UCB. Dr. Wilson Liao has received research grant funding from AbbVie, Amgen, Janssen, Leo, Novartis, Pfizer, Regeneron, and TRex Bio. Edward Hadeler, Megan Mosca, Julie Hong, and Dr. Nicholas Brownstone have nothing to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This paper has not been previously published or posted and is not under consideration elsewhere.
This article is part of the Topical Collection on Hospital-based Dermatology
Rights and permissions
About this article
Cite this article
Hadeler, E., Mosca, M., Hong, J. et al. Inpatient Management of Psoriasis: A Current Perspective and Update for Clinicians. Curr Derm Rep 10, 205–221 (2021). https://doi.org/10.1007/s13671-021-00342-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13671-021-00342-5