Abstract
Purpose of Review
This review will outline seminal and contemporary balance and gait measures most commonly used with geriatric clients, along with the administration procedures, clinical utility, and psychometric qualities that support their use.
Recent Findings
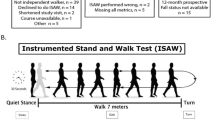
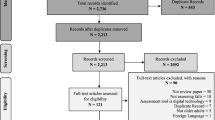
Ten balance and five gait performance tests were reviewed. Balance instruments range from the simple to the complex. These tools quantify older adults’ ability to maintain postural stability during tasks that manipulate sensory conditions and functional activities, and challenge their base of support. Gait assessment is common in geriatric rehabilitation. Frail clients who ambulate with an assistive device can benefit from a more basic locomotion test, whereas seniors at higher mobility levels should be challenged with tasks superimposed on the gait sequence. Recent adaptations of traditional tests include surface changes, technology application, and clinical utility with subsets of older adults such as those with lumbar surgery and postural tremor. Timed floor rise ability more thoroughly addresses the fall risk dimension.
Summary
Balance and gait assessments quantify physical performance in older adults and are utilized to establish interventions to improve mobility, reduce fall risk, and increase balance confidence. A wide variety of outcome measures exists in geriatric rehabilitation, though tests should be tapered for the functional level of the client. Practitioners should consider test administration for older adults with atypical diagnoses, along with flooring changes, technology adaptation, and timed supine to stand ability. Future research should revisit commonly accepted threshold scores for fall risk.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Karinkanta S, Heinonen A, Sievanen H, Uusi-Rasi K, Kannus P. Factors predicting dynamic balance and quality of life in home-dwelling elderly women. Gerontol. 2005;51(2):116–21. https://doi.org/10.1159/000082196.
Schaap LA, Koster A, Visser M. Adiposity, muscle mass, and muscle strength in relation to functional decline in older persons. Epidemiol Rev. 2013;35(1):51–65. https://doi.org/10.1093/epirev/mxs006.
•• Gouveia ER, Ihle A, Gouveia BR, Kliegel M, Marques A, Freitas DL. Muscle mass and muscle strength relationships to balance: the role of age and physical activity. J Aging Phys Act. 2019:1–7. https://doi.org/10.1123/japa.2018-0113This cross-sectional study analyzed the relationship between balance ability and both muscle and muscle strength among 802 older adult volunteers. There was a positive correlation between both variable domains and balance ability using the Fullerton Advanced Balance Scale.
Carty CP, Cronin NJ, Nicholson D, et al. Reactive stepping behaviour in response to forward loss of balance predicts future falls in community-dwelling older adults. Age Ageing. 2015;44(1):109–15. https://doi.org/10.1093/ageing/afu054.
• Selbach NM, O’Brian K, Brooks D, et al. Speed and distance requirements for community ambulation: a systematic review. Arch Phys Med Rehabil. 2014;95:117–28 The systematic review outlines from seven studies distance requirements needed to navigate community locations such as stores, warehouses, and cemeteries. Twenty-four US sites were identified in the review; moreover, speeds required to traverse a street with traffic light changes varied greatly between locations.
Fritz S, Lusardi M. Walking speed: the sixth vital sign. J Geriatr Phys Ther. 2009;32(2):46–9.
Duncan PW, Studenski S, Chandler J, Prescott B. Functional reach: predictive validity in a sample of elderly male veterans. J Gerontol. 1992;47(3):M93–8.
Berg K, Wood-Dauphine SL, Williams JI, Maki B. Measuring balance in the elderly: validation of an instrument. Can J Pub Health. 1992;83:S9–11.
Newton RA. Validity of the multidirectional reach test: a practical measure for limits of stability in older adults. J Gerontol: Med Sci. 2001;56A(4):M248–52.
Newton RA. Balance screening of an inner city older adult population. Arch Phys Med Rehabil. 1997;78:587–91.
Steffen TM, Mollinger LA. Age- and gender-related test performance in community-dwelling adults. J Neurol Phys Ther. 2005;29(4):181–8. https://doi.org/10.1097/01.NPT.0000282315.17359.95.
Tinetti M. Performance-oriented assessment of mobility programs in elderly patients. J Am Geriatr Soc. 1985;34:119–26.
Cipriany-Dacko LM, Innerst D, Johannsen J, Rude V. Interrater reliability of the Tinetti balance scores in novice and experienced physical therapy clinicians. Arch Phys Med Rehabil. 1997;78:1160–4.
Knobe M, Giesen M, Plate S, Gradl-Dietsch G, Buecking B, Eschbach D, et al. The Aachen Mobility and Balance Index to measure physiological falls risk: a comparison with the Tinetti POMA Scale. Eur J Trauma Emerg Surg. 2016;42:537–45. https://doi.org/10.1007/s00068-016-0693-2.
Rivolta MW, Aktaruzzaman M, Rizzo G, Lafortuna CL, Ferrarin M, Bovi G, et al. Evaluation of the tinetti score and fall risk assessment via accelerometry-based movement analysis. Artif Intell Med. 2019;95:38–47.
Bogle-Thorbahn LD, Newton RA. Use of the Berg Balance Test to predict falls in elderly person. Phys Ther. 1997;76(6):576–83.
Shumway-Cook A, Baldwin M, Pollisar N, Gruber W. Predicting the probability of falls in community-dwelling adults. Phys Ther. 1997;77:812–9.
Riddle DL, Stratford PW. Interpreting indexes for diagnostic tests: an illustration using the Berg Balance Test. Phys Ther. 1999;79(10):939–48.
Muir SW, Berg K, Chesworth B, Speechley M. Use of the Berg Balance Scale for predicting multiple falls in community-dwelling elderly people: a prospective study. Phys Ther. 2008;88(4):449–59.
Conradsson M, Lundin-Olsson L, Lindelöf N, Littbrand H, Malmqvist L, Gustafson Y, et al. Berg Balance Scale: intrarater test-retest reliability among older people dependent in activities of daily living and living in residential care facilities. Phys Ther. 2007;87(9):1155–63. https://doi.org/10.2522/ptj.20060343.
Dite W, Temple VA. A clinical test of stepping and change of direction to identify multiple falling older adults. Arch Phys Med Rehabil. 2002;83(11):1566–7.
Batting M, Barker KL. Reliability and validity of the Four Square Step Test in patients with hip osteoarthritis before and after total hip replacement. Physiother. 2019 Jun;105(2):244–53. https://doi.org/10.1016/j.physio.2018.07.014.
Mathurapongsakul P, Siriphorn A. Four Square Step Test with foam is more accurate than those without foam for discriminating between older adults with and without fall history. J Aging Phys Act. 2018;26(4):624–8. https://doi.org/10.1123/japa.2017-0363.
Rose DJ, Lucchese N, Wiersma LD. Development of a multidimensional balance scale for use with functionally independent older adults. Arch Phys Med Rehabil. 2006;87:1478–85.
Klein PJ, Fiedler RC, Rose DJ. Rasch analysis of the Fullerton Advanced Balance Scale. Physiother Can. 2011;63(1):115–25. https://doi.org/10.3138/ptc.2009-51.
Klima D, Morgan L, Baylor M, Reilly C, Gladmon D, Davey A. Physical performance and fall risk in persons with traumatic brain injury. Percept Motor Skills. 2019;126(1):50–69. https://doi.org/10.1177/0031512518809203.
Schlenstedt C, Brombacher S, Hartwigsen G, Weisser B, Möller B, Deuschl G. A comparison of the Fullerton Advanced Balance Scale, Mini-BESTest, and Berg Balance Scale to predict falls in Parkinson disease. Phys Ther. 2016;96(4):494–501.
Horak FB, Wrisley DM, Frank J. The Balance Evaluation Systems Test (BESTest) to differentiate balance deficits. Phys Ther. 2009;89(5):484–98. https://doi.org/10.2522/ptj.20080071.
Jácome C, Cruz J, Oliveira A, Marques A. Validity, reliability, and ability to identify fall status of the Berg Balance Scale, BESTest, Mini-BESTest, and Brief-BESTest in patients with COPD. Phys Ther. 2016;96(11):1807–15. https://doi.org/10.2522/ptj.20150391.
Godi M, Franchignoni F, Caligari M, Giordano A, Turcato AM, Nardone A. Comparison of reliability, validity, and responsiveness of the mini-BESTest and Berg Balance Scale in patients with balance disorders. Phys Ther. 2013;93(2):158–67. https://doi.org/10.2522/ptj.20120171.
Yingyongyudha A, Saengsirisuwan V, Panichaporn W, Boonsinsukh R. The Mini-Balance Evaluation Systems Test (Mini-BESTest) demonstrates higher accuracy in identifying older adult participants with history of falls than do the BESTest, Berg Balance Scale, or Timed Up and Go Test. J Geriatr Phys Ther. 2016;39(2):64–70. https://doi.org/10.1519/JPT.0000000000000050.
• Klima DW, Anderson C, Samrah D, Patel D, Chui K, Newton R. Standing from the floor in community-dwelling older adults. J Aging Phys Act. 2016;24(2):207–13. https://doi.org/10.1123/japa.2015-0081The study analyzes in older adults, both quantitatively and qualitatively, the supine to stand maneuver and relevant performance correlate. Findings demonstrate that floor rise ability is significantly related to age, grip strength, balance confidence, and physical performance variables.
Ulbrich J, Raheja A, Alexander NB. Body positions used by healthy and frail older adults to rise from the floor. J Geriatr Soc. 2000;48:1626–32.
Bohannon RM, Lusardi MM. Getting up from the floor. Determinants and techniques among healthy older adults. Physiother Theory Prac. 2004;20:233–41.
Bloch F. Critical falls: why remaining on the ground after a fall can be dangerous, whatever the fall. J Geriatr Soc. 2012;60:1375–6.
Brito LB, Ricardo DR, Araujo DS, Ramos PS, Myers J, Araujo CG. Ability to sit and rise from the floor as a predictor of all-cause mortality. Eur J Prev Cardiol. 2013;21:892–8.
Legters K. Fear of falling. Phys Ther. 2002;82:264–72.
Maki BE, Holiday PJ, Topper AK. Fear of falling and postural performance in the elderly. J Gerontol. 1991;46:M123–31.
Tinetti ME, Rickman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol B Psych Soc Sci. 1990;45:P239–43.
Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol A Biol Med Sci. 1995;50A:M28–34.
Myers AM, Fletcher PC, Myers AH, Sherk W. Discriminative and evaluative properties of the Activities-specific Balance Confidence (ABC) Scale. J Gerontol Med Sci. 1998;53A(4):M287–94.
Lajoie Y, Girard A, Guay M. Comparison of the reaction time, the Berg Scale, and the ABC in non fallers and fallers. Arch Gerontol Geriatr. 2002;35:215–23.
Peters DM, Fritz SL, Krotish DE. Assessing the reliability and validity of a shorter walk test compared with the 10-meter walk test for measurements of gait speed in healthy, older adults. J Geriatr Phys Ther. 2013;36(1):24–30.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol Med Sci. 2001;56A3:M146–56.
Chui K, Hood E, Klima DW. Meaningful change in walking speed. Topics Geriatr Rehabil. 2012;28:97–103.
Bohannon RW. Comfortable and maximum walking speed of adults aged 20-79 years: reference values and determinants. Age Ageing. 1997;26:15–9.
Podsiadlo D, Richardson S. The Timed “Up and Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–7.
Bohannon RW. Reference values for the Timed Up and Go Test: a descriptive meta-analysis. J Geriatr Phys Ther. 2006;292:64–8.
Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the timed up & go test. Phys Ther. 2000;80(9):896–903.
• Casey CM, Parker EM, Winkler G, Liu X, Lambert GH, Eckstrom E. Lessons learned from implementing CDC’s STEADI falls prevention algorithm in primary care. Gerontol. 2017;57(4):787–96 This descriptive study depicts how the Center for Disease Control’s STEADI initiatives were implemented in an internal medicine clinic to screen for fall risk. The authors describe key implementation strategies using Kotter framework underpinnings to facilitate clinical practice.
Kristensen MT, Foss NB, Kehlet H. Timed “Up and Go” Test as a predictor of falls within six months after hip fracture surgery. Phys Ther. 2007;871:24–30.
Chiu YP, Fritz SL, Light KE, Velozo CA. Use of item response analysis to investigate measurement properties and clinical validity of data for the Dynamic Gait Index. Phys Ther. 2006;86(6):778–87.
Wrisley DM, Walker ML, Echternach JL, Strasnick B. Reliability of the dynamic gait index in people with vestibular disorders. Arch Phys Med Rehabil. 2003;84(10):1528–33.
Whitney S, Wrisley D, Furman J. Concurrent validity of the Berg Balance Scale and Dynamic Gait Index in people with vestibular dysfunction. Physiother Res. 2003;8(4):178–86.
Herman T, Inbar-Borovsky N, Brozgol M, Giladi N, Hausdorff JM. The Dynamic Gait Index in healthy older adults: the role of stair climbing, fear of falling, and gender. Gait Posture. 2009;29:237–41.
Sittichoke C, Buasord J, Boripuntakul S, Sungkarat S. Effects of compliant flooring on dynamic balance and gait characteristics of community-dwelling older persons. J Nutr Health Aging. 2019;23(7):665–8. https://doi.org/10.1007/s12603-019-1211-0.
Wrisley DM, Marchetti GF, Kuharsky DK, Whitney SL. Reliability, internal consistency, and validity of data obtained with the functional gait assessment. Phys Ther. 2004;84(10):906–18.
Wrisley DM, Kumar NA. Functional gait assessment: concurrent, discriminative, and predictive validity in community-dwelling older adults. Phys Ther. 2010;90(5):761–73. https://doi.org/10.2522/ptj.20090069.
Rasekaba T, Lee AL, Naughton MT, Williams TJ, Holland AE. The six-minute walk test: a useful metric for the cardiopulmonary patient. Intern Med J. 2009;39:495–501.
Keeratichananont W, Thanadetsuntorn C, Keeratichananont S. Value of preoperative 6-minute walk test for predicting postoperative pulmonary complications. Ther Adv Respir Dis. 2016;10(1):18–25.
Parry SM, Nalamalapu SR, Nunna K, Rabiee A, Friedman LA, Colantuoni E, et al. Six-minute walk distance after critical illness: a systematic review and meta-analysis. J Intensive Care Med. 2019:1–9. https://doi.org/10.1177/0885066619885838.
Bohannon RW, Crouch R. Minimal clinically important difference for change in 6-minute walk test distance of adults with pathology: a systematic review. J Eval Clin Pract. 2017;23:377–81.
Harada ND, Chiu V, Stewart AL. Mobility-related function in older adults: assessment with a 6-minute walk test. Arch Phys Med Rehabil. 1999;80:837–41.
Crapo RO, Casaburi R, Coates AL, et al. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–7.
Steffen TM, Hacker TA, Mollinger L. Age and gender-related test performance in community-dwelling elderly people: six-minute walk test, berg balance scale, timed up & go test, and gait speeds. Phys Ther. 2002;82(2):128–36.
Mohanan H, Kutty RK, Kamaraj B. Impact of six minute walk distance with quality of life in geriatrics population. Int J Appl Res. 2018;4(6):37–47.
Chuang CY, Lin SY, Li MH, Chang YJ, Hsu MJ. Six-minute walk test in community-dwelling older adults. Topics Geri Rehabil. 2019;35(4):266–72.
Chui KK, Lusardi MM. Spatial and temporal parameters of self-selected and fast walking speeds in healthy community-living adults aged 72–98 years. J Geriatr Phys Ther. 2010;33(4):173–83.
Ghislieri M, Gastaldi L, Pastorelli S, Tadano S, Agostini V. Wearable inertial sensors to assess standing balance: a systematic review. Sensors. 2019;19(19):4075. https://doi.org/10.3390/s19194075.
Sheehan KJ, Greene BR, Cunningham C, Crosby L, Kenny RA. Early identification of declining balance in higher functioning older adults: an inertial sensor based method. Gait Posture. 2014 Apr;39(4):1034–9. https://doi.org/10.1016/j.gaitpost.2014.01.003.
Van Diest M, Lamoth CJ, Stegenga J, Verkerke GJ, Postema K. Exergaming for balance training of elderly: state of the art and future developments. J Neuroeng Rehab. 2013;10(1):101. https://doi.org/10.1186/1743-0003-10-101.
Wallmann HW. Comparison of elderly nonfallers and fallers on performance measures of functional reach, sensory organization, and limits of stability. J Gerontol A Biol Sci. 2001;56(9):M580–3.
Loughran S, Tennant N, Kishore A, Swan IR. Interobserver reliability in evaluation stability between clinicians and posturography. Clin Otolaryngol. 2005;30(3):255–7.
Sparto PJ, Newman AB, Simonsick EM, et al. Contributions to lateral balance control in ambulatory older adults. Aging Clin Exp Res. 2018;30(6):633–41. https://doi.org/10.1007/s40520-017-0819-3.
Levin I, Lewek MD, Giuliani C, Faldowski R, Thorpe DE. Test-retest reliability and minimal detectable change for measures of balance and gait in adults with cerebral palsy. Gait Posture. 2019;72:96–101.
Lubetzky AV, Soroka A, Harel D, Errico T, Bendo J, Leitner J, et al. Static and dynamic balance in adults undergoing lumbar spine surgery. J Am Acad Orthop Surg. 2019;1:e553–9. https://doi.org/10.5435/jaaos-d-19-00113.
Xu X, Chen J, Chen M, Gu Z, Ji S, Liu S, et al. Postural tremor is associated with gait and balance impairments in community-dwelling older people. J Am Geriatr Soc. 2019;67(4):799–803.
Gray VL, Goldberg AP, Rogers MW, Anthony L, Terrin ML, Guralnik JM, et al. Asymptomatic carotid stenosis is associated with mobility and cognitive dysfunction and heightens falls in older adults. J Vasc Surg. 2019:1937. https://doi.org/10.1016/j.jvs.2019.09.020.
Schoene D, Wu SM, Mikolaizak AS, et al. Discriminative ability and predictive validity of the timed up and go test in identifying older people who fall: systematic review and meta-analysis. J Am Geriatr Soc. 2013;61(2):202–8.
Tinetti ME, Kumar C. The patient who falls: “It's always a trade-off”. JAMA. 2010;303(3):258–266. https://doi.org/10.1001/jama.2009.2024
Resources
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Physical Therapy and Rehabilitation
Rights and permissions
About this article
Cite this article
Klima, D.W., Hood, E. Gait and Balance Assessment of Older Adults. Curr Geri Rep 9, 154–162 (2020). https://doi.org/10.1007/s13670-020-00327-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13670-020-00327-5