Abstract
The purpose of this review is to highlight existing literature on the epidemiology, pathophysiology, and novel risk factors for vascular dementia. We further examine the evidence linking chronic brain hypoperfusion induced by a variety of cardiovascular diseases to the development of vascular dementia. In the elderly, in whom cerebral perfusion is diminished by the aging process, additional reduction in cerebral blood flow stemming from exposure to potentially modifiable vascular risk factors increases the probability of developing vascular dementia. Finally, we discuss the association between obstructive sleep apnea, an underrecognized risk factor for stroke, and vascular dementia. Obstructive sleep apnea is linked to cerebrovascular disease through many intermediary vascular risk factors and may directly cause cerebrovascular damage through microvacular disease. Insight into how cardiovascular risk factors induce vascular dementia offers an enhanced understanding of the multifactorial pathophysiology by this disorder and ways of preventing and managing the cerebrovascular precursors of vascular dementia. Many vital questions about the relation of obstructive sleep apnea with stroke and vascular dementia are still unanswered and await future well-designed studies.
Similar content being viewed by others
Introduction
Cognitive impairment and dementia are disabling conditions expected to rise in prevalence with the rapidly aging population [1, 2].Dementia implies a decrease in cognitive abilities leading to functional decline and the inability to carry out usual activities of a cognitively healthy person [3].Stroke remains the number one cause of disability and the third leading cause of death in the USA. Evidence continues to accumulate on the cerebrovascular contribution to incident and prevalent dementia [4].Vascular dementia was initially described in the nineteenth century after dementia developed in patients with recurrent strokes (multi-infarct dementia) or with severe white matter disease associated with long standing hypertension (i.e., Binswanger disease) and was commonly thought to be the primary cause of dementia in the elderly—so called “hardening of the arteries [5].”However, in the second half of the twentieth century, neuropathological studies showed that the pathological hallmarks of Alzheimer disease, as opposed to cerebrovascular damage, are more common in patients with dementia [6].This resulted in a paradigm shift such that most late-onset dementia was thought to be due to Alzheimer disease, and criteria for dementia developed during this period reflect this bias: memory loss became a required component. However, the advent of newer neuroimaging techniques, such as computed tomography and magnetic resonance imaging, demonstrated that vascular damage in the brain was very prevalent. Sub-clinical brain infarcts (SBI) were seen in 17 % of participants from the Northern Manhattan Study [7] and white matter lesions by MRI in up to 90 % of participants of the Rotterdam Study [8].At the same time, associational studies have consistently found that vascular damage contributes to a large proportion of late-onset dementia cases, so much so that “mixed disease”—that is, Alzheimer pathology and cerebrovascular damage—may even be the most common pathological finding in dementia cases. In autopsy series, vascular pathology was found in up to 50 % of those with pathologic Alzheimer’s disease (AD) and approximately one-third of patients diagnosed with vascular dementia will have AD pathology at autopsy [9].
Definition of Vascular Dementia
Vascular dementia is better understood as a heterogeneous syndrome in which the underlying etiology is cerebrovascular disease manifesting as dementia [3, 10].The syndrome should be characterized by evidence of clinical stroke or subclinical vascular brain injury affecting at least two cognitive domains and causing sufficient decline to affect the activities of daily living [3, 11].Progression of vascular dementia can occur as a “step-wise” process or as a continuous decline. Because vascular dementia and Alzheimer disease commonly coexist, they are difficult to differentiate; nonetheless, in the case of subcortical vascular dementia, the clinical presentation is characterized by a subcortical syndrome with signs such as executive dysfunction, psychomotor slowness, pseudobulbar palsy and gait instability. In cases of vascular dementia involving cortical lesions, signs such as dysphasia, dyspraxia, and neglect can be also present [3].
A common misconception about the phenotype of vascular dementia is the expected degree of “memory” impairment. While it is true that patients with Alzheimer disease often presents primarily with an amnestic syndrome, it is important to recognize that the term “memory” is an umbrella term that includes a number of different abilities that can be variably impaired, rather than a single ability. Since damage to different brain areas is variable in cerebrovascular disease, so can memory disturbances vary or be nonexistent. This is less true in Alzheimer pathology, since damage generally spreads from medial temporal lobe structures to other areas, and thus amnestic disorders are more common. In addition, memory disturbance may be relatively mild and/or occur later in vascular dementia.
Neuropsychiatric symptoms such as depression [12] and delirium can be seen dementia, but their role as a risk factor for cognitive decline is controversial [13].In a recent study of patients that underwent cardiac surgery, those that developed post-operative delirium were more likely to have lower mini-mental scores (MMSE) at baseline, 25.8 (delirium) vs. 26.9 (no delirium), p < 0.001. In addition, those with delirium had a larger drop in the MMSE two days after surgery [14].Compared to those without delirium, a greater percentage of patients with delirium did not return to preoperative baseline performance at six months (40 % vs. 24 %, p = 0.01).
Epidemiology of Vascular Dementia
The overall prevalence of dementia in developed countries is 5–10 % in people older than 65 years of age, but this increases rapidly by decade with a prevalence of as much as 50 % of the population over age 85 [3, 10].Vascular dementia is the second leading cause of dementia, without taking into account mixed dementia, and its prevalence is expected to double every five years after age 65 [15].A number of studies have demonstrated an especially high incidence of cognitive impairment and dementia after stroke with rates as high as 30 %. In a recent study of 300 patients with mild strokes, screening tests such as the MMSE were predictive of moderate to severe vascular cognitive impairment, defined by deficits in ≥ 3 cognitive domains neuropsychological testing, 3–6 months after stroke [16].An analysis of the Secondary Prevention of Small Subcortical Strokes (SPS3) trial showed that mild cognitive impairment, defined as z score −1.5 in at least one cognitive domain from either an amnestic or non-amnestic test was present in nearly half of patients with lacunar strokes [17].
Pathophysiology
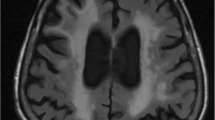
Vascular dementia can be caused by atherosclerosis of the cerebral arteries, cerebral small vessel disease, and chronic subcortical ischemia occurring in the distribution of penetrating arteries of the periventricular white matter [18].Atherosclerotic plaques develop in large to medium size arteries, but can also be present in small penetrating vessels in the form of microatheroma. Plaque rupture causes stroke through local thrombosis or atheromatous thrombi leading to ischemia. The small artery damage underlying lacunar infarctions and ischemic white matter lesions is most commonly found in association with lipohyalinosis affecting the small penetrating arteries [15].
Cerebral small vessel disease is more prevalent in the elderly and in those with hypertension and/or diabetes [19].Cerebral microbleeds [20] and retinal microvascular changes [21] are commonly seen in those with dementia. Cross-sectional studies have observed associations between retinal microvascular changes and dementia (that ranges from OR 1.17 to 5.57). Pathological studies show that ischemic white matter disease consists of demyelination, loss of axons, gliosis, widening of perivascular spaces and loss of blood–brain-barrier integrity [15].Patients with advanced Alzheimer disease can have white matter lesions on MRI. Many studies have focused on vascular causes of these changes, implying an interaction between Alzheimer’s and vascular pathology, but Wallerian degeneration due to degeneration of cortical inputs remains a plausible alternative. Unfortunately, imaging studies cannot differentiate the underlying pathophysiology of white matter lesions and pathological studies are limited. However, the presence of SBI, white matter lesions, microbleeds, and brain atrophy has been linked to aging and vascular risk factors, especially hypertension. The Framingham offspring studies reported that increases in systolic blood pressure among young adults was associated with early structural changes of subcortical structures in the anterior corpus callosum, the inferior fronto-occipital fasciculi and with reduced grey-matter volumes in the middle temporal gyrus [22].In addition, the number and volume of white matter lesions was a predictor of vascular dementia. Clinical–imaging correlations have suggested that larger volumes and greater numbers of brain lesions are associated with a greater risk of vascular dementia [23, 24].The cardiovascular risk factors associated with vascular dementia may disturb hemodynamic flow and thereby induce cerebral hypoperfusion and subsequent disruption of the cortical-subcortical circuitry and microstructural integrity [25].
Advances in Neuroimaging Studies
Neuroimaging studies have provided estimates of the amount of chronic and progressive brain ischemic injury and their effects on cognitive function [13].Brain ischemic changes (e.g., white matter lesions) are associated with stroke, cognitive decline, dementia and death [26, 27].Degenerative and vascular disease often coexists and contributes to white matter disease and cognitive impairment. For example, in a group of 54 normal elderly (mean age 77 years), measures of cognitive performance correlated with cerebrovascular white matter disease on MRI and amyloid imaging by positron emission tomography [28].The authors did not observe an association between measures of cerebrovascular disease and amyloid using Pittsburgh Compound B-positron emission tomography. Compared to participants with positive amyloid, those with white matter disease had worse executive function, while amyloid did not affect cognition in that healthy cohort. In the study, early cognitive changes were mainly associated with cerebrovascular disease and not amyloid. Another study of patients > 70 years of age with extensive white matter hyperintensities (WMH) by MRI, found that approximately 70 % with WMH had no evidence of amyloid [29].The authors noted that participants with negative amyloid were younger, with a greater number of lacunar infarctions, presumably from small vessel disease, and these patients performed better on delayed recall tasks (verbal and visual memory) when compared to those with positive amyloid by PET scan.
Neuroimaging data suggest that progression of brain atrophy contributes to vascular dementia. For example, the Leukoaraiosis and Disability Study (LADIS) evaluated the association of medial temporal lobe atrophy, cortical and subcortical atrophy, and white matter lesion volume prospectively on cognitive decline. After three years of follow-up, medial temporal lobe atrophy and subcortical atrophy predicted a decline in global cognition, psychomotor speed, executive function, and memory [30]. There was also a significant synergistic interaction between white matter lesion volume and atrophy, with an increased rate of cognitive decline. Similar findings were observed by the SMART-MR Study (Second Manifestations of Arterial Disease-Magnetic Resonance), [31] that followed 565 patients > 60 years of age with symptomatic atherosclerotic disease but without large infarcts. After a mean follow up of four years, periventricular white matter lesion volume at baseline, and its progression, was associated with a greater decrease in cortical gray matter volume and an increase in ventricular volume independent of vascular risk factors.
In summary, recent functional neuroimaging studies suggest that early cerebrovascular damage may cause early cognitive dysfunction. In addition, the coexistence of vascular disease and amyloid is complex and the interaction between these factors in causing dementia and brain atrophy warrants further research.
Prevention of Vascular Dementia
Existing evidence suggests that exposure to risk factors in midlife leads to cumulative vascular and neuronal damage contributing to vascular dementia in late life. It is not surprising that epidemiological studies find evidence of modifiable vascular risk factors such as mid-life hypertension, associated with progression of cognitive impairment at 14, 25, and 30 years [32].In the Heart Outcomes Prevention Evaluation (HOPE) study, the effect of the angiotensin-converting enzyme inhibitor (ACE-I) ramipril was compared against placebo in 1013 high-risk patients with a history of stroke or transient ischemic attack (TIA). The HOPE study observed a 59 % relative risk reduction of cognitive decline for those assigned to the ramipril arm [33, 34].
Treatment of high cholesterol [35] and physical inactivity [36] could also prevent the development or progression of dementia. A prospective analysis of the Leukoaraiosis and Disability (LADIS) study composed of 639 subjects with a mean age of 74 years, showed that physical activity protected against vascular dementia (HR 0.42; 95 %CI, 0.22-0.80), independent of age, education, white matter change severity, previous and incident stroke and DM [37].
Randomized controlled trials modifying hypertension and other vascular risk factors (e.g., dyslipidemia) are needed to address the primary prevention of dementia. A series of ongoing trials have been designed to address these limitations, including the Systolic Pressure Intervention Trial (SPRINT) that is currently examining intensive blood pressure lowering compared to standard of care, in relation cognitive function by an extensive neuropsychological battery [38, 39].Another understudied but potentially important set of risk factors for vascular dementia is the metabolic syndrome, a cluster of cardiovascular risk factors that include obesity, hypertension, insulin resistance, and dyslipidemia [10].The metabolic syndrome was strongly associated with incident vascular dementia in a population-based cohort study (HR = 3.7) [40].In addition, patients with metabolic syndrome have early white matter changes by diffusor tensor imaging [41].In the Northern Manhattan study, those with metabolic syndrome had worse mini-mental scores, defined by a score < 18, (OR = 1.94; 95 % CI 1.26, 3.01) compared to those without metabolic syndrome [42].
Vascular Risk factors, Cardiac Disease and Cerebral Hypoperfusion
Chronic brain hypoperfusion and its consequential neural hypometabolism can accelerate the onset of cognitive symptoms and abnormal neuropathology [25].The main risk factor associated with chronic brain hypoperfusion is hypertension. Chronic hypertension causes pulsatile pressure changes and increased microvascular resistance that may lead to brain hypoperfusion [43, 44].Additionally, longstanding hypertension impairs vasomotor reactivity and shifts the cerebral autoregulation curve towards higher blood pressures [25].Reducing blood pressure later in life may result in an increased risk of stroke by further impairing adequate cerebral perfusion [45, 46].
Cardiac disease such as left ventricular heart failure and atrial fibrillation may also lead to chronic cerebral hypoperfusion and vascular dementia [25].Low ejection fraction or low cardiac output has been associated with impairments in attention and executive function [47].
Cerebral hemodynamics measured by transcranial Doppler ultrasound (TCD) may serve as an early surrogate of cerebrovascular compromise [48, 49].Transcranial Doppler ultrasound is a safe, noninvasive technique widely used in clinical practice, which enables measurement of cerebral hemodynamics in the intracranial circulation. Available TCD studies demonstrate low resting flow velocities including mean, systolic and diastolic velocities and impaired vasomotor reactivity in patients with vascular dementia when compared to controls [50, 51] Additionally higher values/scores of the pulsatility index, a TCD measure of increased cerebral small vessel resistance that correlates with greater white matter hyperintensities and lacunar infarcts by MRI.[52, 53] are seen in vascular dementia compared to those with Alzheimer disease and controls [51].Further studies on cerebral hemodynamics as a surrogate of cerebral perfusion are needed to examine early vascular dysfunction in at-risk populations.
Sleep Disorders: Implications for Vascular Dementia
Decrements in sleep health are quite prevalent and continue to be an under-recognized modifiable risk factor for cardiovascular disease and stroke [54].The association of sleep disorders with vascular risk factors and stroke has been well documented but is not fully understood [54].Furthermore, untreated sleep disorders produces sleepiness that has detrimental effects on mood, job performance, and accident risk, and is associated with adverse health outcomes and cognitive dysfunction [55–57].Proper sleep is critical for synaptic plasticity and memory function [57].
Obstructive sleep apnea (OSA) is a sleep disorder that is highly prevalent, occurring in up to 25 % of the general US population and up to 62 % of those older than 65 [58].Obstructive sleep apnea is defined by the apnea–hypopnea index (AHI), which is an index of OSA severity that combines apneas (pauses in breathing) and hypopneas (partial obstructions in breathing) associated with hypoxemia [59–61]. A patient with OSA has more than five AHI events per hour of sleep [60]. Clinical risk factors and the most common symptoms are presented in Table 1. The repetitive collapse of the upper airway during sleep, leads to intermittent nocturnal hypoxemia, hypercapnia and arousals from sleep associated with an increase sympathetic response. Further activation of neuro-endocrine systems (corticotropic, sympathetic, renin-aldosterone-angiotensin) in OSA can cause or exacerbate the cardiometabolic disorders associated to vascular dementia.
Poor or inadequate sleep may lead to cognitive dysfunction as suggested by the association between sleepiness, poor sleep quality, and OSA with incident dementia. A large community-based cohort of older men found that severe daytime sleepiness, a symptom closely associated with OSA and poor sleep quality, was strongly predictive of vascular dementia but did not predict non-vascular dementia [62]. In another prospective study of 4,894 patients without baseline dementia, excessive daytime sleepiness predicted cognitive decline (defined as a four-point reduction in the mini-mental score) at 2, 4, and 8 year follow up (OR = 1.26, 95 % CI 1.02-1.56). Logistic regression models were adjusted for sociodemographic, behavioral, physical, and mental health variables, and apolipoprotein E genotype [63].
In the Osteoporotic Fractures Study, elderly women (mean age of 82 years) with and without OSA were followed for a median of five years. Compared to the 193 women without OSA, the 105 women (35.2 %) with moderate to severe OSA (AHI >15 events per hour of sleep) had a greater odds of cognitive impairment and dementia (31.1 % vs. 44.8 %) in multivariable analysis (adjusted OR = 1.85, 95 % CI 1.11-3.08) [64••]. This association was mediated by the levels of hypoxemia, as opposed to measures of sleep fragmentation.
Obstructive sleep apnea is a novel risk factor for stroke and cardiovascular mortality [59, 60, 65]. Long term follow up of both the Sleep Heart Health Study and the Wisconsin Sleep Cohort show nearly threefold to fourfold higher associations between baseline OSA and incident stroke [66–69]. Obstructive sleep apnea is also known to cause a variety of cardiac arrhythmias during sleep such as bradycardia, supraventricular tachycardia, ventricular tachycardia, and atrial fibrillation. Severe OSA (AHI ≥ 30) has been linked to a fourfold increased risk of atrial fibrillation. In addition, there is evolving evidence that OSA may contribute to insulin resistance and other components of the metabolic syndrome such as obesity and increased elevated leptin levels, a hormone produced by the adipocytes strongly associated with obesity. Mounting evidence suggest that OSA is related to subclinical brain infarcts and white matter hyperintensities by MRI [70–72]. In a study of Japanese men, 25 % of patients with moderate to severe OSA had silent brain infarcts when compared to 6 % of controls.
Obstructive sleep apnea could potentiate or exacerbate established vascular risk factors, but OSA can also lead to impairments in cerebral hemodynamics. Obstructive events leading to hypoxemia, hypercapnia, and changes in intrathoracic pressures can lead to reductions in cerebral blood flow and impaired cerebral autoregulation [73–76], similar to the effects of aging and hypertension. In addition, patients with OSA had reduced cerebral blood flow velocities during apneas in the middle cerebral artery. Decreased cerebral blood flow along with impaired vasomotor reactivity and increased pulsatility index has been described in OSA during wakefulness [73].Chronic hypoxemia and hypercapnia can cause desensitization of the cerebral chemoreceptors responsible for maintaining cerebral autoregulation leading to dysfunction of cerebral hemodynamics.
An OSA “microvascular model” has been proposed [56].The vascular and neuronal damage in OSA may occur as a consequence of cerebral chemoreflex dysfunction, in addition to increased endothelin levels, and cerebral endothelial dysfunction caused by oxidative stress (hypoxemia-reoxygenation). The end result is cerebral vasoconstriction and “stiffness” of cerebral blood vessels causing or exacerbating cerebral hypoperfusion, and direct transmittal of systemic pulsatile wave pressures to the cerebral microvasculature. Cognitive dysfunction in OSA is not only a result of sleep disruption, but is related to the chronic effects of hypoxemia–reoxygenation and increased sympathetic tone leading to vascular and neuronal damage.
In animal models of spontaneously hypertensive stroke-prone rats, early microvascular damage was caused by hypoxemia-related endothelial damage leading to disruption of the blood brain barrier (BBB). This ongoing damage of the vessel wall results in small vessel rupture and microbleeds [76•].Sustained hypoxia causes dysfunction of the BBB. Hypothetically, intermittent hypoxemia–-reoxygneation, as seen in OSA, could lead to BBB leakage in susceptible individuals [77•].Additionally, chronic inflammation in OSA may cause BBB dysfunction and neuronal injury. There are elevations of leukotrienes and prostaglandings in chronic inflammatory states and in chronic intermittent hypoxemia. These molecules serve as ligands for the proliferator-activated receptors (PPRE) and the peroxisomses proliferator response element that activates downstream genes involved in chronic inflammation and other pathways that alter microvessel permeability [78•]. In addition, the transcription factor CCAT-enhancer binding protein (C/EBP) regulates the expression of PPRE. In an OSA animal model, upregulation and activation of CCAT-enhancer binding protein (C/EBP) homologous protein (CHOP) was observed in response to intermittent hypoxemia. Upregulation of these proteins leads to greater oxidative stress and signaling of apoptosis in neuronal cells [79].
Further prospective studies are needed to better characterize the pathophysiological mechanisms and the contribution of OSA in middle age to vascular dementia in late life. In addition, randomized clinical trials are needed to determine if treatments of sleep disorders in the general population is effective in the primary prevention of stroke, cardiovascular disease, and consequently vascular dementia.
Conclusion
Vascular causes of dementia are expected to become increasingly prevalent with the aging population. This is a heterogeneous group of disorders that does not have a single cause and with numerous pathological underpinnings. Controlled trials that moderate vascular risk will be important to reducing vascular dementia risk, and novel risk factors, such as sleep disorders, require attention. Advances in neuroimaging and in understanding the molecular pathways involved in different types of vascular damage provide hope for progress to limit the potential epidemic of vascular dementia as our population ages.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
2010 Alzheimer's disease facts and figures. Alzheimers Dement 2010;6:158–94.
Korczyn AD. The underdiagnosis of the vascular contribution to dementia. J Neurol Sci. 2005;229–230:3–6.
Gorelick PB, Scuteri A, Black SE, et al. Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the american heart association/american stroke association. Stroke. 2011;42:2672–713.
Dichgans M, Zietemann V. Prevention of vascular cognitive impairment. Stroke. 2012;43:3137–46.
Hachinski VC, Lassen NA, Marshall J. Multi-infarct dementia. A cause of mental deterioration in the elderly. Lancet. 1974;2:207–10.
Tomlinson BE, Blessed G, Roth M. Observations on the brains of demented old people. J Neurol Sci. 1970;11:205–42.
Prabhakaran S, Wright CB, Yoshita M, et al. Prevalence and determinants of subclinical brain infarction: the Northern Manhattan Study. Neurology. 2008;70:425–30.
Bots ML, van Swieten JC, Breteler MM, et al. Cerebral white matter lesions and atherosclerosis in the Rotterdam Study. Lancet. 1993;341:1232–7.
Kalaria RN, Ballard C. Overlap between pathology of Alzheimer disease and vascular dementia. Alzheim Dis Assoc Disord. 1999;13 Suppl 3:S115–23.
Rincon F, Wright CB. Vascular cognitive impairment. Curr Opin Neurol. 2013;26:29–36.
Sorbi S, Hort J, Erkinjuntti T, et al. EFNS-ENS Guidelines on the diagnosis and management of disorders associated with dementia. Eur J Neurol. 2012;19:1159–79.
Richard E, Reitz C, Honig LH, et al. Late-life depression, mild cognitive impairment, and dementia. JAMA Neurol. 2013;70:374–82.
Gorelick PB, Pantoni L. Advances in vascular cognitive impairment. Stroke. 2013;44:307–8.
Saczynski JS, Marcantonio ER, Quach L, et al. Cognitive trajectories after postoperative delirium. N Engl J Med. 2012;367:30–9.
Kalaria RN. Cerebrovascular disease and mechanisms of cognitive impairment: evidence from clinicopathological studies in humans. Stroke. 2012;43:2526–34.
Dong Y, Venketasubramanian N, Chan BP, et al. Brief screening tests during acute admission in patients with mild stroke are predictive of vascular cognitive impairment 3–6 months after stroke. J Neurol Neurosurg Psychiatry. 2012;83:580–5.
Jacova C, Pearce LA, Costello R, et al. Cognitive impairment in lacunar strokes: the SPS3 trial. Ann Neurol. 2012;72:351–62.
Thal DR, Grinberg LT, Attems J. Vascular dementia: different forms of vessel disorders contribute to the development of dementia in the elderly brain. Exp Gerontol. 2012;47:816–24.
Smith EE, Schneider JA, Wardlaw JM, Greenberg SM. Cerebral microinfarcts: the invisible lesions. Lancet Neurol. 2012;11:272–82.
Yakushiji Y, Hara H. [Cerebral microbleeds: clinical features and management]. Rinsho shinkeigaku =. Clinical neurology. 2012;52:1106–9.
Heringa SM, Bouvy WH, van den Berg E, Moll AC, Jaap Kappelle L, Jan Biessels G. Associations between retinal microvascular changes and dementia, cognitive functioning, and brain imaging abnormalities: a systematic review. J Cereb Blood Flow Metab 2013.
Maillard P, Seshadri S, Beiser A, et al. Effects of systolic blood pressure on white-matter integrity in young adults in the Framingham Heart Study: a cross-sectional study. Lancet Neurol. 2012;11:1039–47.
Maillard P, Carmichael O, Fletcher E, Reed B, Mungas D, DeCarli C. Coevolution of white matter hyperintensities and cognition in the elderly. Neurology. 2012;79:442–8.
Mok V, Xiong Y, Wong KK, et al. Predictors for cognitive decline in patients with confluent white matter hyperintensities. Alzheimers Dement. 2012;8:S96–S103.
de la Torre JC. Cardiovascular risk factors promote brain hypoperfusion leading to cognitive decline and dementia. Cardiovasc Psychiatry Neurol. 2012;2012:367516.
De Groot JC, De Leeuw FE, Oudkerk M, et al. Periventricular cerebral white matter lesions predict rate of cognitive decline. Ann Neurol. 2002;52:335–41.
Debette S, Markus HS. The clinical importance of white matter hyperintensities on brain magnetic resonance imaging: systematic review and meta-analysis. BMJ. 2010;341:c3666.
Marchant NL, Reed BR, DeCarli CS, et al. Cerebrovascular disease, beta-amyloid, and cognition in aging. Neurobiol Aging. 2012;33:1006.e25–1006.e36.
Lee JH, Kim SH, Kim GH, et al. Identification of pure subcortical vascular dementia using 11C-Pittsburgh compound B. Neurology. 2011;77:18–25.
Jokinen H, Lipsanen J, Schmidt R, et al. Brain atrophy accelerates cognitive decline in cerebral small vessel disease: the LADIS study. Neurology. 2012;78:1785–92.
Kloppenborg RP, Nederkoorn PJ, Grool AM, et al. Cerebral small-vessel disease and progression of brain atrophy: the SMART-MR study. Neurology. 2012;79:2029–36.
Nagai M, Hoshide S, Kario K. Hypertension and dementia. Am J Hypertens. 2010;23:116–24.
Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med. 2000;342:145–53.
Bosch J, Yusuf S, Pogue J, et al. Use of ramipril in preventing stroke: double blind randomised trial. BMJ. 2002;324:699–702.
van Vliet P. Cholesterol and late-life cognitive decline. J Alzheim Dis JAD. 2012;30 Suppl 2:S147–62.
Denkinger MD, Nikolaus T, Denkinger C, Lukas A. Physical activity for the prevention of cognitive decline: current evidence from observational and controlled studies. Z Gerontol Geriatr. 2012;45:11–6.
Verdelho A, Madureira S, Ferro JM, et al. Physical activity prevents progression for cognitive impairment and vascular dementia: results from the LADIS (Leukoaraiosis and Disability) study. Stroke. 2012;43:3331–5.
Mangialasche F, Kivipelto M, Solomon A, Fratiglioni L. Dementia prevention: current epidemiological evidence and future perspective. Alzheimer's Res Ther. 2012;4:6.
Richard E, Andrieu S, Solomon A, et al. Methodological challenges in designing dementia prevention trials - the European Dementia Prevention Initiative (EDPI). J Neurol Sci. 2012;322:64–70.
Solfrizzi V, Scafato E, Capurso C, et al. Metabolic syndrome and the risk of vascular dementia: the Italian Longitudinal Study on Ageing. J Neurol Neurosurg Psychiatry. 2010;81:433–40.
Segura B, Jurado MA, Freixenet N, Falcon C, Junque C, Arboix A. Microstructural white matter changes in metabolic syndrome: a diffusion tensor imaging study. Neurology. 2009;73:438–44.
Vieira JR, Elkind MS, Moon YP, et al. The metabolic syndrome and cognitive performance: the Northern Manhattan Study. Neuroepidemiology. 2011;37:153–9.
Feldstein CA. Association between chronic blood pressure changes and development of Alzheimer's disease. J Alzheim Dis JAD. 2012;32:753–63.
Shah NS, Vidal JS, Masaki K, et al. Midlife blood pressure, plasma beta-amyloid, and the risk for Alzheimer disease: the Honolulu Asia Aging Study. Hypertension. 2012;59:780–6.
Kario K, Pickering TG, Matsuo T, Hoshide S, Schwartz JE, Shimada K. Stroke prognosis and abnormal nocturnal blood pressure falls in older hypertensives. Hypertension. 2001;38:852–7.
Kennelly S, Collins O. Walking the cognitive "minefield" between high and low blood pressure. J Alzheim Dis JAD. 2012;32:609–21.
Jerskey BA, Cohen RA, Jefferson AL, et al. Sustained attention is associated with left ventricular ejection fraction in older adults with heart disease. J Int Neuropsychol Soc JINS. 2009;15:137–41.
Vasdekis SN, Tsivgoulis G, Athanasiadis D, et al. Cerebrovascular Reacivity Assessment in Patients with Carotid Artery Disease: A Combined TCD and NIRS Study. J Neuroimaging 2011
Kleiser B, Widder B. Course of carotid artery occlusions with impaired cerebrovascular reactivity. Stroke. 1992;23:171–4.
de la Torre JC. Cerebral hemodynamics and vascular risk factors: setting the stage for Alzheimer's disease. J Alzheim Dis JAD. 2012;32:553–67.
Lee KO, Lee KY, Lee SY, Ahn CW, Park JS. Lacunar infarction in type 2 diabetes is associated with an elevated intracranial arterial pulsatility index. Yonsei Med J. 2007;48:802–6.
Lee KY, Sohn YH, Baik JS, Kim GW, Kim JS. Arterial pulsatility as an index of cerebral microangiopathy in diabetes. Stroke. 2000;31:1111–5.
Xiong YY, Mok V, Wong A, et al. Evaluation of Age-Related White Matter Changes Using Transcranial Doppler Ultrasonography. J Neuroimaging. 2013;23:53–7.
Somers VK, White DP, Amin R, et al. Sleep apnea and cardiovascular disease: an American Heart Association/american College Of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council On Cardiovascular Nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). Circulation. 2008;118:1080–111.
Shafazand S, Wallace DM, Vargas SS, et al. Sleep disordered breathing, insomnia symptoms, and sleep quality in a clinical cohort of U.S. Hispanics in south Florida. J Clin Sleep Med. 2012;8:507–14.
Zimmerman ME, Aloia MS. Sleep-Disordered Breathing and Cognition in Older Adults. Curr Neurol Neurosci Rep. 2012;12:537–46.
Wang G, Grone B, Colas D, Appelbaum L, Mourrain P. Synaptic plasticity in sleep: learning, homeostasis and disease. Trends Neurosci. 2011;34:452–63.
Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5:136–43.
•• Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353:2034–41. Prospective observational study that linked obstructive sleep apnea with increased risk of stroke and vascular death.
Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165:1217–39.
Wallace DM, Ramos AR, Rundek T. Sleep disorders and stroke. Int J Stroke. 2012;7:231–42.
Elwood PC, Bayer AJ, Fish M, Pickering J, Mitchell C, Gallacher JE. Sleep disturbance and daytime sleepiness predict vascular dementia. J Epidemiol Community Health. 2011;65:820–4.
Jaussent I, Bouyer J, Ancelin ML, et al. Excessive sleepiness is predictive of cognitive decline in the elderly. Sleep. 2012;35:1201–7.
•• Yaffe K, Laffan AM, Harrison SL, et al. Sleep-disordered breathing, hypoxia, and risk of mild cognitive impairment and dementia in older women. JAMA. 2011;306:613–9. Seminal prospective study demonstrating that moderate to severe sleep apnea is a predictor of mild cognitive impairment and dementia in an elderly cohort of women.
Redline S, Yenokyan G, Gottlieb DJ, et al. Obstructive sleep apnea-hypopnea and incident stroke: the sleep heart health study. Am J Respir Crit Care Med. 2010;182:269–77.
Arzt M, Young T, Finn L, Skatrud JB, Bradley TD. Association of sleep-disordered breathing and the occurrence of stroke. Am J Respir Crit Care Med. 2005;172:1447–51.
Hermann DM, Bassetti CL. Sleep-related breathing and sleep-wake disturbances in ischemic stroke. Neurology. 2009;73:1313–22.
Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365:1046–53.
Kiernan TE, Capampangan DJ, Hickey MG, Pearce LA, Aguilar MI. Sleep apnea and white matter disease in hypertensive patients: a case series. Neurologist. 2011;17:289–91.
Minoguchi K, Yokoe T, Tazaki T, et al. Silent brain infarction and platelet activation in obstructive sleep apnea. Am J Respir Crit Care Med. 2007;175:612–7.
Nishibayashi M, Miyamoto M, Miyamoto T, Suzuki K, Hirata K. Correlation between severity of obstructive sleep apnea and prevalence of silent cerebrovascular lesions. J Clin Sleep Med. 2008;4:242–7.
Suzuki E, Yorifuji T, Ueshima K, et al. Sleep duration, sleep quality and cardiovascular disease mortality among the elderly: a population-based cohort study. Prev Med. 2009;49:135–41.
Ramos AR, Cabral D, Lee DJ, Sacco RL, Rundek T. Cerebrovascular pulsatility in patients with sleep-disordered breathing. Sleep Breath. 2013;17:723–6.
Virtanen J, Noponen T, Salmi T, Toppila J, Merilainen P. Impaired cerebral vasoreactivity may cause cerebral blood volume dip following obstructive sleep apnea termination. Sleep Breath. 2012;16:309–12.
Urbano F, Roux F, Schindler J, Mohsenin V. Impaired cerebral autoregulation in obstructive sleep apnea. J Appl Physiol. 2008;105:1852–7.
Schreiber S, Bueche CZ, Garz C, Braun H. Blood brain barrier breakdown as the starting point of cerebral small vessel disease? - New insights from a rat model. Exp Transl Stroke Med. 2013;5(1):4.
• Lim DC, Pack AI. Obstructive sleep apnea and cognitive impairment: Addressing the blood–brain barrier. Sleep Med Rev. 2013. doi:10.1016/j.smrv.2012.12.003. Review on the mechanisms that could explain the link between obstructive sleep apnea cognitive impairment. The review discusses the role of chronic intermittent hypoxemia, inflammation and cerebrovascular and blood brain barrier dysfunction.
• Chou YT, Zhan G, Zhu Y, et al. C/EBP Homologous Binding Protein (CHOP) Underlies Neural Injury in Sleep Apnea Model. Sleep. 2013;36(4):481–92. Study demonstrating the effect of hypoxemia in neural injury and neuronal apoptosis in an animal model of sleep apnea.
Barbe F, Duran-Cantolla J, Sanchez-de-la-Torre M, et al. Effect of continuous positive airway pressure on the incidence of hypertension and cardiovascular events in nonsleepy patients with obstructive sleep apnea: a randomized controlled trial. JAMA. 2012;307:2161–8.
Compliance with Ethics Guidelines
Conflict of Interest
Alberto R. Ramos has received compensation from MCMC, LLC for serving as a consultant.
Salim I. Dib declares that he has no conflict of interest.
Clinton B. Wright declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ramos, A.R., Dib, S.I. & Wright, C.B. Vascular Dementia. Curr Transl Geriatr and Exp Gerontol Rep 2, 188–195 (2013). https://doi.org/10.1007/s13670-013-0054-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13670-013-0054-5