Abstract
Purpose of Review
The purpose of this review is to describe the latest methods of fertility preservation for female cancer patients, as well as the associated psychological benefits, pregnancy outcomes, and oncological outcomes of these techniques.
Recent Findings
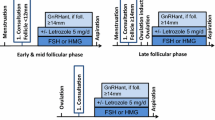
Using random-start controlled ovarian stimulation for embryo and oocyte cryopreservation provides adequate oocyte yield and minimizes delay to starting cancer treatment. Protocols including estrogen-lowering medications should be used in women with hormone-sensitive cancers. Newer methods including ovarian tissue cryopreservation and ovarian transposition have promising pregnancy outcomes. Ovarian suppression helps prevent premature ovarian failure in young women with breast cancer and women who require rapid start systemic cancer treatment. Fertility-sparing surgery is safe in women with early-stage cervical and ovarian cancer. Providing counseling regarding fertility preservation yields significant psychological benefits for patients.
Summary
Improved cancer survival and delayed childbearing have resulted in a greater need for fertility preservation for female cancer patients. The most commonly used fertility preservation strategy is controlled ovarian stimulation (COS). A number of new studies provide data on ways to maximize COS such as through use of random-start protocols and the addition of medications that lower estrogen levels. Recent research also suggests that newer methods including ovarian tissue cryopreservation and ovarian transposition may provide valuable alternatives to COS. However, many topics remain controversial, including where to re-transplant cryopreserved ovaries, the best surgical approach to ovarian transposition, short- versus long-term benefits of ovarian transposition, and the role of ovarian suppression for fertility preservation.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA A Cancer J Clin. 2019;69(1):7–34.
Fidler MM, Gupta S, Soerjomataram I, Ferlay J, Steliarova-Foucher E, Bray F. Cancer incidence and mortality among young adults aged 20–39 years worldwide in 2012: a population-based study. Lancet Oncol. 2017;18(12):1579–89.
Mathews TJ, Hamilton BE. Mean age of mother, 1970–2000. Natl Vital Stat Rep. 2002;51(1):1–16.
Woodruff TK. The emergence of a new interdiscipline: oncofertility. Cancer Treat Res. 2007;138(3):3–11.
•• Oktay K, Harvey BE, Loren AW. Fertility preservation in patients with cancer: ASCO clinical practice guideline update summary. J Oncol Pract. 2018;14(6):381-385. This article provides updated guidelines from the American Society of Clinical Oncology regarding fertility preservation for adults and children with cancer.
•• Practice Committee of the American Society for Reproductive Medicine. Fertility preservation in patients undergoing gonadotoxic therapy or gonadectomy: a committee opinion. Fertil Steril. 2019;112:1022–33. This article provides updated guidelines from the American Society for Reproductive Medicine regarding fertility preservation for both men and women with cancer.
Stensheim H, Cvancarova M, Moller B, Fossa SD. Pregnancy after adolescent and adult cancer: a population-based matched cohort study. Int J Cancer. 2011;129(5):1255–1236.
Faddy MJ, Gosden RG, Guugeon A, Richardson SJ, Nelson JF. Accelerated disappearance of ovarian follicles in mid-life: implications for forecasting menopause. Hum Reprod. 1992;7(10):1342–6.
Faddy MJ, Gosden RG. A model conforming the decline in follicle numbers to the age of menopause in women. Hum Reprod. 1996;11(7):1484–6.
Wo JU, Viswanathan AN. Impact of radiotherapy on fertility, pregnancy and neonatal outcomes in female cancer patients. Int J Radiat Oncol Biol Phys. 2009;3(5):1304–12.
Sonmezer M, Oktay K. Fertility preservation in female patients. Hum Repro Update. 2004;10(3):251–66.
Wallace WHB, Thomson AB, Saran F, Kelsey TW. Predicting age of ovarian failure after radiation to a field that includes the ovaries. 2005;62(3):738–44.
Spears N, Lopes F, Stefandsottir A, Rossi V, De Felici MD, Anderson RA, Klinger FG. Ovarian damage from chemotherapy and current approaches to its protection. Hum Repro Update. 2009;25(6):673–93.
van Dorp W, Haut R, Anderson RA, Mulder RL, van den Heuvel-Eibrink MM, van Dulmen-den BE, Su HI, Winther JF, Hudson MM, Levine JM, Wallace WH. Reproduction function and outcomes in female survivors of childhood, adolescent, and young adult cancer: a review. J Clin Oncol. 2018;6(21):2169–80.
Letourneau JM, Ebbel EE, Katz PP, Oktay KH, McCulloch CE, Ai WZ, Chien AJ, Melisko ME, Ceders MI, Rosen MP. Acute ovarian failure underestimates age-specific reproductive impairment for young women undergoing chemotherapy for cancer. Cancer. 2011;118(7):1933–9.
• Schuurman T, Zilver S, Samuels S, Winne S, Amant F, Van Trommel N, Lok C. Fertility-Sparing Surgery in Gynecologic Cancer: A Systematic Review. Cancers. 2021;13(5):1008. This systematic review suggests acceptable oncologic outcomes and reasonable pregnancy outcomes for patients after fertility-sparing surgery.
Somigliana E, Ragni G, Benedetti F, Borroni R, Vegetti W, Crosignani PG. Does laparoscopic excision of endometriotic ovarian cysts significant affect ovarian reserve? Insights from IVF cycles Hum Repro. 2003;18(11):2450–3.
Ye XP, Yang YZ, Sun XX. A retrospective analysis of the effect of salpingectomy on serum antiMullerian hormone level and ovarian reserve. Am J Obstet and Gynecol. 2015;212(1):53e1–53e10.
Cakmak H, Katz A, Ceders MI, Rosen MP. Effective method for emergency fertility preservation: random-start controlled ovarian stimulation. Fertil Steril. 2013;100(6):1673–80.
Lambertini M, Del Mastro L, Pescio M, Anderson CY, Azim HA, Peccatori FA, Costa M, Revelli A, Salvagno F, Gennari A, Ubaldi FM, La Sala GB, De Stefano C, Wallach WH, Partridge AH, Anserini P. Cancer and fertility preservation: international recommendations from an expert meeting. BMC Medicine. 2016;41(1).
Oktay K, Buyuk E, Davis O, Yermakova I, Veeck L, Rosenwaks Z. Fertility preservation in breast cancer patients: IVF and embryo cryopreservation after ovarian stimulation with tamoxifen. Human Reprod. 2003;18(1):90–5.
Oktay K, Buyuk E, Libertella N, Akar M, Rosenwaks Z. Fertility preservation in breast cancer patients: a prospective controlled comparison of ovarian stimulation with tamoxifen and letrozole for embryo cryopreservation. J Clin Oncol. 2005;23(19):4347–53.
• Kawwass JF, Shandley LM, Boulet SL, Hipp HS. Oncologic oocyte cryopreservation: national comparison of fertility preservation between women with and without cancer. J Assist Reprod Genet. 2020;37(4):883-890.
Gosden RG, Baird DT, Wade JC, Webb R. Restoration of fertility to oophorectomized sheep by ovarian autografts stored at -196 degrees C. Hum Reprod. 1994;9(4):597–603.
• Anderson R, Wallash WHB, Telfer EE. Ovarian tissue cryopreservation for fertility preservation: clinical and research perspectives. Hum Reprod Open. 2017(1). This study demonstrates successful pregnancies following ovarian tissue cryopreservation followed by transplantation.
Donnez J, Dolmans MM, Pellicer A, Diaz-Garcia C, Serrano MS, Schmidt KT, Ernst E, Luyckx V, Anderson CY. Restoration of ovarian activity and pregnancy after transplantation of cryopreserved ovarian tissue: a review of 60 cases of reimplantation. Fertil Steril. 2013;99(6):1503–13.
Jadoul P, Guilmain A, Squifflet J, Luyckx M, Votino R, Wyns C, Dolmans MM. Efficacy of ovarian tissue cryopreservation for fertility preservation: lessons learned from 545 cases. Hum Reprod. 2017;32(5):1046–54.
Gubbala K, Laios A, Gallos I, Pathiraja P, Haldar K, Ind T. Outcomes of ovarian transposition in gynaecological cancers; a systematic review and meta-analysis. J Ovarian Res. 2014;7(69).
Fernandez-Pineda I, Davidoff AM, Lu L, Rao BN, Wilson CL, Srivastava DK, Klosky JL, Metzger ML, Krasin MJ, Ness KK, Pui CH, Robinson LL, Hudson MM, Sklar CA, Green DM, Chemaitilly W. Impact of ovarian transposition before pelvic irradiation on ovarian function among long-term survivors of childhood Hodgkin lymphoma: a report from the St. Jude Lifetime Cohort Study. Pediatr Blood Cancer. 2018;65(9).
Prodromidou A, Iavazzo C, Fotiou A, Psomiadou V, Douligeris A, Vorgias G, Kalinoglou N. Short- and long-term outcomes after abdominal radical trachelectomy versus radical hysterectomy for early-stage cervical cancer: a systematic review of the literature and meta-analysis. Arch Gynecol Obstet. 2019;300(1):25–31.
Plett H, Harter P, Ataseven B, Heitz F, Prader S, Schneider S, Heikaus S, Fisseler-Eckhoff A, Kommoss F, Lax SF, Staebler A, Traut A, du Bois A. Fertility-sparing surgery and reproductive-outcomes in patients with borderline ovarian tumors. Gynecol Oncol. 2020;157(2):411–7.
Bentivegna E, Gouy S, Maulard A, Pautier P, Leary A, Colombo N, Morice P. Fertility-sparing surgery in epithelial ovarian cancer: a systematic review of oncological issues. Ann Oncol. 2016;27(11):1994–2004.
Melamed A, Rizzo AE, Nitecki R, Gockley AA, Bregar AJ, Schorge JO, Del Carmen MG, Rauh-Hain JA. All-cause mortality after fertility-sparing surgery for stage I epithelial ovarian cancer. Obstet Gynecol. 2017;130(1):71–9.
Westin SN, Fellman B, Sun CC, Broaddus RR, Woodall ML, Pal N, Urbauer DL, Ramondetta LM, Schmeler KM, Soliman PT, Fleming ND, Burzawa JK, Nick AM, Milbourne AM, Yuan Y, Lu KH, Bodurka DC, Coleman RL, Yates MS. Prospective phase II trial of levonorgestrel intrauterine device: nonsurgical approach for complex atypical hyperplasia and early-stage endometrial cancer. Am J Obstet Gynecol. 2021;224(2):191.e1-191.e15.
Harrison RF, He W, Fu S, Zhao H, Sun CC, Suidan RS, Woodard TL, Rauh-Hain JA, Westin SN, Giordano SH, Meyer LA. National patterns of care and fertility outcomes for reproductive-aged women with endometrial cancer or atypical hyperplasia. Am J Obstet Gynecol. 2019;221(5):474.e1-474.e11.
Wei J, Zhang W, Feng L, Gao W. Comparison of fertility-sparing treatments in patients with early endometrial cancer and atypical complex hyperplasia: a meta-analysis and systematic review. Medicine (Baltimore). 2017;96(37):e8034.
Lambertini M, Ceppi M, Poggio F, Peccatori FA, Azim HA, Ugolini D, Pronzato P, Loibl S, Moore HCG, Partridge AH, Bruzzi P, De Mastro LD. Ovarian suppression using luteinizing hormone-releasing agonists during chemotherapy to preserve ovarian function and fertility of breast cancer patients: a meta-analysis of randomized studies. Ann Oncol. 2015;26(12):2408–19.
Lambertini M, Moore HCF, Leonard RCF, Loibl S, Munster P, Bruzzone M, Boni L, Unger JM, Anderson RA, Mehta K, Minton S, Poggio F, Albain KS, Adamson DJA, Gerber B, Cripps A, Bertelli G, Seiler S, Ceppi M, Partridge A, Del Mastro L. Gonadotropin-releasing hormone agonists during chemotherapy for preservation of ovarian function and fertility in premenopausal patients with early breast cancer: a systematic review and meta-analysis of individual patient-level data. J Clin Oncol. 2018;36(19):1981–90.
Partridge AH, Gelber S, Peppercorn J, Sampson E, Knudsen K, Laufer M, Rosenberg R, Przypyszny M, Rein A, Winer EP. Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol. 2004;22(20):4174–83.
Logan S, Perz J, Ussher JM, Peate M, Anazodo A. Systematic review of fertility-related psychological distress in cancer patients: information on an improved model of care. Psycho-Oncology. 2018;28(1):22–30.
Deshpande NA, Braun IM, Mayer FL. Impact of fertility preservation counseling and treatment on psychological outcomes among women with cancer: a systematic review. Cancer. 2015;121(22):3938–47.
Benedict C, Thom B, Friedman DN, Pottenger E, Raghunathan N, Kelvin JF. Fertility information needs and concerns post-treatment contribute to lower quality of life among young adult female cancer survivors. Support Care Cancer. 2018;26(7):2209–15.
Cardozo ER, Thomson AP, Karmon AE, Dickinson KA, Wright DL, Sabatini ME. Ovarian stimulation and in-vitro fertilization outcomes of cancer patients undergoing fertility preservation compared to age matched controls: a 17-year experience. J Assist Reprod Genet. 2015;32(4):587–96.
Marklund A, Lundberg DE, Eloranta S, Hedayati E, Petterson K, Rodriguez-Wallberg KA. Reproductive outcomes after breast cancer in women with vs without fertility preservation. JAMA Oncol. 2021;7(1):86–91.
Moravek MB, Confino R, Smith KN, Kazer RR, Klock SC, Lawson AK, Gradishar WJ, Pavone ME. Long-term outcomes in cancer patients who did or did not pursue fertility preservation. Fertil Steril. 2018;109(2):349–55.
Marklund A, Eloranta S, Wikander I, Kitlinski ML, Lood M, Nedstrand E, Thurin-Kjellberg A, Zhang P, Bergh J, Rodriguez-Wallberg K. Efficacy and safety of controlled ovarian stimulation using GnRH antagonist protocols for emergency fertility preservation in young women with breast cancer- a prospective nationwide Swedish multicenter study. Hum Reprod. 2020;35(4):929–38.
Morice P, Thiam-Ba R, Castaigne D, Haie-Meder C, Gerbaulet A, Pautier P, Duvillard P, Michel G. Fertility results after ovarian transposition for pelvic malignancies treated by external irradiation or brachytherapy. Human Reprod. 1998;13(3):660–3.
Moravek MB, Confino R, Lawson AK, Smith KN, Kazer RR, Klock SC, Gradishar WJ, Jeruss JS, Pavone ME. Predictors and outcomes in breast cancer patients who did or did not pursue fertility preservation. Breast Cancer Res Treat. 2021;186(2):429–37.
Letourneau JM, Wald K, Sinha N, Juarez-Hernandez F, Harris E, Ceders M, McCulloch CE, Dolezal M, Chien AJ, Rosen MP. Fertility preservation before breast cancer treatment appears unlikely to affect disease-free survival at a median follow-up of 42 months after fertility-preservation consultation. Cancer. 2019;126(3):487–95.
Masciaganelo R, Bosisio C, Donnez J, Amorim CA, Dolmans MM. Safety of ovarian tissue transplantation in patients with borderline ovarian tumors. Human Reprod. 2018;33(2):212–9.
Nezhat C, Roman RA, Rambhatla A, Nezhat F. Reproductive and oncologic outcomes after fertility-sparing surgery for early stage cervical cancer: a systematic review. Fertil Steril. 2020;113(4):685–703.
Yin J, Wang Y, Shan Y, Li Y, Jin Y, Pan L. Pregnancy and oncologic outcomes of early stage low grade epithelial ovarian cancer after fertility sparing surgery: a retrospective study in one tertiary hospital of China. Journal of Ovarian Research. 2019;12(1):44.
Johansen G, Dahm-Kahler P, Staf C, Radestad AF, Rodriguez-Wallberg KA. Fertility-sparing surgery for treatment of non-epithelial ovarian cancer: oncological and reproductive outcomes in a prospective nationwide population-based cohort study. Gynecol Onc. 2019;155(2):287–93.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors report no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Reproductive Endocrinology and Infertility (REI)
Rights and permissions
About this article
Cite this article
Naert, M.N., Greer, A. & Elias, K.M. Oncofertility: a Review. Curr Obstet Gynecol Rep 10, 83–91 (2021). https://doi.org/10.1007/s13669-021-00312-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13669-021-00312-5