Abstract
Purpose of Review
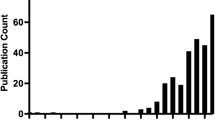
While the number of lung transplants continues to increase, there remains an imbalance between potential lung transplant candidates and acceptable donor lungs resulting in excess mortality. We sought to describe the current state of donor acceptance practices and highlight novel approaches that have the potential to result in an increase in acceptable lungs available for transplant.
Recent Findings
Increased utilization of lungs from donors with positive nucleic acid amplification tests for hepatitis C, donation after circulatory death, lungs conditioned for transplant at Centralized Lung Evaluation facilities using ex vivo lung perfusion, and improvements in organ storage during transport, have the potential to immediately increase the number of lungs suitable for transplant. In the future, application of advanced therapeutics using the ex vivo lung perfusion, stem-cell and gene therapy, and cross-circulation organ support may allow for transplant of previously non-transplantable organs.
Summary
Scientific advances in the management of donor organs may conceivably lead to a future where lungs are tailored to the unique needs of the potential recipient, resulting in an increase in lung transplants performed and improvements in long-term survival sorely desired by clinicians, researchers, and patients alike.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Chambers DC, Cherikh WS, Goldfarb SB, Hayes D, Kucheryavaya AY, Toll AE, et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: thirty-fifth adult lung and heart-lung transplant report—2018; focus theme: multiorgan transplantation. J Heart Lung Transplant. 2018;37(10):1169–83.
Lentine KL, Smith JM, Miller JM, Bradbrook K, Larkin L, Weiss S, et al. OPTN/SRTR 2021 annual data report: kidney. Am J Transplant. 2023;23(2):S21-120.
Valapour M, Skeans MA, Smith JM, Edwards LB, Cherikh WS, Uccellini K, et al. OPTN/SRTR 2015 annual data report: lung. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2017;17(Suppl 1):357–424.
Stewart D, Hasz R, Lonze B. Beyond donation to organ utilization in the USA. Curr Opin Organ Transplant. 2023;28(3):197–206.
Mulvihill M, Lee H, Weber J, Choi A, Cox M, Yerokun B, et al. Variability in donor organ offer acceptance and lung transplantation survival. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2020;39(4):353–62.
De Meester J, Smits JM, Persijn GG, Haverich A. Lung transplant waiting list: differential outcome of type of end-stage lung disease, one year after registration. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 1999;18(6):563–71.
Sundaresan S, Trachiotis GD, Aoe M, Patterson GA, Cooper JD. Donor lung procurement: assessment and operative technique. Ann Thorac Surg. 1993;56(6):1409–13.
Reul RM, Loor G, Garcha PS, Goss JA, Rana AA. Allograft discard risk index for lung transplantation. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2021;40(12):1658–67.
Chambers DC, Zuckermann A, Cherikh WS, Harhay MO, Hayes D, Hsich E, et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: 37th adult lung transplantation report - 2020; focus on deceased donor characteristics. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2020;39(10):1016–27.
Meers C, Van Raemdonck D, Verleden GM, Coosemans W, Decaluwe H, De Leyn P, et al. The number of lung transplants can be safely doubled using extended criteria donors; a single-center review. Transpl Int Off J Eur Soc Organ Transplant. 2010;23(6):628–35.
Stehlik J, Smits J, Jarcho JA, Lehman R, Cherikh W, Mehra MR. The opioid use crisis and organ transplantation: a comparison of the United States and Europe. J Heart Lung Transplant. 2018;37(4):S188.
Woolley AE, Singh SK, Goldberg HJ, Mallidi HR, Givertz MM, Mehra MR, et al. Heart and lung transplants from HCV-infected donors to uninfected recipients. N Engl J Med. 2019;380(17):1606–17.
Lewis TC, Lesko M, Rudym D, Lonze BE, Mangiola M, Natalini JG, et al. One-year immunologic outcomes of lung transplantation utilizing hepatitis C-viremic donors. Clin Transplant. 2022;36(8): e14749.
• Li SS, Osho A, Moonsamy P, Wolfe S, Villavicencio MA, Langer N, et al. Outcomes of lung transplantation from hepatitis C viremic donors. Ann Thorac Surg. 2022;113(5):1598–607. Outcomes of lung transplantation from hepatitis C viremic donors.
Aslam S, Grossi P, Schlendorf KH, Holm AM, Woolley AE, Blumberg E, et al. Utilization of hepatitis C virus-infected organ donors in cardiothoracic transplantation: an ISHLT expert consensus statement. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2020;39(5):418–32.
Avlonitis VS, Fisher AJ, Kirby JA, Dark JH. Pulmonary transplantation: the role of brain death in donor lung injury. Transplantation. 2003;75(12):1928–33.
Nijboer WN, Schuurs TA, van der Hoeven J, Leuvenink HGD, van der Heide JJH, van Goor H, et al. Effects of brain death on stress and inflammatory response in the human donor kidney. Transplant Proc. 2005;37(1):367–9.
Krutsinger D, Reed RM, Blevins A, Puri V, De Oliveira NC, Zych B, et al. Lung transplantation from donation after cardiocirculatory death: a systematic review and meta-analysis. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2015;34(5):675–84.
Van Raemdonck D, Keshavjee S, Levvey B, Cherikh WS, Snell G, Erasmus M, et al. Donation after circulatory death in lung transplantation-five-year follow-up from ISHLT Registry. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2019;38(12):1235–45.
Siddique A, Urban M, Strah H, Herber K, Morrow L, Loor G, et al. Controlled DCD lung transplantation: circumventing imagined and real barriers-time for an international taskforce? J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2022;41(9):1198–203.
Choi K, Spadaccio C, Villavicencio M, Langlais B, Pennington K, Ribeiro R, et al. (257) National trends of lung allograft utilization during donation-after-circulatory-death (DCD) heart procurement in the United States. J Heart Lung Transplant. 2023;42(4, Supplement):S124.
Cypel M, Rubacha M, Yeung J, Hirayama S, Torbicki K, Madonik M, et al. Normothermic ex vivo perfusion prevents lung injury compared to extended cold preservation for transplantation. Am J Transplant. 2009;9(10):2262–9.
Jirsch DW, Fisk RL, Couves CM. Ex vivo evaluation of stored lungs. Ann Thorac Surg. 1970;10(2):163–8.
Steen S, Sjöberg T, Pierre L, Liao Q, Eriksson L, Algotsson L. Transplantation of lungs from a non-heart-beating donor. Lancet Lond Engl. 2001;357(9259):825–9.
Steen S, Ingemansson R, Eriksson L, Pierre L, Algotsson L, Wierup P, et al. First human transplantation of a nonacceptable donor lung after reconditioning ex vivo. Ann Thorac Surg. 2007;83(6):2191–4.
Gouin C, Vu Manh TP, Jouneau L, Bevilacqua C, De Wolf J, Glorion M, et al. Cell type- and time-dependent biological responses in ex vivo perfused lung grafts. Front Immunol. 2023;14:1142228.
Yeung JC, Zamel R, Klement W, Bai XH, Machuca TN, Waddell TK, et al. Towards donor lung recovery—gene expression changes during ex vivo lung perfusion of human lungs. Am J Transplant. 2018;18(6):1518–26.
Yeung JC, Cypel M, Machuca TN, Koike T, Cook DJ, Bonato R, et al. Physiologic assessment of the ex vivo donor lung for transplantation. J Heart Lung Transplant. 2012;31(10):1120–6.
Takahashi M, Cheung HYA, Watanabe T, Zamel R, Cypel M, Liu M, et al. Strategies to prolong homeostasis of ex vivo perfused lungs. J Thorac Cardiovasc Surg. 2021;161(6):1963–73.
Van De Wauwer C, van Suylen V, Zhang ZL, Verschuuren EAM, van der Bij W, Gan CT, et al. Is logistically motivated ex vivo lung perfusion a good idea? Front Transplant. 2022. https://doi.org/10.3389/frtra.2022.988950.
Cypel M, Yeung JC, Liu M, Anraku M, Chen F, Karolak W, et al. Normothermic ex vivo lung perfusion in clinical lung transplantation. N Engl J Med. 2011;364(15):1431–40.
Sanchez PG, Cantu E, Hartwig M, D’Ovidio F, Machuca T, Whitson B, et al. The NOVEL Study. A multi-center clinical trial studying the safety of ex vivo lung perfusion. J Heart Lung Transplant. 2020;39(4):S110.
Warnecke G, Van Raemdonck D, Smith MA, Massard G, Kukreja J, Rea F, et al. Normothermic ex-vivo preservation with the portable Organ Care System Lung device for bilateral lung transplantation (INSPIRE): a randomised, open-label, non-inferiority, phase 3 study. Lancet Respir Med. 2018;6(5):357–67.
Loor G, Warnecke G, Villavicencio MA, Smith MA, Kukreja J, Ardehali A, et al. Portable normothermic ex-vivo lung perfusion, ventilation, and functional assessment with the Organ Care System on donor lung use for transplantation from extended-criteria donors (EXPAND): a single-arm, pivotal trial. Lancet Respir Med. 2019;7(11):975–84.
Choi K. National trends in utilization of ex-vivo lung perfusion in lung transplantation [Internet]. Mechanical Support and Thoracic Transplantation Summit. The Omni King Edward Hotel, Toronto, ON, Canada. 2023. Available from: https://www.aats.org/resources/national-trends-in-utilization-of-ex-vivo-lung-perfusion-in-lung-transplantation.
Cypel M, Yeung JC, Donahoe L, Chen M, Zamel R, Hoetzenecker K, et al. Normothermic ex vivo lung perfusion: does the indication impact organ utilization and patient outcomes after transplantation? J Thorac Cardiovasc Surg. 2020;159(1):346-355.e1.
Peel JK, Keshavjee S, Naimark D, Liu M, Sorbo LD, Cypel M, et al. Determining the impact of ex-vivo lung perfusion on hospital costs for lung transplantation: a retrospective cohort study. J Heart Lung Transplant. 2023;42(3):356–67.
• Chen Q, Malas J, Krishnan A, Thomas J, Megna D, Egorova N, et al. Limited cumulative experience with ex vivo lung perfusion is associated with inferior outcomes after lung transplantation. J Thorac Cardiovasc Surg. 2024;167(1):371–379.e8. This paper highlights that despite increasing interest and use of EVLP systems, transplant outcomes remain highly linked to the experience of the team conducting EVLP. Notably this remains a substantial limitation of the platform and currently limits widespread adoption.
• Mallea JM, Hartwig MG, Keller CA, Kon Z, Iii RNP, Erasmus DB, et al. Remote ex vivo lung perfusion at a centralized evaluation facility. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2022;41(12):1700–11. This paper highlights that as cost and efficacy of using EVLP systems remains a challenge, centralization of EVLP at specialized centers may serve as a better method to improved lung recovery and utilization of EVLP to enable more transplants.
Nakajima D, Cypel M, Bonato R, Machuca TN, Iskender I, Hashimoto K, et al. Ex vivo perfusion treatment of infection in human donor lungs. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2016;16(4):1229–37.
Cloer CM, Givens CS, Buie LK, Rochelle LK, Lin YT, Popa S, et al. Mitochondrial transplant after ischemia reperfusion promotes cellular salvage and improves lung function during ex-vivo lung perfusion. J Heart Lung Transplant. 2023;42(5):575–84.
Lin H, Chen M, Tian F, Tikkanen J, Ding L, Cheung HYA, et al. α1-Anti-trypsin improves function of porcine donor lungs during ex-vivo lung perfusion. J Heart Lung Transplant. 2018;37(5):656–66.
Arni S, Maeyashiki T, Latshang T, Opitz I, Inci I. Ex vivo lung perfusion with K(ATP) channel modulators antagonize ischemia reperfusion injury. Cells. 2021;10(9):2296.
Stone ML, Sharma AK, ValeriaR M, Gehrau RC, Mulloy DP, Zhao Y, et al. Ex vivo perfusion with adenosine A2A receptor agonist enhances rehabilitation of murine donor lungs after circulatory death. Transplantation. 2015;99(12):2494–503.
Machuca TN, Cypel M, Bonato R, Yeung JC, Chun YM, Juvet S, et al. Safety and efficacy of ex vivo donor lung adenoviral IL-10 gene therapy in a large animal lung transplant survival model. Hum Gene Ther. 2017;28(9):757–65.
Ku TJ, Cypel M, Ribeiro RV, Ferreira VH, Kumar D, Humar A. Ex-vivo lung perfusion mediated delivery of rituximab to clear latent Epstein-Barr virus. J Heart Lung Transplant. 2019;38(4):S54–5.
Galasso M, Feld JJ, Watanabe Y, Pipkin M, Summers C, Ali A, et al. Inactivating hepatitis C virus in donor lungs using light therapies during normothermic ex vivo lung perfusion. Nat Commun. 2019;10(1):481.
Matthay MA, Calfee CS, Zhuo H, Thompson BT, Wilson JG, Levitt JE, et al. Treatment with allogeneic mesenchymal stromal cells for moderate to severe acute respiratory distress syndrome (START study): a randomised phase 2a safety trial. Lancet Respir Med. 2019;7(2):154–62.
Matthay MA, Goolaerts A, Howard JP, Lee JW. Mesenchymal stem cells for acute lung injury: preclinical evidence. Crit Care Med. 2010;38(10 Suppl):S569–73.
Nakajima D, Watanabe Y, Ohsumi A, Pipkin M, Chen M, Mordant P, et al. Mesenchymal stromal cell therapy during ex vivo lung perfusion ameliorates ischemia-reperfusion injury in lung transplantation. J Heart Lung Transplant. 2019;38(11):1214–23.
Guenthart BA, O’Neill JD, Kim J, Fung K, Vunjak-Novakovic G, Bacchetta M. Cell replacement in human lung bioengineering. J Heart Lung Transplant. 2019;38(2):215–24.
Ali A, Wang A, Ribeiro RVP, Beroncal EL, Baciu C, Galasso M, et al. Static lung storage at 10°C maintains mitochondrial health and preserves donor organ function. Sci Transl Med. 2021;13(611):eabf7601.
Priest C, Tontonoz P. Inter-organ cross-talk in metabolic syndrome. Nat Metab. 2019;1(12):1177–88.
O’Neill JD, Guenthart BA, Hozain AE, Bacchetta M. Xenogeneic support for the recovery of human donor organs. J Thorac Cardiovasc Surg. 2022;163(4):1563–70.
Hough O, Mariscal A, Yamamoto H, Mangat H, Taniguchi D, Gokhale H, et al. (113) Improved ex vivo lung perfusion (EVLP) with dialysis and nutrition to achieve successful 36h EVLP and lung transplantation. J Heart Lung Transplant. 2023;42(4):S60.
Lillehei CW. Controlled cross circulation for direct-vision intracardiac surgery; correction of ventricular septal defects, atrioventricularis communis, and tetralogy of Fallot. Postgrad Med. 1955;17(5):388–96.
O’Neill JD, Guenthart BA, Kim J, Chicotka S, Queen D, Fung K, et al. Cross-circulation for extracorporeal support and recovery of the lung. Nat Biomed Eng. 2017;1(3):1–15.
Hozain AE, Tipograf Y, Pinezich MR, Cunningham KM, Donocoff R, Queen D, et al. Multiday maintenance of extracorporeal lungs using cross-circulation with conscious swine. J Thorac Cardiovasc Surg. 2020;159(4):1640-1653.e18.
Griesemer A, Yamada K, Sykes M. Xenotransplantation: immunological hurdles and progress toward tolerance. Immunol Rev. 2014;258(1):241–58.
Sykes M, Sachs DH. Transplanting organs from pigs to humans. Sci Immunol [Internet]. 2019[cited 2019 Nov 14];4(41). Available from: https://immunology.sciencemag.org/content/4/41/eaau6298.
• Hozain AE, O’Neill JD, Pinezich MR, Tipograf Y, Donocoff R, Cunningham KM, et al. Xenogeneic cross-circulation for extracorporeal recovery of injured human lungs. Nat Med. 2020;26(7):1102–13. This study highlights the first time a damaged human lung was successfully recovered using a xenogeneic swine host. This foundational study may ultimately lay the groundwork for future research that can enable highly specialized organ therapeutics and bioengineering of damaged human organs for transplantation.
Wu WK, Guenthart BA, O’Neill JD, Hozain AE, Tipograf Y, Ukita R, et al. Technique for xenogeneic cross-circulation to support human donor lungs ex vivo. J Heart Lung Transplant. 2023;42(3):335–44.
Sandrin MS, McKenzie IF. Gal alpha (1,3)Gal, the major xenoantigen(s) recognised in pigs by human natural antibodies. Immunol Rev. 1994;141:169–90.
Tai HC, Zhu X, Hara H, Lin YJ, Ezzelarab M, Long C, et al. The pig-to-primate immune response: relevance for xenotransplantation. Xenotransplantation. 2007;14(3):227–35.
Wu WK, Stier MT, Stokes JW, Ukita R, Patel YJ, Cortelli M, et al. Immune characterization of a xenogeneic human lung cross-circulation support system. Sci Adv. 2023;9(13):eade7647.
• Griffith BP, Goerlich CE, Singh AK, Rothblatt M, Lau CL, Shah A, et al. Genetically modified porcine-to-human cardiac xenotransplantation. N Engl J Med. 2022;387(1):35–44. This study highlights the recent success of a successful pig heart xenotransplant into a patient and marks a historic moment in the field of xenotransplantation. Furthermore, this publication highlights decades of research that allowed the development of humanized genetically modified swine, and marks a turning point for possible future xenogeneic transplants.
Lu T, Yang B, Wang R, Qin C. Xenotransplantation: current status in preclinical research. Front Immunol. 2019;10:3060.
Author information
Authors and Affiliations
Contributions
A.E.H. and R.P.J. wrote the manuscript text. A.E.H. prepared the figure. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hozain, A.E., Jablonski, R.P. Novel Strategies for Optimization of the Pre-transplant Donor Lung. Curr Pulmonol Rep (2024). https://doi.org/10.1007/s13665-024-00348-x
Accepted:
Published:
DOI: https://doi.org/10.1007/s13665-024-00348-x