Abstract
Purpose of Review
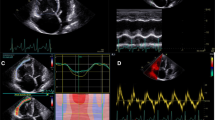
This review discusses the current limitations of assessing the right ventricle (RV) using Point-of-Care Ultrasound, explains the challenges in describing the complexity of the RV, and provides guidance on how to use Point-of-Care Ultrasound data in clinical practice.
Recent Findings
Assessing the RV requires assessments from multiple views and parameters due to its complex shape. Combined use of multiple ultrasound-derived measures along with clinical information from other sources is recommended. Artificial intelligence is increasingly used in Point-of-Care Ultrasound and will help improve validity and consistency of measurements. Future studies are needed to examine the impact of the Point-of-Care Ultrasound exam on clinical outcomes.
Summary
Multiple challenges exist in RV assessment. Future studies and guidance are required to investigate the feasibility of Point-of-Care Ultrasound in specific clinical settings, training and credentialing of examiners, and practice guidance on parameters to be used and reported.

Similar content being viewed by others
Data Availability
No datasets were generated or analysed during the current study.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Grignola JC, Domingo E. Acute right ventricular dysfunction in intensive care unit. Biomed Res Int. 2017;2017:8217105. https://doi.org/10.1155/2017/8217105.
Zhang H, Huang W, Zhang Q, Chen X, Wang X, Liu D, et al. Prevalence and prognostic value of various types of right ventricular dysfunction in mechanically ventilated septic patients. Ann Intensive Care. 2021;11(1):108. https://doi.org/10.1186/s13613-021-00902-9.
Vallabhajosyula S, Shankar A, Vojjini R, Cheungpasitporn W, Sundaragiri PR, DuBrock HM, et al. Impact of right ventricular dysfunction on short-term and long-term mortality in sepsis: a meta-analysis of 1,373 patients. Chest. 2021;159(6):2254–63. https://doi.org/10.1016/j.chest.2020.12.016.
Chotalia M, Ali M, Alderman JE, Kalla M, Parekh D, Bangash MN, et al. Right ventricular dysfunction and its association with mortality in coronavirus disease 2019 acute respiratory distress syndrome. Crit Care Med. 2021;49(10):1757–68. https://doi.org/10.1097/CCM.0000000000005167.
Coutance G, Cauderlier E, Ehtisham J, Hamon M, Hamon M. The prognostic value of markers of right ventricular dysfunction in pulmonary embolism: a meta-analysis. Crit Care. 2011;15(2):R103. https://doi.org/10.1186/cc10119.
Santas E, De la Espriella R, Chorro FJ, Palau P, Minana G, Heredia R, et al. Right ventricular dysfunction staging system for mortality risk stratification in heart failure with preserved ejection fraction. J Clin Med. 2020 Mar 18;9(3):831. https://doi.org/10.3390/jcm9030831.
• Braunwald E. Pathophysiology of heart failure. Heart disease: a textbook of cardiovascular medicine. Philadelphia: Saunders; 1980. Excellent resource to study basic cardiac physiology.
Naeije R, Manes A. The right ventricle in pulmonary arterial hypertension. Eur Respir Rev. 2014;23(134):476–87. https://doi.org/10.1183/09059180.00007414.
Lahm T, Douglas IS, Archer SL, Bogaard HJ, Chesler NC, Haddad F, et al. Assessment of right ventricular function in the research setting: knowledge gaps and pathways forward. An Official American Thoracic Society Research Statement. Am J Respir Crit Care Med. 2018;198(4):e15–43. https://doi.org/10.1164/rccm.201806-1160ST.
Haddad F, Hunt SA, Rosenthal DN, Murphy DJ. Right ventricular function in cardiovascular disease, part I: anatomy, physiology, aging, and functional assessment of the right ventricle. Circulation. 2008;117(11):1436–48. https://doi.org/10.1161/CIRCULATIONAHA.107.653576.
Kovacs A, Lakatos B, Tokodi M, Merkely B. Right ventricular mechanical pattern in health and disease: beyond longitudinal shortening. Heart Fail Rev. 2019;24(4):511–20. https://doi.org/10.1007/s10741-019-09778-1.
Addetia K, Muraru D, Badano LP, Lang RM. New directions in right ventricular assessment using 3-dimensional echocardiography. JAMA Cardiol. 2019;4(9):936–44. https://doi.org/10.1001/jamacardio.2019.2424.
Kind T, Mauritz GJ, Marcus JT, van de Veerdonk M, Westerhof N, Vonk-Noordegraaf A. Right ventricular ejection fraction is better reflected by transverse rather than longitudinal wall motion in pulmonary hypertension. J Cardiovasc Magn Reson. 2010;12(1):35. https://doi.org/10.1186/1532-429X-12-35.
• Surkova E, Kovacs A, Tokodi M, Lakatos BK, Merkely B, Muraru D, et al. Contraction patterns of the right ventricle associated with different degrees of left ventricular systolic dysfunction. Circ Cardiovasc Imaging. 2021;14(10):e012774. https://doi.org/10.1161/CIRCIMAGING.121.012774. Describes changes in RV contraction with decreasing LV function.
Lakatos B, Toser Z, Tokodi M, Doronina A, Kosztin A, Muraru D, et al. Quantification of the relative contribution of the different right ventricular wall motion components to right ventricular ejection fraction: the ReVISION method. Cardiovasc Ultrasound. 2017;15(1):8. https://doi.org/10.1186/s12947-017-0100-0.
Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing GJ, Harjola VP, et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS): The Task Force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC). Eur Respir J. 2019;54(3):1901647. https://doi.org/10.1183/13993003.01647-2019.
Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23(7):685–713; quiz 86–8. https://doi.org/10.1016/j.echo.2010.05.010.
•• Prada G, Pustavoitau A, Koenig S, Mitchell C, Stainback RF, Diaz-Gomez JL. Focused cardiac ultrasonography for right ventricular size and systolic function. N Engl J Med. 2022;387(21):e52. https://doi.org/10.1056/NEJMvcm2004089. Recent article providing guidance on RV assessment using Point-of-care Ultrasound.
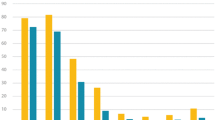
Schneider M, Aschauer S, Mascherbauer J, Ran H, Binder C, Lang I, et al. Echocardiographic assessment of right ventricular function: current clinical practice. Int J Cardiovasc Imaging. 2019;35(1):49–56. https://doi.org/10.1007/s10554-018-1428-8.
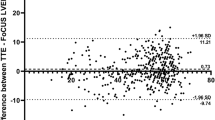
Ling LF, Obuchowski NA, Rodriguez L, Popovic Z, Kwon D, Marwick TH. Accuracy and interobserver concordance of echocardiographic assessment of right ventricular size and systolic function: a quality control exercise. J Am Soc Echocardiogr. 2012;25(7):709–13. https://doi.org/10.1016/j.echo.2012.03.018.
Bellsham-Revell HR, Simpson JM, Miller OI, Bell AJ. Subjective evaluation of right ventricular systolic function in hypoplastic left heart syndrome: how accurate is it? J Am Soc Echocardiogr. 2013;26(1):52–6. https://doi.org/10.1016/j.echo.2012.09.020.
Schneider M, Ran H, Aschauer S, Binder C, Mascherbauer J, Lang I, et al. Visual assessment of right ventricular function by echocardiography: how good are we? Int J Cardiovasc Imaging. 2019;35(11):2001–8. https://doi.org/10.1007/s10554-019-01653-2.
Tilly R, Mehrlaender M, Reichle C, Rosenberger P, Magunia H, Keller M. A one-day focused cardiac ultrasound training has a limited impact on residentsʼ abilities to visually assess right ventricular dimensions and function. Echocardiography. 2022;39(12):1481–7. https://doi.org/10.1111/echo.15461.
Zhang H, He W, Wang X, Chao Y, Zhang L, Zhu R, et al. Physiciansʼ ability to visually estimate left ventricular ejection fraction, right ventricular enlargement, and paradoxical septal motion after a 2-day focused cardiac ultrasound training course. J Cardiothorac Vasc Anesth. 2019;33(7):1912–8. https://doi.org/10.1053/j.jvca.2018.10.019.
Cecconi M, De Backer D, Antonelli M, Beale R, Bakker J, Hofer C, et al. Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of Intensive Care Medicine. Intensive Care Med. 2014;40(12):1795–815. https://doi.org/10.1007/s00134-014-3525-z.
Jaff MR, McMurtry MS, Archer SL, Cushman M, Goldenberg N, Goldhaber SZ, et al. Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American Heart Association. Circulation. 2011;123(16):1788–830. https://doi.org/10.1161/CIR.0b013e318214914f.
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28(1):1-39 e14. https://doi.org/10.1016/j.echo.2014.10.003.
Hadad Y, Iluz M, Ziv-Baran T, Shalmon T, Rozenbaum Z, Berliner S, et al. High prevalence of right ventricular/left ventricular ratio >/=1 among patients undergoing computed tomography pulmonary angiography. J Thorac Imaging. 2021;36(4):231–5. https://doi.org/10.1097/RTI.0000000000000547.
Altmayer SPL, Han QJ, Addetia K, Patel AR, Forfia PR, Han Y. Using all-cause mortality to define severe RV dilation with RV/LV volume ratio. Sci Rep. 2018;8(1):7200. https://doi.org/10.1038/s41598-018-25259-1.
Fremont B, Pacouret G, Jacobi D, Puglisi R, Charbonnier B, de Labriolle A. Prognostic value of echocardiographic right/left ventricular end-diastolic diameter ratio in patients with acute pulmonary embolism: results from a monocenter registry of 1,416 patients. Chest. 2008;133(2):358–62. https://doi.org/10.1378/chest.07-1231.
Pruszczyk P, Kurnicka K, Ciurzynski M, Hobohm L, Thielmann A, Sobkowicz B, et al. Defining right ventricular dysfunction by echocardiography in normotensive patients with pulmonary embolism. Pol Arch Intern Med. 2020;130(9):741–7. https://doi.org/10.20452/pamw.15459.
Cimini LA, Candeloro M, Plywaczewska M, Maraziti G, Di Nisio M, Pruszczyk P, et al. Prognostic role of different findings at echocardiography in acute pulmonary embolism: a critical review and meta-analysis. ERJ Open Res. 2023;9(2):00641–2022. https://doi.org/10.1183/23120541.00641-2022.
Ammari Z, Hasnie AA, Ruzieh M, Dasa O, Al-Sarie M, Shastri P, et al. Prognostic value of computed tomography versus echocardiography derived right to left ventricular diameter ratio in acute pulmonary embolism. Am J Med Sci. 2021;361(4):445–50. https://doi.org/10.1016/j.amjms.2020.07.008.
Tang A, Hunsaker A, Hammer M. Significance of right-to-left ventricular ratio as a quantitative computed tomography biomarker in patients with negative computed tomography pulmonary angiograms. J Thorac Imaging. 2022;37(3):181–6. https://doi.org/10.1097/RTI.0000000000000630.
Cote B, Jimenez D, Planquette B, Roche A, Marey J, Pastre J, et al. Prognostic value of right ventricular dilatation in patients with low-risk pulmonary embolism. Eur Respir J. 2017;50(6):1701611. https://doi.org/10.1183/13993003.01611-2017.
Ayoz S, Erol S, Kul M, Gurun Kaya A, Gursoy Coruh A, Savas I, et al. Using RV/LV ratio and cardiac biomarkers to define the risk of mortality from pulmonary embolism. Tuberk Toraks. 2021;69(3):297–306. https://doi.org/10.5578/tt.20219701.
Bax S, Jacob J, Ahmed R, Bredy C, Dimopoulos K, Kempny A, et al. Right ventricular to left ventricular ratio at CT pulmonary angiogram predicts mortality in interstitial lung disease. Chest. 2020;157(1):89–98. https://doi.org/10.1016/j.chest.2019.06.033.
Cirulis MM, Huston JH, Sardar P, Suksaranjit P, Wilson BD, Hatton ND, et al. Right-to-left ventricular end diastolic diameter ratio in severe sepsis and septic shock. J Crit Care. 2018;48:307–10. https://doi.org/10.1016/j.jcrc.2018.09.025.
Galderisi M, Cosyns B, Edvardsen T, Cardim N, Delgado V, Di Salvo G, et al. Standardization of adult transthoracic echocardiography reporting in agreement with recent chamber quantification, diastolic function, and heart valve disease recommendations: an expert consensus document of the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2017;18(12):1301–10. https://doi.org/10.1093/ehjci/jex244.
Claessen G, Claus P, Delcroix M, Bogaert J, La Gerche A, Heidbuchel H. Interaction between respiration and right versus left ventricular volumes at rest and during exercise: a real-time cardiac magnetic resonance study. Am J Physiol Heart Circ Physiol. 2014;306(6):H816–24. https://doi.org/10.1152/ajpheart.00752.2013.
Jiang L, Levine RA, Weyman AE. Echocardiographic assessment of right ventricular volume and function. Echocardiography. 1997;14(2):189–206. https://doi.org/10.1111/j.1540-8175.1997.tb00711.x.
Norgard G, Vik-Mo H. Effects of respiration on right ventricular size and function: an echocardiographic study. Pediatr Cardiol. 1992;13(3):136–40. https://doi.org/10.1007/BF00793944.
Ryan T, Petrovic O, Dillon JC, Feigenbaum H, Conley MJ, Armstrong WF. An echocardiographic index for separation of right ventricular volume and pressure overload. J Am Coll Cardiol. 1985;5(4):918–27. https://doi.org/10.1016/s0735-1097(85)80433-2.
King ME, Braun H, Goldblatt A, Liberthson R, Weyman AE. Interventricular septal configuration as a predictor of right ventricular systolic hypertension in children: a cross-sectional echocardiographic study. Circulation. 1983;68(1):68–75. https://doi.org/10.1161/01.cir.68.1.68.
Dasgupta S, Richardson JC, Aly AM, Jain SK. Role of functional echocardiographic parameters in the diagnosis of bronchopulmonary dysplasia-associated pulmonary hypertension. J Perinatol. 2022;42(1):19–30. https://doi.org/10.1038/s41372-021-01009-6.
Howard LS, Grapsa J, Dawson D, Bellamy M, Chambers JB, Masani ND, et al. Echocardiographic assessment of pulmonary hypertension: standard operating procedure. Eur Respir Rev. 2012;21(125):239–48. https://doi.org/10.1183/09059180.00003912.
Badano LP, Ginghina C, Easaw J, Muraru D, Grillo MT, Lancellotti P, et al. Right ventricle in pulmonary arterial hypertension: haemodynamics, structural changes, imaging, and proposal of a study protocol aimed to assess remodelling and treatment effects. Eur J Echocardiogr. 2010;11(1):27–37. https://doi.org/10.1093/ejechocard/jep152.
Wang L, Chen X, Wan K, Gong C, Li W, Xu Y, et al. Diagnostic and prognostic value of right ventricular eccentricity index in pulmonary artery hypertension. Pulm Circ. 2020;10(2):2045894019899778. https://doi.org/10.1177/2045894019899778.
D’Alto M, Romeo E, Argiento P, Pavelescu A, Melot C, D’Andrea A, et al. Echocardiographic prediction of pre- versus postcapillary pulmonary hypertension. J Am Soc Echocardiogr. 2015;28(1):108–15. https://doi.org/10.1016/j.echo.2014.09.004.
Haddad F, Guihaire J, Skhiri M, Denault AY, Mercier O, Al-Halabi S, et al. Septal curvature is marker of hemodynamic, anatomical, and electromechanical ventricular interdependence in patients with pulmonary arterial hypertension. Echocardiography. 2014;31(6):699–707. https://doi.org/10.1111/echo.12468.
Teng WH, McCall PJ, Shelley BG. The utility of eccentricity index as a measure of the right ventricular function in a lung resection cohort. J Cardiovasc Echogr. 2019;29(3):103–10. https://doi.org/10.4103/jcecho.jcecho_19_19.
Raymond RJ, Hinderliter AL, Willis PW, Ralph D, Caldwell EJ, Williams W, et al. Echocardiographic predictors of adverse outcomes in primary pulmonary hypertension. J Am Coll Cardiol. 2002;39(7):1214–9. https://doi.org/10.1016/s0735-1097(02)01744-8.
Anavekar NS, Gerson D, Skali H, Kwong RY, Yucel EK, Solomon SD. Two-dimensional assessment of right ventricular function: an echocardiographic-MRI correlative study. Echocardiography. 2007;24(5):452–6. https://doi.org/10.1111/j.1540-8175.2007.00424.x.
Kaul S, Tei C, Hopkins JM, Shah PM. Assessment of right ventricular function using two-dimensional echocardiography. Am Heart J. 1984;107(3):526–31. https://doi.org/10.1016/0002-8703(84)90095-4.
Mertens LL, Friedberg MK. Imaging the right ventricle–current state of the art. Nat Rev Cardiol. 2010;7(10):551–63. https://doi.org/10.1038/nrcardio.2010.118.
Nesser HJ, Tkalec W, Patel AR, Masani ND, Niel J, Markt B, et al. Quantitation of right ventricular volumes and ejection fraction by three-dimensional echocardiography in patients: comparison with magnetic resonance imaging and radionuclide ventriculography. Echocardiography. 2006;23(8):666–80. https://doi.org/10.1111/j.1540-8175.2006.00286.x.
Aune E, Baekkevar M, Rodevand O, Otterstad JE. The limited usefulness of real-time 3-dimensional echocardiography in obtaining normal reference ranges for right ventricular volumes. Cardiovasc Ultrasound. 2009;7:35. https://doi.org/10.1186/1476-7120-7-35.
Zornoff LA, Skali H, Pfeffer MA, St John Sutton M, Rouleau JL, Lamas GA, et al. Right ventricular dysfunction and risk of hear failure and mortality after myocardial infarction. J Am Coll Cardiol. 2002;39(9):1450–5. https://doi.org/10.1016/s0735-1097(02)01804-1.
Anavekar NS, Skali H, Bourgoun M, Ghali JK, Kober L, Maggioni AP, et al. Usefulness of right ventricular fractional area change to predict death, heart failure, and stroke following myocardial infarction (from the VALIANT ECHO Study). Am J Cardiol. 2008;101(5):607–12. https://doi.org/10.1016/j.amjcard.2007.09.115.
Antoni ML, Scherptong RW, Atary JZ, Boersma E, Holman ER, van der Wall EE, et al. Prognostic value of right ventricular function in patients after acute myocardial infarction treated with primary percutaneous coronary intervention. Circ Cardiovasc Imaging. 2010;3(3):264–71. https://doi.org/10.1161/CIRCIMAGING.109.914366.
Ghio S, Gavazzi A, Campana C, Inserra C, Klersy C, Sebastiani R, et al. Independent and additive prognostic value of right ventricular systolic function and pulmonary artery pressure in patients with chronic heart failure. J Am Coll Cardiol. 2001;37(1):183–8. https://doi.org/10.1016/s0735-1097(00)01102-5.
Gorter TM, Hoendermis ES, van Veldhuisen DJ, Voors AA, Lam CS, Geelhoed B, et al. Right ventricular dysfunction in heart failure with preserved ejection fraction: a systematic review and meta-analysis. Eur J Heart Fail. 2016;18(12):1472–87. https://doi.org/10.1002/ejhf.630.
Okada DR, Rahmouni HW, Herrmann HC, Bavaria JE, Forfia PR, Han Y. Assessment of right ventricular function by transthoracic echocardiography following aortic valve replacement. Echocardiography. 2014;31(5):552–7. https://doi.org/10.1111/echo.12421.
Calvin JE Jr. Pressure segment length analysis of right ventricular function: influence of loading conditions. Am J Physiol. 1991;260(4 Pt 2):H1087–97. https://doi.org/10.1152/ajpheart.1991.260.4.H1087.
McConnell MV, Solomon SD, Rayan ME, Come PC, Goldhaber SZ, Lee RT. Regional right ventricular dysfunction detected by echocardiography in acute pulmonary embolism. Am J Cardiol. 1996;78(4):469–73. https://doi.org/10.1016/s0002-9149(96)00339-6.
Casazza F, Bongarzoni A, Capozi A, Agostoni O. Regional right ventricular dysfunction in acute pulmonary embolism and right ventricular infarction. Eur J Echocardiogr. 2005;6(1):11–4. https://doi.org/10.1016/j.euje.2004.06.002.
Fields JM, Davis J, Girson L, Au A, Potts J, Morgan CJ, et al. Transthoracic echocardiography for diagnosing pulmonary embolism: a systematic review and meta-analysis. J Am Soc Echocardiogr. 2017;30(7):714-23 e4. https://doi.org/10.1016/j.echo.2017.03.004.
Kjaergaard J, Schaadt BK, Lund JO, Hassager C. Quantification of right ventricular function in acute pulmonary embolism: relation to extent of pulmonary perfusion defects. Eur J Echocardiogr. 2008;9(5):641–5. https://doi.org/10.1093/ejechocard/jen033.
Forfia PR, Fisher MR, Mathai SC, Housten-Harris T, Hemnes AR, Borlaug BA, et al. Tricuspid annular displacement predicts survival in pulmonary hypertension. Am J Respir Crit Care Med. 2006;174(9):1034–41. https://doi.org/10.1164/rccm.200604-547OC.
Martha JW, Pranata R, Wibowo A, Lim MA. Tricuspid annular plane systolic excursion (TAPSE) measured by echocardiography and mortality in COVID-19: a systematic review and meta-analysis. Int J Infect Dis. 2021;105:351–6. https://doi.org/10.1016/j.ijid.2021.02.029.
Lobo JL, Holley A, Tapson V, Moores L, Oribe M, Barron M, et al. Prognostic significance of tricuspid annular displacement in normotensive patients with acute symptomatic pulmonary embolism. J Thromb Haemost. 2014;12(7):1020–7. https://doi.org/10.1111/jth.12589.
Aceituno-Melgar JE, Posada-Martinez EL. Focused cardiac ultrasonography for right ventricular size and systolic function. N Engl J Med. 2023;388(12):1149–50. https://doi.org/10.1056/NEJMc2300338.
Surkova E, Cosyns B, Gerber B, Gimelli A, La Gerche A, Ajmone MN. The dysfunctional right ventricle: the importance of multi-modality imaging. Eur Heart J Cardiovasc Imaging. 2022;23(7):885–97. https://doi.org/10.1093/ehjci/jeac037.
• Le MT, Voigt L, Nathanson R, Maw AM, Johnson G, Dancel R, et al. Comparison of four handheld point-of-care ultrasound devices by expert users. Ultrasound J. 2022;14(1):27. https://doi.org/10.1186/s13089-022-00274-6. Practical paper comparing 4 different handheld Point-of-care Ultrasound device.
Jordan MI, Mitchell TM. Machine learning: trends, perspectives, and prospects. Science. 2015;349(6245):255–60. https://doi.org/10.1126/science.aaa8415.
Barry T, Farina JM, Chao CJ, Ayoub C, Jeong J, Patel BN, et al. The role of artificial intelligence in echocardiography. J Imaging. 2023;9(2):50. https://doi.org/10.3390/jimaging9020050.
EchoNous: Kosmos Ultraportable Ultrasound. https://echonous.com/product/kosmos-ultraportable-ultrasound/. Accessed 23 Jan 2024.
Baum E, Tandel MD, Ren C, Weng Y, Pascucci M, Kugler J, et al. Acquisition of cardiac point-of-care ultrasound images with deep learning a randomized trial for educational outcomes with novices. CHEST Pulmonary. 2023;1(3):100023. https://doi.org/10.1016/j.chpulm.2023.100023.
Hsia BC, Lai A, Singh S, Samtani R, Bienstock S, Liao S, et al. Validation of American Society of Echocardiography Guideline-recommended parameters of right ventricular dysfunction using artificial intelligence compared with cardiac magnetic resonance imaging. J Am Soc Echocardiogr. 2023;36(9):967–77. https://doi.org/10.1016/j.echo.2023.05.015.
Tokodi M, Magyar B, Soos A, Takeuchi M, Tolvaj M, Lakatos BK, et al. Deep learning-based prediction of right ventricular ejection fraction using 2D echocardiograms. JACC Cardiovasc Imaging. 2023;16(8):1005–18. https://doi.org/10.1016/j.jcmg.2023.02.017.
•• Kirkpatrick JN, Grimm R, Johri AM, Kimura BJ, Kort S, Labovitz AJ, et al. Recommendations for echocardiography laboratories participating in cardiac point of care cardiac ultrasound (POCUS) and critical care echocardiography training: report from the American Society of Echocardiography. J Am Soc Echocardiogr. 2020;33(4):409-22 e4. https://doi.org/10.1016/j.echo.2020.01.008. Guideline of Point-of-care Ultrasound training.
Huang GS, Alviar CL, Wiley BM, Kwon Y. The era of point-of-care ultrasound has arrived: are cardiologists ready? Am J Cardiol. 2020;132:173–5. https://doi.org/10.1016/j.amjcard.2020.06.062.
Butterfly Network, Inc: Butterfly for Individuals Seeing is knowing. Patient assessment, transformed. https://www.butterflynetwork.com/iq-ultrasound-individuals. Accessed 23 Jan 2024.
Clarius Ultrasound Scanner - HD3 Scanners User Manual. 2023. https://support.clarius.com/hc/article_attachments/20287469196692. Accessed 23 Jan 2024.
Wellbin Technology Co. L: Transforming Point-of-Care with Unparalleled Mobility: EagleView Wireless Probe Type Ultrasound Scanner. https://geteagleview.com/products/dual-head-wireless-handheld-ultrasound?currency=USD. Accessed 23 Jan 2024.
Philips: Exceptional ultrasound capabilities in the palm of your hand. https://www.usa.philips.com/healthcare/sites/lumify-handheld-ultrasound. Accessed 23 Jan 2024.
Mindray North America: TE Air Wireless Handheld Ultrasound. https://m9m2s9g3.rocketcdn.me/wp-content/uploads/2023/05/TE-Air-Launch-Brochure_6pg_FA-to-CR.pdf. Accessed 23 Jan 2024
Dr.Sono: Tri-Scan Max Portable Ultrasound Scanner. https://drsono.com/product/tri-scan-max/. Accessed 23 Jan 2024.
Inc. VH: Vave Wireless Ultrasound User Manual. 2021. https://vavehealth.com/wp-content/uploads/2021/01/Vave-Health-User-Guide.pdf. Accessed 23 Jan 2024.
GE HealthCare: Vscan Air™ SL. https://handheldultrasound.gehealthcare.com/vscan-air-cl/. Accessed 22 Jan 2024.
Author information
Authors and Affiliations
Contributions
I.I. and M.K. drafted the manuscript. All authors reviewed and provided critical comments and suggestions. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
II receives a research grant from the American Academy of Sleep Medicine Foundation. TY is a Pulmonologist and Intensivist in Pulmonary, Critical Care Medicine at Jesse Brown VA Medical Center, Chicago, IL. MK is a Cardiologist in the Division of Cardiology at the University of Illinois at Chicago and the Jesse Brown VA Medical Center, Chicago, IL.
Human and Animal Rights and Informed Consent
This article does not contain any studies of human or animal subjects performed by any of the authors.
Disclaimer
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Imayama, I., Yamanaka, T., Ascoli, C. et al. Challenges in Grading the Severity of Right Ventricular Dysfunction via Point-of-Care Echocardiography. Curr Pulmonol Rep (2024). https://doi.org/10.1007/s13665-024-00346-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s13665-024-00346-z