Abstract
Purpose of Review
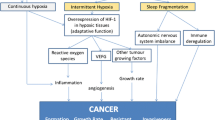
Obstructive sleep apnea (OSA) has been investigated the most within the spectrum of sleep-related breathing disorders in cancer. The purpose of this review is to describe the biological pathways and review the epidemiological studies regarding OSA and cancer, and to additionally explore the spectrum of sleep-related breathing disorders in cancer.
Recent Findings
Murine models have elucidated intermittent hypoxia and sleep fragmentation as oncogenic, and large epidemiologic studies have identified increased cancer incidence among those with OSA and hypoxemia. Central sleep apnea (CSA) may develop in those using opioids for pain control. Sleep-related hypoventilation should be considered in those with underlying pulmonary dysfunction, vocal cord abnormalities, and neuromuscular weakness.
Summary
Cancer patients are at risk of developing sleep-related breathing disorders in the form of OSA, CSA, or sleep-related hypoventilation. The impact of sleep-related breathing disorders on cancer may have ramifications for the prevention and treatment of cancer.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Stepanski E, Burgess HJ. Sleep and cancer. Sleep medicine clinics. 2007;2:67–75.
Davidson JR, MacLean AW, Brundage MD, Schulze K. Sleep disturbance in cancer patients. Soc Sci Med. 2002;54:1309–21.
Erren TC. Re: “Self-reported sleep duration, sleep quality, and breast cancer risk in a population-based case-control study”. Am J Epidemiol. 2013;177:1020–1.
Erren TC, Morfeld P. Shift work and cancer research: a thought experiment into a potential chronobiological fallacy of past and perspectives for future epidemiological studies. Neuro endocrinology letters. 2013;34:282–6.
Erren TC, Morfeld P, Foster RG, Reiter RJ, Gross JV, Westermann IK. Sleep and cancer: synthesis of experimental data and meta-analyses of cancer incidence among some 1,500,000 study individuals in 13 countries. Chronobiol Int. 2016;33:325–50.
Ma QQ, Yao Q, Lin L, Chen GC, Yu JB. Sleep duration and total cancer mortality: a meta-analysis of prospective studies. Sleep Med. 2016;27-28:39–44.
• Balachandran DD, Faiz S, Bashoura L, Manzullo E. Cancer-related fatigue and sleep disorders. Sleep medicine clinics. 2013;8:229–34. Reviews the etiology and management of cancer-related fatigue and examine role of sleep disorders in this debilitating cancer-related symptom
Fortner BV, Stepanski EJ, Wang SC, Kasprowicz S, Durrence HH. Sleep and quality of life in breast cancer patients. J Pain Symptom Manag. 2002;24:471–80.
Opp MR. Sleep and psychoneuroimmunology. Immunol Allergy Clin N Am. 2009;29:295–307.
Payne JK, Piper BF, Rabinowitz I, Zimmerman MB. Biomarkers, fatigue, sleep, and depressive symptoms in women with breast cancer: a pilot study. Oncol Nurs Forum. 2006;33:775–83.
Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, Daniels S, Floras JS, Hunt CE, Olson LJ, Pickering TG, Russell R, Woo M, Young T. Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation scientific statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. J Am Coll Cardiol. 2008;52:686–717.
Unnikrishnan D, Jun J, Polotsky V. Inflammation in sleep apnea: an update. Rev Endocr Metab Disord. 2015;16:25–34.
May AM, Mehra R. Obstructive sleep apnea: role of intermittent hypoxia and inflammation. Semin Respir Crit Care Med. 2014;35:531–44.
Berry RB BR, Gamaldo CE, Harding SM, Lloyd RM, Marcus CL and Vaughn BV for the American Academy of Sleep Medicine. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications, Version 2.3. www.aasmnet.org. Darien, Illinois: American Academy of Sleep Medicine; 2016.
Malhotra A, Owens RL. What is central sleep apnea? Respir Care. 2010;55:1168–78.
Orr JE, Malhotra A, Sands SA. Pathogenesis of central and complex sleep apnoea. Respirology (Carlton, Vic). 2017;22:43–52.
Faiz SA, Bashoura L, Kodali L, Hessel AC, Evans SE, Balachandran DD. Sleep-disordered breathing as a delayed complication of iatrogenic vocal cord trauma. Sleep Med. 2016;22:1–3.
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–5.
Cai A, Wang L, Zhou Y. Hypertension and obstructive sleep apnea. Hypertension research : official journal of the Japanese Society of Hypertension. 2016;39:391–5.
Sajkov D, McEvoy RD. Obstructive sleep apnea and pulmonary hypertension. Prog Cardiovasc Dis. 2009;51:363–70.
Wong JK, Mariano ER, Doufas AG, Olejniczak MJ, Kushida CA. Preoperative treatment of obstructive sleep apnea with positive airway pressure is associated with decreased incidence of atrial fibrillation after cardiac surgery. J Cardiothorac Vasc Anesth. 2016; doi:10.1053/j.jvca.2016.11.016.
Tung Md P, Anter ME. Atrial fibrillation and sleep apnea: considerations for a dual epidemic. J Atr Fibrillation. 2016;8:1283.
Goyal SK, Sharma A. Atrial fibrillation in obstructive sleep apnea. World J Cardiol. 2013;5:157–63.
Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, Daniels S, Floras JS, Hunt CE, Olson LJ, Pickering TG, Russell R, Woo M, Young T. American Heart Association Council for High Blood Pressure Research Professional Education Committee CoCC, American Heart Association Stroke C, American Heart Association Council on Cardiovascular N, American College of Cardiology F. Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology foundation scientific statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). Circulation. 2008;118:1080–111.
Lyons OD, Ryan CM. Sleep apnea and stroke. Can J Cardiol. 2015;31:918–27.
Gao ZH, Yuan RY, Chen KY, Li GP. Obstructive sleep apnea and the metabolic syndrome. Sleep & breathing = Schlaf & Atmung. 2012;16:937–8.
Chen L, Kuang J, Pei JH, Chen HM, Chen Z, Li ZW, Yang HZ, Fu XY, Wang L, Chen ZJ, Lai SQ, Zhang ST. Continuous positive airway pressure and diabetes risk in sleep apnea patients: a systemic review and meta-analysis. Eur J Intern Med 2016.
Iftikhar IH, Hoyos CM, Phillips CL, Magalang UJ. Meta-analyses of the Association of Sleep Apnea with insulin resistance, and the effects of CPAP on HOMA-IR, adiponectin, and visceral adipose fat. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2015;11:475–85.
American Society of Anesthesiologists Task Force on Perioperative Management of patients with obstructive sleep apnea. Practice guidelines for the perioperative management of patients with obstructive sleep apnea: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Management of patients with obstructive sleep apnea. Anesthesiology 2014; 120: 268–286.
Joshi GP, Ankichetty SP, Gan TJ, Chung F. Society for Ambulatory Anesthesia consensus statement on preoperative selection of adult patients with obstructive sleep apnea scheduled for ambulatory surgery. Anesth Analg. 2012;115:1060–8.
Adesanya AO, Lee W, Greilich NB, Joshi GP. Perioperative management of obstructive sleep apnea. Chest. 2010;138:1489–98.
Memtsoudis SG, Besculides MC, Mazumdar M. A rude awakening—the perioperative sleep apnea epidemic. N Engl J Med. 2013;368:2352–3.
Vaessen TJ, Overeem S, Sitskoorn MM. Cognitive complaints in obstructive sleep apnea. Sleep Med Rev. 2015;19:51–8.
Ejaz SM, Khawaja IS, Bhatia S, Hurwitz TD. Obstructive sleep apnea and depression: a review. Innov Clin Neurosci. 2011;8:17–25.
Garbarino S, Durando P, Guglielmi O, Dini G, Bersi F, Fornarino S, Toletone A, Chiorri C, Magnavita N. Sleep apnea, sleep debt and daytime sleepiness are independently associated with road accidents. A cross-sectional study on truck drivers. PLoS One. 2016;11:e0166262.
Kales SN, Czeisler CA. Obstructive sleep apnea and work accidents: time for action. Sleep. 2016;39:1171–3.
Garbarino S, Guglielmi O, Sanna A, Mancardi GL, Magnavita N. Risk of occupational accidents in workers with obstructive sleep apnea: systematic review and meta-analysis. Sleep. 2016;39:1211–8.
Gurubhagavatula I, Patil S, Meoli A, Olson R, Sullivan S, Berneking M, Watson NF. Sleep apnea evaluation of commercial motor vehicle operators. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2015;12:285–6.
Gozal D, Farre R, Nieto FJ. Putative links between sleep apnea and cancer: from hypotheses to evolving evidence. Chest. 2015;148:1140–7.
Gozal D, Farre R, Nieto FJ. Obstructive sleep apnea and cancer: epidemiologic links and theoretical biological constructs. Sleep Med Rev. 2016;27:43–55.
Almendros I, Montserrat JM, Torres M, Bonsignore MR, Chimenti L, Navajas D, Farre R. Obesity and intermittent hypoxia increase tumor growth in a mouse model of sleep apnea. Sleep Med. 2012;13:1254–60.
•• Almendros I, Montserrat JM, Ramirez J, Torres M, Duran-Cantolla J, Navajas D, Farre R. Intermittent hypoxia enhances cancer progression in a mouse model of sleep apnoea. Eur Respir J. 2012;39:215–7. This study provides a thorough description of the role of IH in cancer genesis
Kaczmarek E, Bakker JP, Clarke DN, Csizmadia E, Kocher O, Veves A, Tecilazich F, O'Donnell CP, Ferran C, Malhotra A. Molecular biomarkers of vascular dysfunction in obstructive sleep apnea. PLoS One. 2013;8:e70559.
Saloman JL, Albers KM, Rhim AD, Davis BM. Can stopping nerves, stop cancer? Trends Neurosci. 2016;39:880–9.
Magnon C. Role of the autonomic nervous system in tumorigenesis and metastasis. Molecular & cellular oncology. 2015;2:e975643.
•• Campos-Rodriguez F, Martinez-Garcia MA, Martinez M, Duran-Cantolla J, Pena Mde L, Masdeu MJ, Gonzalez M, Campo F, Gallego I, Marin JM, Barbe F, Montserrat JM, Farre R, Spanish Sleep N. Association between obstructive sleep apnea and cancer incidence in a large multicenter Spanish cohort. Am J Respir Crit Care Med. 2013;187:99–105. First study to examine the relationship between OSA and cancer incidence
Christensen AS, Clark A, Salo P, Nymann P, Lange P, Prescott E, Rod NH. Symptoms of sleep disordered breathing and risk of cancer: a prospective cohort study. Sleep. 2013;36:1429–35.
Kendzerska T, Leung RS, Hawker G, Tomlinson G, Gershon AS. Obstructive sleep apnea and the prevalence and incidence of cancer. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne. 2014;186:985–92.
Chang WP, Liu ME, Chang WC, Yang AC, Ku YC, Pai JT, Lin YW, Tsai SJ. Sleep apnea and the subsequent risk of breast cancer in women: a nationwide population-based cohort study. Sleep Med. 2014;15:1016–20.
Chen JC, Hwang JH. Sleep apnea increased incidence of primary central nervous system cancers: a nationwide cohort study. Sleep Med. 2014;15:749–54.
Gozal D, Ham SA, Mokhlesi B. Sleep apnea and cancer: analysis of a nationwide population sample. Sleep. 2016;39:1493–500.
•• Nieto FJ, Peppard PE, Young T, Finn L, Hla KM, Farre R. Sleep-disordered breathing and cancer mortality: results from the Wisconsin Sleep Cohort Study. Am J Respir Crit Care Med. 2012;186:190–4. First study to examine the correlation between OSA and cancer mortality
Martinez-Garcia MA, Campos-Rodriguez F, Duran-Cantolla J, de la Pena M, Masdeu MJ, Gonzalez M, Del Campo F, Serra PC, Valero-Sanchez I, Ferrer MJ, Marin JM, Barbe F, Martinez M, Farre R, Montserrat JM, Spanish SN. Obstructive sleep apnea is associated with cancer mortality in younger patients. Sleep Med. 2014;15:742–8.
Correa D, Farney RJ, Chung F, Prasad A, Lam D, Wong J. Chronic opioid use and central sleep apnea: a review of the prevalence, mechanisms, and perioperative considerations. Anesth Analg. 2015;120:1273–85.
• Van Ryswyk E, Antic NA. Opioids and sleep-disordered breathing. Chest. 2016;150:934–44. Excellent review of SRBD associated with opiod use
Ramar K, Ramar P, Morgenthaler TI. Adaptive servoventilation in patients with central or complex sleep apnea related to chronic opioid use and congestive heart failure. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2012;8:569–76.
Cowie MR, Woehrle H, Wegscheider K, Angermann C, d'Ortho MP, Erdmann E, Levy P, Simonds AK, Somers VK, Zannad F, Teschler H. Adaptive servo-ventilation for central sleep apnea in systolic heart failure. N Engl J Med. 2015;373:1095–105.
Tsai SC. Chronic obstructive pulmonary disease and sleep related disorders. Current opinion in pulmonary medicine 2016.
Payne RJ, Hier MP, Kost KM, Black MJ, Zeitouni AG, Frenkiel S, Naor N, Kimoff RJ. High prevalence of obstructive sleep apnea among patients with head and neck cancer. J Otolaryngol. 2005;34:304–11.
Friedman M, Landsberg R, Pryor S, Syed Z, Ibrahim H, Caldarelli DD. The occurrence of sleep-disordered breathing among patients with head and neck cancer. Laryngoscope. 2001;111:1917–9.
•• Faiz SA, Balachandran D, Hessel AC, Lei X, Beadle BM, William Jr WN, Bashoura L. Sleep-related breathing disorders in patients with tumors in the head and neck region. Oncologist. 2014;19:1200–6. Describes the incidence of SRBD in the largest population of patients with head and neck cancer
Martinez-Garcia MA, Martorell-Calatayud A, Nagore E, Valero I, Selma MJ, Chiner E, Landete P, Montserrat JM, Carrera C, Perez-Gil A, Campos-Rodriguez F, Farre R. Association between sleep disordered breathing and aggressiveness markers of malignant cutaneous melanoma. Eur Respir J. 2014;43:1661–8.
Knox ABD, Murphy VC, Bashoura L, Faiz SA. Sleep disorders in breast cancer patients based on polysomnographic data. Am J Respir Crit Care Med. 2016;193:A4183.
Grunstein RR, Ho KY, Berthon-Jones M, Stewart D, Sullivan CE. Central sleep apnea is associated with increased ventilatory response to carbon dioxide and hypersecretion of growth hormone in patients with acromegaly. Am J Respir Crit Care Med. 1994;150:496–502.
van Haute FR, Taboada GF, Correa LL, Lima GA, Fontes R, Riello AP, Dominici M, Gadelha MR. Prevalence of sleep apnea and metabolic abnormalities in patients with acromegaly and analysis of cephalometric parameters by magnetic resonance imaging. Eur J Endocrinol. 2008;158:459–65.
Fatti LM, Scacchi M, Pincelli AI, Lavezzi E, Cavagnini F. Prevalence and pathogenesis of sleep apnea and lung disease in acromegaly. Pituitary. 2001;4:259–62.
Potter A, Faiz SA, Lopez-Mattei J, Balachandran D. Sleep disordered breathing in multiple myeloma. Chest. 2016;150:1275A.
Fortner RT, Katzke V, Kuhn T, Kaaks R. Obesity and breast cancer. Recent results in cancer research Fortschritte der Krebsforschung Progres dans les recherches sur le cancer. 2016;208:43–65.
Jiralerspong S, Goodwin PJ. Obesity and breast cancer prognosis: evidence, challenges, and opportunities. J Clin Oncol. 2016;34:4203–16.
Webb PM. Obesity and gynecologic cancer etiology and survival. Am Soc Clin Oncol Educ Book 2013.
Mendonca F, Soares R. Obesity and cancer phenotype: is angiogenesis a missed link? Life Sci. 2015;139:16–23.
Chung F, Yegneswaran B, Liao P, Chung SA, Vairavanathan S, Islam S, Khajehdehi A, Shapiro CM. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108:812–21.
Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5.
Buysse DJ, Reynolds 3rd CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213.
Mendoza TR, Wang XS, Cleeland CS, Morrissey M, Johnson BA, Wendt JK, Huber SL. The rapid assessment of fatigue severity in cancer patients: use of the Brief Fatigue Inventory. Cancer. 1999;85:1186–96.
Chung F, Chau E, Yang Y, Liao P, Hall R, Mokhlesi B. Serum bicarbonate level improves specificity of STOP-Bang screening for obstructive sleep apnea. Chest. 2013;143:1284–93.
Chung F, Abdullah HR, Liao P. STOP-Bang questionnaire: a practical approach to screen for obstructive sleep apnea. Chest. 2016;149:631–8.
Balachandran DD, Faiz SA, Hernandez M, Kowalski AM, Bashoura L, Goravanchi F, Cherian SV, Rebello E, Kee SS, French KE. Length of stay in ambulatory surgical oncology patients at high risk for sleep apnea as predicted by STOP-BANG questionnaire. Anesthesiology research and practice. 2016;2016:9425936.
Cooksey JA, Balachandran JS. Portable monitoring for the diagnosis of OSA. Chest. 2016;149:1074–81.
Kuzniar TJ. New approaches to positive airway pressure treatment in obstructive sleep apnea. Sleep medicine clinics. 2016;11:153–9.
Palesh OG, Roscoe JA, Mustian KM, Roth T, Savard J, Ancoli-Israel S, Heckler C, Purnell JQ, Janelsins MC, Morrow GR. Prevalence, demographics, and psychological associations of sleep disruption in patients with cancer: University of Rochester Cancer Center-Community Clinical Oncology Program. J Clin Oncol. 2010;28:292–8.
Armstrong TS, Shade MY, Breton G, Gilbert MR, Mahajan A, Scheurer ME, Vera E, Berger AM. Sleep-wake disturbance in patients with brain tumors. Neuro Oncol 2016.
Acknowledgements
Thanks to Dr. George Eapen for commissioning and reviewing this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
L.B., S.F., and D.B. declare no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Funding
This research is supported in part by the National Institutes of Health through MD Anderson’s Cancer Center Support Grant (CA016672).
Additional information
This article is part of the Topical Collection on Sleeping and Breathing
Rights and permissions
About this article
Cite this article
Balachandran, D.D., Bashoura, L. & Faiz, S.A. Sleep-Related Breathing Disorders and Cancer. Curr Pulmonol Rep 6, 90–101 (2017). https://doi.org/10.1007/s13665-017-0182-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13665-017-0182-z