Abstract
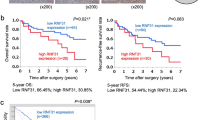
Hepatocellular carcinoma (HCC) is one of the malignant tumors with the worst prognosis, and tumor recurrence and metastasis are the main factors leading to poor prognosis of HCC patients. Accumulating studies show that RNF126, ring finger protein 126, is involved in the pathological process of many tumors. However, the biological function and exact molecular mechanism of RNF126 in HCC remain unclear. In this study, we investigated the role of RNF126 in the pathogenesis of HCC. By analyzing database and verifying with our clinical specimens, it was found that RNF126 was highly expressed in HCC tissues, which is associated with shorter overall survival and higher recurrence rate. Overexpressed RNF126 can significantly promote the proliferation, migration, invasion and angiogenesis of HCC cells, whereas knockdown RNF126 can reverse this effect. Mechanically, RNF126 down-regulates liver kinase B1 (LKB1) expression by ubiquitination of LKB1 to weaken its stability, thereby significantly promoting stem-cell-like activity, migration, and angiogenesis of HCC. Notably, consistent with in vitro results, RNF126 was stably transformed in Hep3B and subcutaneously injected into nude mice. In established mouse xenograft models, tumor growth can be effectively inhibited and the occurrence of lung metastasis is reduced. In HCC, RNF126 may down-regulate LKB1 through ubiquitination, thus becoming a powerful prognostic biomarker and a recognized tumor suppressor. Therefore, our study may provide a promising new therapeutic strategy for targeting RNF126 for HCC patients.
Access this article
We’re sorry, something doesn't seem to be working properly.
Please try refreshing the page. If that doesn't work, please contact support so we can address the problem.








Similar content being viewed by others
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. https://doi.org/10.3322/caac.21492.
Yang JD, Hainaut P, Gores GJ, Amadou A, Plymoth A, Roberts LR. A global view of hepatocellular carcinoma: trends, risk, prevention and management. Nat Rev Gastroenterol Hepatol. 2019;16(10):589–604. https://doi.org/10.1038/s41575-019-0186-y.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):7–30. https://doi.org/10.3322/caac.21442.
Bruix J, Qin S, Merle P, Granito A, Huang YH, Bodoky G, et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;389(10064):56–66. https://doi.org/10.1016/S0140-6736(16)32453-9.
Huang J, Lok V, Ngai CH, Zhang L, Yuan J, Lao XQ, et al. Worldwide burden of, risk factors for, and trends in pancreatic cancer. Gastroenterology. 2021;160(3):744–54. https://doi.org/10.1053/j.gastro.2020.10.007.
Torimura T, Iwamoto H. Treatment and the prognosis of hepatocellular carcinoma in Asia. Liver Int. 2021. https://doi.org/10.1111/liv.15130.
Chen Q, Shu C, Laurence AD, Chen Y, Peng BG, Zhen ZJ, et al. Effect of Huaier granule on recurrence after curative resection of HCC: a multicentre, randomised clinical trial. Gut. 2018;67(11):2006–16. https://doi.org/10.1136/gutjnl-2018-315983.
Ciechanover A. The unravelling of the ubiquitin system. Nat Rev Mol Cell Biol. 2015;16(5):322–4. https://doi.org/10.1038/nrm3982.
Nakayama KI, Nakayama K. Ubiquitin ligases: cell-cycle control and cancer. Nat Rev Cancer. 2006;6(5):369–81. https://doi.org/10.1038/nrc1881.
Lee NS, Chang HR, Kim S, Ji JH, Lee J, Lee HJ, et al. Ring finger protein 126 (RNF126) suppresses ionizing radiation-induced p53-binding protein 1 (53BP1) focus formation. J Biol Chem. 2018;293(2):588–98. https://doi.org/10.1074/jbc.M116.765602.
Yang X, Pan Y, Qiu Z, Du Z, Zhang Y, Fa P, et al. RNF126 as a biomarker of a poor prognosis in invasive breast cancer and CHEK1 inhibitor efficacy in breast cancer cells. Clin Cancer Res. 2018;24(7):1629–43. https://doi.org/10.1158/1078-0432.CCR-17-2242.
Kamikubo K, Kato H, Kioka H, Yamazaki S, Tsukamoto O, Nishida Y, et al. A molecular triage process mediated by RING finger protein 126 and BCL2-associated athanogene 6 regulates degradation of G0/G1 switch gene 2. J Biol Chem. 2019;294(40):14562–73. https://doi.org/10.1074/jbc.RA119.008544.
Smith CJ, Berry DM, McGlade CJ. The E3 ubiquitin ligases RNF126 and Rabring7 regulate endosomal sorting of the epidermal growth factor receptor. J Cell Sci. 2013;126(Pt 6):1366–80. https://doi.org/10.1242/jcs.116129.
Zhang R, Liu W, Sun J, Kong Y, Chen C. Roles of RNF126 and BCA2 E3 ubiquitin ligases in DNA damage repair signaling and targeted cancer therapy. Pharmacol Res. 2020;155: 104748. https://doi.org/10.1016/j.phrs.2020.104748.
Zhang R, Zhu Y, Li Y, Liu W, Yin L, Yin S, et al. Human umbilical cord mesenchymal stem cell exosomes alleviate sepsis-associated acute kidney injury via regulating microRNA-146b expression. Biotechnol Lett. 2020;42(4):669–79. https://doi.org/10.1007/s10529-020-02831-2.
He X, Ai S, Guo W, Yang Y, Wang Z, Jiang D, et al. Umbilical cord-derived mesenchymal stem (stromal) cells for treatment of severe sepsis: a phase 1 clinical trial. Transl Res. 2018;199:52–61. https://doi.org/10.1016/j.trsl.2018.04.006.
Zhi X, Zhao D, Wang Z, Zhou Z, Wang C, Chen W, et al. E3 ubiquitin ligase RNF126 promotes cancer cell proliferation by targeting the tumor suppressor p21 for ubiquitin-mediated degradation. Cancer Res. 2013;73(1):385–94. https://doi.org/10.1158/0008-5472.CAN-12-0562.
Wang C, Wen A, Qiao J, Liu Y, Guo Y, Wang W. High expression of RING finger protein 126 predicts unfavorable prognosis of epithelial ovarian cancer. Med Sci Monit. 2020;26:e921370. https://doi.org/10.12659/MSM.921370.
Xu H, Ju L, Xiong Y, Yu M, Zhou F, Qian K, et al. E3 ubiquitin ligase RNF126 affects bladder cancer progression through regulation of PTEN stability. Cell Death Dis. 2021;12(3):239. https://doi.org/10.1038/s41419-021-03521-1.
Shackelford DB, Shaw RJ. The LKB1-AMPK pathway: metabolism and growth control in tumour suppression. Nat Rev Cancer. 2009;9(8):563–75. https://doi.org/10.1038/nrc2676.
Hollstein PE, Eichner LJ, Brun SN, Kamireddy A, Svensson RU, Vera LI, et al. The AMPK-related kinases SIK1 and SIK3 mediate key tumor-suppressive effects of LKB1 in NSCLC. Cancer Discov. 2019;9(11):1606–27. https://doi.org/10.1158/2159-8290.CD-18-1261.
Bi L, Ren Y, Feng M, Meng P, Wang Q, Chen W, et al. HDAC11 regulates glycolysis through the LKB1/AMPK signaling pathway to maintain hepatocellular carcinoma stemness. Cancer Res. 2021;81(8):2015–28. https://doi.org/10.1158/0008-5472.CAN-20-3044.
Liu X, Sui X, Zhang C, Wei K, Bao Y, Xiong J, et al. Glutathione S-transferase A1 suppresses tumor progression and indicates better prognosis of human primary hepatocellular carcinoma. J Cancer. 2020;11(1):83–91. https://doi.org/10.7150/jca.36495.
Li N, Wang Y, Neri S, Zhen Y, Fong LWR, Qiao Y, et al. Tankyrase disrupts metabolic homeostasis and promotes tumorigenesis by inhibiting LKB1-AMPK signalling. Nat Commun. 2019;10(1):4363. https://doi.org/10.1038/s41467-019-12377-1.
World Medical A. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–4. https://doi.org/10.1001/jama.2013.281053.
Chen H, Zhang L. Downregulation of FPR1 abates lipopolysaccharide-induced inflammatory injury and apoptosis by upregulating MAPK signaling pathway in murine chondrogenic ATDC5 cells. Allergol Immunopathol (Madr). 2021;49(5):57–63. https://doi.org/10.15586/aei.v49i5.455.
He Y, Li Q, Zhou W, Gu Y, Jiang Y. Coniferyl aldehyde alleviates LPS-induced WI-38 cell apoptosis and inflammation injury via JAK2-STAT1 pathway in acute pneumonia. Allergol Immunopathol (Madr). 2021;49(5):72–7. https://doi.org/10.15586/aei.v49i5.464.
Bai S, Chen W, Zheng M, Wang X, Peng W, Zhao Y, et al. Spindle and kinetochore-associated complex subunit 3 (SKA3) promotes stem cell-like properties of hepatocellular carcinoma cells through activating Notch signaling pathway. Ann Transl Med. 2021;9(17):1361. https://doi.org/10.21037/atm-21-1572.
Wang S, Wang L, Hu H, Dong P. MiR-224 ameliorates inflammation and symptoms in mouse model of allergic rhinitis by targeting CDK9. Allergol Immunopathol (Madr). 2021;49(6):80–8. https://doi.org/10.15586/aei.v49i6.451.
Luo J, Wang P, Wang R, Wang J, Liu M, Xiong S, et al. The Notch pathway promotes the cancer stem cell characteristics of CD90+ cells in hepatocellular carcinoma. Oncotarget. 2016;7(8):9525–37. https://doi.org/10.18632/oncotarget.6672.
In: th, editor. Guide for the Care and Use of Laboratory Animals. The National Academies Collection: Reports funded by National Institutes of Health. Washington (DC) 2011.
Zhou C, Liu C, Liu W, Chen W, Yin Y, Li CW, et al. SLFN11 inhibits hepatocellular carcinoma tumorigenesis and metastasis by targeting RPS4X via mTOR pathway. Theranostics. 2020;10(10):4627–43. https://doi.org/10.7150/thno.42869.
Lytle NK, Barber AG, Reya T. Stem cell fate in cancer growth, progression and therapy resistance. Nat Rev Cancer. 2018;18(11):669–80. https://doi.org/10.1038/s41568-018-0056-x.
Visvader JE, Lindeman GJ. Cancer stem cells in solid tumours: accumulating evidence and unresolved questions. Nat Rev Cancer. 2008;8(10):755–68. https://doi.org/10.1038/nrc2499.
Yaghobi Z, Movassaghpour A, Talebi M, Abdoli Shadbad M, Hajiasgharzadeh K, Pourvahdani S, et al. The role of CD44 in cancer chemoresistance: a concise review. Eur J Pharmacol. 2021;903: 174147. https://doi.org/10.1016/j.ejphar.2021.174147.
Liu T, Duan X, He J, Yang C. KCNQ1OT1 promotes the proliferation and migration of psoriatic keratinocytes by regulating miR-183–3p/GAB1. Allergol Immunopathol (Madr). 2021;49(5):125–30. https://doi.org/10.15586/aei.v49i5.480.
Yu X, Zheng Y, Zhu X, Gao X, Wang C, Sheng Y, et al. Osteopontin promotes hepatocellular carcinoma progression via the PI3K/AKT/Twist signaling pathway. Oncol Lett. 2018;16(4):5299–308. https://doi.org/10.3892/ol.2018.9281.
Hartke J, Johnson M, Ghabril M. The diagnosis and treatment of hepatocellular carcinoma. Semin Diagn Pathol. 2017;34(2):153–9. https://doi.org/10.1053/j.semdp.2016.12.011.
Sun Z, Liu X, Chen M, Zhang H, Zeng X. Overexpression of RNF126 is associated with poor prognosis and contributes to the progression of lung adenocarcinoma. Biomark Med. 2021;15(15):1345–55. https://doi.org/10.2217/bmm-2020-0798.
Wang Y, Chu Y, Li K, Zhang G, Guo Z, Wu X, et al. Exosomes secreted by adipose-derived mesenchymal stem cells foster metastasis and osteosarcoma proliferation by increasing COLGALT2 expression. Front Cell Dev Biol. 2020;8:353. https://doi.org/10.3389/fcell.2020.00353.
Li H, Feng Z, He ML. Lipid metabolism alteration contributes to and maintains the properties of cancer stem cells. Theranostics. 2020;10(16):7053–69. https://doi.org/10.7150/thno.41388.
Yan Y, Zuo X, Wei D. Concise review: emerging role of CD44 in cancer stem cells: a promising biomarker and therapeutic target. Stem Cells Transl Med. 2015;4(9):1033–43. https://doi.org/10.5966/sctm.2015-0048.
Kawaguchi M, Dashzeveg N, Cao Y, Jia Y, Liu X, Shen Y, et al. Extracellular Domains I and II of cell-surface glycoprotein CD44 mediate its trans-homophilic dimerization and tumor cluster aggregation. J Biol Chem. 2020;295(9):2640–9. https://doi.org/10.1074/jbc.RA119.010252.
Zhong L, Pan Y, Shen J. FBXW7 inhibits invasion, migration and angiogenesis in ovarian cancer cells by suppressing VEGF expression through inactivation of beta-catenin signaling. Exp Ther Med. 2021;21(5):514. https://doi.org/10.3892/etm.2021.9945.
Whynott RM, Manahan P, Geisler JP. Vascular endothelial growth factor (VEGF) and cyclooxygenase 2 (COX 2) immunostaining in ovarian cancer. Eur J Gynaecol Oncol. 2016;37(2):164–6.
Klein CA. Cancer progression and the invisible phase of metastatic colonization. Nat Rev Cancer. 2020;20(11):681–94. https://doi.org/10.1038/s41568-020-00300-6.
Acknowledgements
Not applicable.
Funding
This work was supported by the Yunnan Science and Technology Department and Kunming Medical University Special Fund (Grant No. 202001AY070001-229), the Yun nan Fundamental Research Projects (Grant No. 202101AT070239) and the Investigator Initiated Trail Projects of the Second Affiliated Hospital of Kunming Medical University (Grant No. 2020ynlc004).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and the experiments were performed by JH. Data collection and analysis were performed by YL, MZ and HH. The first draft of the manuscript was written by DX and DT and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors state that there are no conflicts of interest to disclose.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the standards upheld by the Ethics Committee of the Second Affiliated Hospital of Kunming Medical University and with those of the 1964 Helsinki Declaration and its later amendments for ethical research involving human subjects. All animal experiments were approved by the Ethics Committee of the Second Affiliated Hospital of Kunming Medical University for the use of animals and conducted in accordance with the National Institutes of Health Laboratory Animal Care and Use Guidelines(Approval No.kmmu20200411).
Statement of informed consent
Written informed consent was obtained from a legally authorized representative(s) for anonymized patient information to be published in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, J., Li, Y., Zheng, M. et al. RNF126 contributes to stem cell-like properties and metastasis in hepatocellular carcinoma through ubiquitination and degradation of LKB1. Human Cell 35, 1869–1884 (2022). https://doi.org/10.1007/s13577-022-00782-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13577-022-00782-6