Abstract
Purpose
The purpose of this study is to evaluate the differences in treatment optimization algorithms in two leading treatment planning systems, Pinnacle v9.8 (Philips Healthcare, Amsterdam, Netherlands) and Raystation 8A (Raysearch Americas Inc., Garden City, USA). The aim is to compare and contrast between planning systems in terms of sparing of vital organs (SVO) using several gradient and conformity indices, as well as vital organ dose limits.
Methods
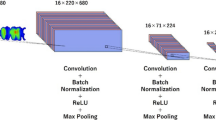
The study includes patients (N = 18) presenting with lung (10), liver (4), and head and neck (4) tumors and treated with intensity modulated radiation therapy (IMRT) or volumetric modulated arc therapy (VMAT) planned using the same objectives and weights, number of iterations, beam angles, and planning target volume (PTV) coverage. Both plans were analyzed for Radiation Therapy Oncology Group (RTOG) conformity index, Paddick conformity index, gradient index (GI), dose gradient index, and sparing of vital organs. This study utilized both segmented and dynamic approaches to multileaf collimation (SMLC and DMLC, respectively) in the Raystation planning system in lung IMRT plans, as some plans could not be optimized in Raystation with SMLC (7).
Results
It was determined that in lung plans, Pinnacle demonstrated better sparing of the right lung and the spinal cord, but Raystation more effectively spared the heart and esophagus. In liver plans, Raystation demonstrated a superior GI, indicating faster dose falloff; this correlated with lower volumes of the liver receiving 24 Gy. In head and neck (H&N) plans, Pinnacle demonstrated superior sparing of the parotid but inferior GI, indicating more rapid dose falloff in Raystation beyond the PTV.
Conclusions
The analysis for the lung, liver, and H&N cases indicated that both planning systems are equivocal for the majority of parameters measured, with a few differentiating trends. In H&N plans, Pinnacle showed improved parotid sparing but inferior performance in calculated GI values. Liver plans showed superiority of Raystation in GI computations, but the most notable differences were in the lung plans where Pinnacle spared the spinal cord significantly more in contrast to Raystation’s performance but also delivered significantly more dose to the esophagus.
Similar content being viewed by others
Abbreviations
- PCI:
-
Paddick conformity index
- RTOGCI:
-
RTOG conformity index
- CN:
-
conformation number
- CNS:
-
central nervous system
- CT:
-
computed tomography
- CTV:
-
clinical target volume
- IDL:
-
isodose line
- DGI:
-
dose gradient index
- DVH:
-
dose-volume histogram
- DMLC:
-
dynamic multileaf collimator
- GI:
-
gradient index
- GTV:
-
gross tumor volume
- IMRT:
-
intensity modulated radiation therapy
- LL:
-
left lung
- LP:
-
left parotid
- MLC:
-
multileaf collimator
- OAR:
-
organ at risk
- PI:
-
prescription isodose
- PIV:
-
prescription isodose volume
- PIV50% :
-
volume of the 50% prescription isodose
- PTV:
-
planning target volume
- Reff,50%Rx :
-
effective radius of the 50% prescription isodose
- Reff,Rx :
-
effective radius of the prescription isodose
- RL:
-
right lung
- RP:
-
right parotid
- ROI:
-
region of interest
- RTOG:
-
Radiation Therapy Oncology Group
- SMLC:
-
segmented multileaf collimator
- SRS:
-
stereotactic radiosurgery
- SVO:
-
sparing of vital organs
- TPS:
-
treatment planning system
- TV:
-
target volume, defined as the PTV for this study
- TVPIV :
-
volume of prescription isodose located within the target volume
- VOAR:
-
volume of organ at risk
References
Siegel RL, Miller KD, Jemal A (2017) Cancer statistics, 2017. CA Cancer J Clin 67:7–30. https://doi.org/10.3322/caac.21387
Barton MB, Jacob S, Shafiq J, Wong K, Thompson SR, Hanna TP, Delaney GP (2014) Estimating the demand for radiotherapy from the evidence: a review of changes from 2003 to 2012. Radiother Oncol 112:140–144. https://doi.org/10.1016/j.radonc.2014.03.024
Jaffray DA, Gospodarowicz MK. (2015) Radiation Therapy for Cancer DCP3. doi: https://doi.org/10.1596/978-1-4648-0349-9_ch14
Sterzing F, Stoiber EM, Nill S, Bauer H, Huber P, Debus J, Münter MW (2009) Intensity modulated radiotherapy (IMRT) in the treatment of children and adolescents - a single institution’s experience and a review of the literature. Radiat Oncol 4:37. https://doi.org/10.1186/1748-717x-4-37
Teh BS, Woo SY, Butler EB (1999) Intensity modulated radiation therapy (IMRT): a new promising technology in radiation oncology. Oncologist 4:433–442
Chen W-Z (2014) Impact of dose calculation algorithm on radiation therapy. World J Radiol 6:874–880. https://doi.org/10.4329/wjr.v6.i11.874
Jothybasu K, Bahl A, Subramani V, Rath G, Sharma D, Julka P (2009) Static versus dynamic intensity-modulated radiotherapy: profile of integral dose in carcinoma of the nasopharynx. J Med Phys 34:66–72. https://doi.org/10.4103/0971-6203.51932
Alaei P, Higgins PD, Weaver R, Nguyen N (2004) Comparison of dynamic and step-and-shoot intensity-modulated radiation therapy planning and delivery. Med Dosim 29:1–6. https://doi.org/10.1016/j.meddos.2003.10.002
Hall EJ (2006) Intensity-modulated radiation therapy, protons, and the risk of second cancers. Int J Radiat Oncol Biol Phys 65:1–7. https://doi.org/10.1016/j.ijrobp.2006.01.027
Shaw E, Kline R, Gillin M, Souhami L, Hirschfeld A, Dinapoli R, Martin L (1993) Radiation Therapy Oncology Group: radiosurgery quality assurance guidelines. Int J Radiat Oncol Biol Phys 27:1231–1239. https://doi.org/10.1016/0360-3016(93)90548-A
Feuvret L, Noël G, Mazeron JJ, Bey P (2006) Conformity index: a review. Int J Radiat Oncol Biol Phys 64:333–342. https://doi.org/10.1016/j.ijrobp.2005.09.028
Paddick I (2000) A simple scoring ratio to index the conformity of radiosurgical treatment plans: technical note. J Neurosurg 93:219–222. https://doi.org/10.3171/jns.2000.93.supplement
Paddick I, Lippitz B (2006) A simple dose gradient measurement tool to complement the conformity index. J Neurosurg 105(Suppl):194–201. https://doi.org/10.3171/sup.2006.105.7.194
Torrens M, Chung C, Chung HT, Hanssens P, Jaffray D, Kemeny A, Larson D, Levivier M, Lindquist C, Lippitz B, Novotny J, Paddick I, Prasad D, Yu CP (2014) Standardization of terminology in stereotactic radiosurgery: report from the Standardization Committee of the International Leksell Gamma Knife Society: special topic. J Neurosurg 121:2–15. https://doi.org/10.3171/2014.7.GKS141199
Sheth NS, Sim S, Cheng J, Lustgarten J, Estin D, Olson T, Weiss M, Murphy S, Chen Y, Yang J (2011) A dose gradient index for stereotactic radiosurgery/radiotherapy: evaluated with helical tomotherapy. Int J Radiat Oncol Biol Phys 81(2):S867–S868
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this study.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Statement of informed consent was not applicable since the manuscript does not contain any patient data.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Parsai, E.I., Ulizio, V., Eckstein, J.M. et al. Quantitative assessment of the efficacy of two different treatment plan optimization algorithms in treating tumors in locations of high heterogeneity. J Radiat Oncol 8, 233–238 (2019). https://doi.org/10.1007/s13566-019-00392-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13566-019-00392-0