Abstract
Introduction
Cradle cap is a very common condition in infants that presents as greasy, scaly patches on the scalp within the first weeks of life. Although usually disappearing by itself, the condition worries parents because of its appearance. When removing the scales, it is crucial to prevent spot bleedings to avoid infections. The investigational medical device LOYON® (Cetiol® CC, dimethicone) solution (G. Pohl-Boskamp GmbH & Co. KG, Hohenlockstedt, Germany) has the potential to meet these needs since it removes scales gently. It was, therefore, the aim of this proof-of-concept study to assess the efficacy and safety of topically applied, non-medicated LOYON® in facilitating the removal of scaling in infants and children with cradle cap without inducing spot bleedings.
Methods
This single-center, open, proof-of-concept, pilot study was conducted in 20 male or female infants/children aged 3–36 months with clinically diagnosed cradle cap. The 8-day study period included one to three applications of LOYON®. Clinical assessment of scaling and secondary parameters was performed at baseline and after treatment. Adverse events were recorded. A questionnaire on subjective efficacy and usability was handed out to the parents.
Results
With a maximum of three applications of LOYON® applied to 20 subjects, a reduction in scaling intensity from moderate or severe to very mild or mild was achieved in 80% of the subjects. Treatment success, defined as the reduction of the scaling baseline score by at least two points, was achieved in 50% of subjects. Results of this study do not indicate any safety concern. No spot bleedings were observed. LOYON® was generally well tolerated and overall treatment was rated as “good” by the parents/legal guardians.
Conclusion
This study suggests that LOYON® is well tolerated, safe and effective in facilitating the removal of scaling in infants and children with cradle cap. With its gentle approach and rapid effect, LOYON® thus represents a good alternative to home remedies for treatment of cradle cap.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cradle cap is a form of seborrheic dermatitis that mainly manifests as thick, crusty, yellow scales on the scalp of infants and young children. It is a very common condition, usually appearing within the first 6 weeks of life and clearing spontaneously by about 6–9 months of age [1, 2]. The prevalence of cradle cap is rarely reported. According to Foley et al. [3], the overall age- and sex-adjusted prevalence of seborrheic dermatitis in Australian preschool-aged children was 10%. A prevalence of 9.6 per 1,000 persons aged 1–5 years was reported in one study from the United States [4]. An incidence of 10% was observed for newborns in one investigation of neonatal cutaneous lesions from India [5]. Many factors including proliferation of the yeast Malassezia furfur (formerly Pityrosporum ovale), transplacental hormones and dysfunction of the sebaceous glands have been implicated in the pathogenesis of cradle cap, however, its exact etiology and pathogenesis are still unknown [2, 6, 7].
The distinction between cradle cap or infantile seborrheic dermatitis and other skin disorders such as atopic dermatitis and psoriasis can be difficult in infants. This is due to the considerable overlap of clinical features such as hyperkeratosis, inflammation, pruritus and hair loss and combined forms which may exist [8, 9]. Distinguishing features may involve age at onset, course, distribution and pruritus. Whereas cradle cap is characterized by its early onset, mild and self-limited course, typical clinical picture, absence of itch and discomfort, atopic dermatitis is a chronic pruritic disease that may present as early as 3 months of age and due to severe itching and irritation can be extremely bothersome to the child. Psoriasis, on the other hand, is uncommon in this age group and is characterized by sharply demarcated erythematous lesions surmounted by a silvery scale [1, 2, 7, 10].
Although cradle cap usually resolves within 6–8 weeks [11], some cases may persist longer, and even if lasting for only a few weeks the condition worries parents because of its appearance [1]. Cradle cap may also have a bad smell. That is why caregivers generally want to act rather than wait for the condition to spontaneously resolve, even if medical treatment is usually not indicated. Although the majority of cases would require little, if any, treatment, medical intervention may be indicated in some cases. For example, if moisture accumulating under the scales causes pruritus and leads the infant to scratch affected areas, resulting skin lesions may provoke secondary infections necessitating medical treatment. Where medical therapy is indicated, thick layers of scales might prevent medications from reaching their target sites. When removing the scales in cradle cap or other cutaneous disorders that share a similar clinical picture such as psoriasis, it is crucial to use a gentle approach to prevent spot bleedings to avoid the occurrence of infections.
Management of cradle cap depends on the severity of the disease. In mild cases, daily shampooing using a non-medicated baby shampoo may be effective in loosening and removing scales. Should simple shampooing prove ineffective, emollients such as warmed mineral or olive oil or white petrolatum are often applied to soften scales, followed by gentle removal with a soft hairbrush and shampooing. In severe or persistent cases, emollients in combination with medical treatments may be used, with reported topical medications including keratolytic agents like salicylic acid, anti-inflammatory agents such as low-potency steroids, antimycotics, for instance ketoconazole, and antibiotics [1, 12–14]. Gentle approaches will suffice to treat most infants with cradle cap, with non-medicated topicals serving as first-line treatment to facilitate removal of scales and reduce the need for medical treatments carrying potential risks, which is of particular importance in this age group. Although generally not indicated, medications may be required in a few cases as second-line treatment; however, their use in infants and young children is highly debatable, due to unproven efficacy and a general lack of rigorous safety data in this age group. Safety concerns of conventional medical treatments include salicylism resulting from percutaneous absorption of salicylic acid and local or systemic effects produced by percutaneous absorption of steroids, e.g., skin atrophy or adrenocortical suppression. With regard to antimycotics or antibiotics, these should only be used in established mycoses or bacterial infections, respectively, otherwise the benefits are questionable [1, 7, 10, 15–17].
Limited evidence exists regarding the benefits of currently available treatment modalities for cradle cap [15]. Especially non-medicated symptomatic measures, for example home remedies such as olive oil, are not well investigated and controversially discussed [18–20]. Natural oils further have the disadvantage of lacking standardization, and some of them cannot be used in case of allergy, for example, arachis oil should not be used in a child who is allergic to peanuts [1]. Hence, products with proven clinical safety and efficacy are still needed for cradle cap; these should preferably not pose a pharmacological burden in this patient population and should not result in spot bleedings. Therefore, a new topical, non-medicated product for facilitating the removal of scaling in infants and children with cradle cap has been developed, the investigational medical device LOYON® (Cetiol® CC, dimethicone) solution (G. Pohl-Boskamp GmbH & Co. KG, Hohenlockstedt, Germany).
LOYON®, which is referred to as investigational medical device (IMD) during the present study, is a solution containing Cetiol® CC (dicaprylyl carbonate) (BASF SE, Ludwigshafen, Germany), a fast spreading emollient with excellent dermatological compatibility [21], and two dimethicones (polydimethylsiloxane/silicones), which serve as skin protectants and moisturizers [22]. These components have a long history of safe use. They are found in medicinal products, medical devices and cosmetics. Its viscosity and creeping/spreading properties allow the IMD to readily flow underneath the scales and remove them in a gentle way. Softening of the scales by the solution further eases their removal. Due to the gentle physical removal process, spot bleedings are likely avoided. In addition, given its mode of action, the effectiveness of the IMD is independent of the cause which leads to the skin alterations: the IMD thus appears capable of removing scales present in several clinical entities such as cradle cap, seborrheic dermatitis and psoriasis.
The aim of this proof-of-concept study was to evaluate the efficacy and safety of topically applied, non-medicated LOYON® in facilitating the removal of scaling in infants and children with cradle cap of the scalp without inducing spot bleedings.
Methods
This single-center, open, proof-of-concept, pilot study was conducted from November 1, 2011 to February 21, 2012 at Bioskin GmbH, Berlin, Germany.
Compliance with Ethics Guidelines
All procedures were followed in compliance with Good Clinical Practice (GCP) and in accordance with the Declaration of Helsinki of 1975, as revised in 2000 and 2008, and national laws and regulations. Informed consent was obtained for all parents/legal guardians included in this study. The investigational medical device (IMD), LOYON® (Cetiol® CC, dimethicone) solution, was manufactured by G. Pohl-Boskamp GmbH & Co. KG, Hohenlockstedt, Germany (Note: during process of study the official brand name changed from Loion® to LOYON®).
Male or female infants/children aged 3–36 months with clinically diagnosed cradle cap on the scalp and a scaling score of at least 2 on a 5-point scale from 0 to 3 (0, 0.5, 1, 2 and 3) were eligible for the study. For study inclusion, the physical examination of the scalp had to be without abnormal findings, unless the investigator considered an abnormality irrelevant to the outcome of the study. Subjects were excluded from this study, if they experienced symptoms of a clinically significant illness with potential influence on the outcome of the study within 4 weeks prior to or during the study, if they suffered from inflammation, tinea capitis or psoriasis capitis, if they used dimethicone containing shampoos and/or if they participated in another clinical trial within 4 weeks prior to or during the study. Further exclusion criteria were known hypersensitivity to components of the study preparation and treatment within 4 weeks prior to or during the study with systemically or locally acting drugs such as steroids, antimycotics, salicylic acid or other keratolytics, or skin care products such as olive oil with potential influence on the outcome of the study. The use of baby shampoos was allowed within 4 weeks prior to the study.
The IMD was not to be applied together with other hair care or hair cosmetic products. All relevant medication that had been taken 6 weeks prior to Day 1 and any medication, including over-the-counter remedies, that were taken during the study were regarded as concomitant treatment and had to be documented. The use of vitamin D preparations and fluorine-containing medications was allowed. Other concomitant medications were to be kept to a minimum during the study; however, if considered necessary for the subject’s welfare and unlikely to interfere with the study objectives, these were allowed at the discretion of the investigator.
The primary aim of this open, short-term study was proof-of-concept, comparing treatment effects with baseline. Primary efficacy parameters were scaling in the target area of the scalp and treatment success. Secondary efficacy parameters were the presence of spot bleedings, redness, time to treatment success, and the analysis of the parent(s)/legal guardian(s) questionnaire on subjective efficacy, usability and further cosmetic items. Clinical assessment of scaling and redness was performed using 5-point scales from 0 to 3 (0, 0.5, 1, 2 and 3). Scales used for scoring of the target area of the scalp for scaling and redness are shown in Table 1. Scaling and redness were assessed separately, with the scoring performed by two trained investigators to assure comparable grading. Treatment success was defined as the reduction of the scaling baseline score by at least two points, i.e., a resulting grade of 0.5 or 1 at maximum when the initial score was 2 or 3, respectively. Time to treatment success was determined as the difference of the visit day of the first occurrence of treatment success minus one (baseline visit day). In case of no treatment success until Day 4, the outcome was assigned as “no treatment success”.
Safety parameters were adverse events (AEs) and device deficiencies. Spontaneously noted complaints were recorded with duration, intensity and assessment of causality with the study preparation. Relevant medical history of the previous three months was recorded. Laboratory parameters were not monitored during the course of the study. Photographic documentation of the scalp was performed under standardized conditions (e.g., distance, illumination).
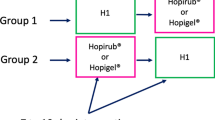
The 8-day study schedule included a baseline visit, depending on treatment success one to three control visits, and a follow-up visit. On the first day of the study, the target area, defined as the worst affected area on the scalp, was selected and its location on the scalp was documented. The outline of the affected area and the target area were traced onto a transparent plastic sheet. Baseline scores for scaling in the target area of the scalp and for secondary parameters were assessed. Following baseline evaluation, all subjects were treated at least once (Day 1). In case of no treatment success, i.e., a reduction of the scaling baseline score by less than two points, further treatments were performed on Days 2 and 3. The target area and adjoining areas were treated, with the study drug administration performed by the parent(s)/legal guardian(s) under supervision of Bioskin staff according to the instructions for use. The IMD was pipetted drop wise to the entire affected area of the dry scalp, excessive solution was swabbed with a soft paper tissue and the solution was spread by gentle massage until the area was completely moistened. The dose to be applied was not defined and depended on the size of the affected area. The study preparation had to be washed off at home by the parent(s)/legal guardian(s) at the earliest 3 h after application and at the latest before the next site visit on the following day using a standardized shampoo (HiPP Baby Shampoo™, HiPP GmbH & Co. Vertrieb KG, Pfaffenhofen, Germany). On Day 2, subjects returned to Bioskin for assessment of scaling and further study parameters. As long as no treatment success was achieved, study drug administration to the affected area was repeated; it was carried out at most thrice. Clinical assessment of the target area was performed on Day 1 (before treatment), 2 (after treatment) and 8 ± 1 (at follow-up), and—in case of no treatment success on an earlier day—also on Days 3 and 4. On Day 2, 3 or 4, depending on the day of treatment success, the parent(s)/legal guardian(s) filled out a questionnaire on subjective efficacy, usability and further cosmetic items of the study preparation. On Day 8 (±1), subjects returned for a follow-up visit where scaling and further study parameters were scored for assessment of persistence of treatment effect and safety. The scalp was also documented photographically at baseline and on all further visits including the follow-up visit.
The statistical analyses were performed at Bioskin using the software program SAS (Statistical analysis system (SAS) Institute Inc., Cary, USA) version 9.2 or higher. All analyses were explorative and interpreted descriptively. The intention-to-treat (ITT) analysis was based on the full analysis set (FAS) including all subjects who received the study device at least once and had at least one post-baseline assessment. The per-protocol (PP) analysis was based on the valid cases set (VCS) including all subjects without any major violation to the study plan, who received all the doses and with available values of the primary variables at all days. All safety analyses were based on the safety evaluation set (SES) including all subjects who received the study preparation at least once.
Results
A total of 20 male or female infants/children aged 3–36 months with cradle cap on the scalp (scaling score ≥2) were enrolled in this study, 19 of whom completed the trial. Data of all 20 subjects were valid for the SES and FAS. Nineteen subjects were included in the VCS. One subject prematurely discontinued the investigation due to an AE (fever) on Day 2, which was assessed as unlikely related to the study preparation. Since this subject did not receive the full dose, this boy was excluded from the PP population. Demographic characteristics of the study participants are summarized in Table 2. With regard to previous and concomitant therapies, 12 subjects were taking medication for prophylaxis of cold and 2 subjects took medication for treatment of cold.
Before treatment all subjects experienced moderate to severe scaling (moderate 80% of subjects, severe 20% of subjects). The mean scaling score at baseline was 2.2 ± 0.4. Following treatment with the IMD, LOYON®, a reduction of scaling intensity was seen in the target area of the scalp skin in most of the subjects during the study course: with one to a maximum of three applications of the IMD to the total affected area of the scalp a reduction from moderate or severe to no, very mild or mild in scaling was seen in 80% of the subjects (Fig. 1). Complete resolution of scaling was noted in one subject on Day 3, in one further subject on Day 4 and in two further subjects at the follow-up visit (Day 8 ± 1). On Day 4, the mean scaling score was 1.0 ± 0.9, corresponding to a mean change from baseline of −1.2 ± 0.6. Representative photographs showing different degrees of scalp scaling are depicted in Fig. 2.
Clinical assessment of scaling during the study course. The target area of the scalp was scored for scaling on Day 1 (baseline), and after treatment on Day 2, on Days 3 and 4 in case of no treatment success on an earlier day and on Day 8 using the scale shown in Table 1
As shown in Fig. 3, treatment success—defined as the reduction of the scaling baseline score by at least two points—was achieved in 50% of subjects, predominantly after 3 days of treatment: 5% of subjects had achieved treatment success on Day 2, additional 10% of subjects on Day 3 and further 35% of subjects on Day 4, yielding a time to treatment success of 1, 2 and 3 days in 5, 10 and 35% of subjects, respectively. No spot bleedings were observed at any time point during the entire study period. No redness at the target area was noted in any subject at baseline; after treatment with the IMD, moderate redness was observed in two subjects (in one subject on Days 2 and 4 and in another subject on Day 3) and very mild to mild redness at the target area occurred in most subjects during the study period, with the largest percentage (75%) occurring on Day 4 (Fig. 4). At the follow-up visit resolution of redness was observed in 53% of the subjects.
Clinical assessment of redness. The target area of the scalp was scored for redness on Day 1 (baseline), and after treatment on Days 2, on Days 3 and 4 in case of no treatment success on an earlier day and on Day 8 using the scale shown in Table 1
The results recorded by the investigators are in agreement with the positive treatment evaluations by the parents/legal guardians. According to the judgment by most parents/legal guardians the product is easy to apply (90% of parents/legal guardians), has a comfortable consistency (80%) and brings about a significant improvement of skin appearance (85%). 70% of them were satisfied with the improved skin appearance in their children, with 20% experiencing this as positively affecting the relationship to their child. In one subject, an unpleasant odor of the affected skin had been noted at baseline which improved with treatment. Overall treatment with the IMD was rated as ‘good’.
Regarding safety, a total of seven non-serious AEs of mild to moderate intensity were reported in five subjects (Table 3). Two AEs concerned itching and were assessed as probably related to the study preparation and the procedure. In a further child, soft yellow crusts with tiny vesicles and no signs of infection or pruritus at the application area were noted. This AE was assessed as possibly related to the study preparation, with the investigator suggesting an accumulation of sweat under the crust. The other four AEs (cold with fever, fever, rhinitis and conjunctivitis) were considered as unlikely related to the study preparation. Whereas five AEs had resolved at the end of the study, two AEs [cold with fever and fever (dropout on Day 2)] were still ongoing on Day 8, follow-up by phone revealed that both affected subjects had made a full recovery. There were no device deficiencies recorded during the study.
Discussion
As opposed to conventional treatments for cradle cap that often contain salicylic acid, steroids or antimycotics, the IMD (LOYON®) does not contain any pharmacologically active ingredient. Unlike medicinal products, it does not achieve its effect by pharmacological or immunological means, but by a physical mode of action with the absence of systemic effects. Its viscosity and creeping/spreading properties allow the IMD to readily flow underneath the scales and gently remove them. Moreover, scales are softened by the solution, additionally easing their removal. The aim of the present study was proof-of-concept, i.e., the evaluation of efficacy and safety of a topically applied IMD in facilitating the removal of scales in infants and children with cradle cap.
Indeed, treatment with the IMD reduced scaling of the scalp skin in most of the infants or children with cradle cap and the onset of effect was rapid: an improvement was already observed after one to three administrations. A reduction from at least moderate scaling to mild scaling or less was noted in 80% of subjects. Concurrently, very mild to mild redness was noted in most of the subjects during the study period, i.e., in 75% of subjects on Day 4. The presence of the two clinical findings, improvement in scaling and appearance of mild redness, favors the occurrence of mild redness as being due to the removal of scales rather than due to irritation. In more than half of the subject, redness had disappeared at the follow-up visit on Day 8 ± 1.
A treatment success, i.e., reduction in scaling intensity by at least two points, was achieved in half of the subjects. This treatment success occurred after only one or two applications in some subjects and was generally reached after three applications. Since cradle cap can be rather tenacious, this is an especially remarkable study result. In addition, treatment effects persisted without further application, as assessed at the follow-up. It might thus be speculated that a longer treatment period with the IMD would result in a greater overall improvement of cradle cap and more subjects showing treatment success. Indeed, with a maximum of 3 days of treatment and a clinical investigation period of 8 (±1) days, the treatment period tested in this proof-of-concept study was rather short when compared to those used with other commonly used formulations [15].
The absence of any spot bleedings supports the assumption that the IMD acts in a particularly gentle way. Hence, treatment with the IMD may facilitate the removal of scales while minimizing the risk of infections. The positive experiences by the parents/legal guardians regarding the efficacy and usability of the IMD for treatment of cradle cap corroborate the evaluation by the investigators. Treatment with the IMD not only removed the scales effectively, but was also able to relieve the distress associated with their child’s cradle cap in the caretakers.
Results of this study do not indicate any safety concern. The number of AEs in this study was low, with all seven AEs being classified as non-serious. Three of these were assessed to be in some causal association with the study preparation. One AE was assessed as possibly related to the study device and concerned soft yellow crusts with tiny vesicles resembling accumulation of sweat under the crust. The reaction resolved within 5 days without treatment. Itching, which occurred in two subjects, was assessed as probably related to the study preparation and procedure. Overall, the IMD appears to be well tolerated in infants and young children. Specific risks were not observed.
There are several limitations of this study. First, this study involved only a limited sample size of 20 subjects. Yet, the main intention of this study was proof-of-concept and corresponding studies are usually small and obtained data may not be complete. Second, the study period was rather short and the number of applications limited. As for safety, specific risks were not observed with short-term use and, considering the composition and mode of action of the device, are not expected to occur with longer use.
This pilot study has been conducted to determine whether the IMD is effective in the removal of scaling during treatment of cradle cap. The chosen design allowed for a detection of possible signals for safety concerns without exposing a huge group of participants.
The study provided first evidence for the effectiveness of the IMD during the treatment and pointed to a good safety profile. However, there is a need for further trials to compare the IMD with other options for removal of scaling, such as olive oils or baby shampoos.
With regard to efficacy, treatment duration with only three applications was sufficient to achieve rapid improvement in 80% of the study participants. Third, this study lacked a comparator group. However, there are no official guidelines on cradle cap and a generally accepted reference treatment does not exist. Since cradle cap usually lasts a few weeks or months until it clears by itself it seems very unlikely that cradle cap improved spontaneously in all of the treatment responders (15 of 20 subjects) during the three study days. Therefore, the obtained improvement in scaling is not considered an incidental finding but a result of treatment. Thus, the aim of this study has been reached, i.e., the demonstration of the feasibility of using the IMD as an effective and safe treatment option in cradle cap.
In summary, topically applied, non-medicated LOYON® in the present study has been well tolerated, safe and effective in facilitating the removal of scaling in infants and children with cradle cap. With its gentle approach and rapid effect, LOYON® thus represents a good alternative to home remedies with their unproven safety and efficacy for symptomatic treatment of cradle cap and helps to avoid unnecessary pharmacologically or immunologically active substances in infants and young children, when disease-specific medical treatment is not indicated. Thus, the results of this proof-of-concept study are very promising. They need to be confirmed, however, in larger prospective randomized controlled studies.
Conclusion
This proof-of-concept study provides clinical evidence on the safety and efficacy of the IMD, LOYON® for treatment of cradle cap. LOYON®, at good tolerability, effectively descales cradle cap and may also help to reduce the scale load in other clinical diseases such as seborrheic dermatitis and psoriasis, where efficient removal of scales is not only relevant for cosmetic reasons but may also enable subsequently applied medications to reach their target sites. Further studies with LOYON® are currently undertaken in the indication of psoriasis and show promising first results.
References
Smoker AL. On top of cradle cap. J Fam Health Care. 2007;17(4):134–6.
Steward M. Cradle cap. Community Outlook 1990;18.
Foley P, Zuo Y, Plunkett A, Merlin K, Marks R. The frequency of common skin conditions in preschool-aged children in Australia: seborrheic dermatitis and pityriasis capitis (cradle cap). Arch Dermatol. 2003;139(3):318–22.
Johnson M-LT, Roberts J. Prevalence of dermatological disease among persons 1–74 years of age: United States. Advance data from Vital and Health Statistics National Center for Health Statistics; U S Department of Health, Education, and Welfare 1977;No 4:1–7.
Sachdeva M, Kaur S, Nagpal M, Dewan SP. Cutaneous lesions in new born. Indian J Dermatol Venereol Leprol. 2002;68(6):334–7.
Janniger CK. Infantile seborrheic dermatitis: an approach to cradle cap. Cutis. 1993;51(4):233–5.
O’Connor NR, McLaughlin MR, Ham P. Newborn skin: part I. Common rashes. Am Fam Phys. 2008;77(1):47–52.
Elewski BE. Clinical diagnosis of common scalp disorders. J Investig Dermatol Symp Proc. 2005;10(3):190–3.
McDonald LL, Smith ML. Diagnostic dilemmas in pediatric/adolescent dermatology: scaly scalp. J Pediatr Health Care. 1998;12(2):80–4.
Singleton JK. Pediatric dermatoses: three common skin disruptions in infancy. Nurse Pract. 1997;22(6):32–51.
Arora V, Arora S. Management of infantile seborrheic dermatitis. Am Fam Physician. 2007;75(6):807.
Fleischer AB Jr. Diagnosis and management of common dermatoses in children: atopic, seborrheic, and contact dermatitis. Clin Pediatr (Phila). 2008;47(4):332–46.
Morrell DS, Burkhart CN, Poindexter GB. Therapies for pediatric seborrheic dermatitis. Pediatr Ann. 2009;38(6):333–8.
Zuniga R, Nguyen T. Skin conditions: common skin rashes in infants. FP Essent. 2013;407:31–41.
Sheffield RC, Crawford P, Wright ST, King VJ. Clinical inquiries. What’s the best treatment for cradle cap? J Fam Pract. 2007;56(3):232–3.
Shohat M, Mimouni M, Shuper A, Varsano I. Adrenocortical suppression by topical application of glucocorticosteroids in infants with seborrheic dermatitis. Clin Pediatr (Phila). 1986;25(4):209–12.
Turpeinen M, Lehtokoski-Lehtiniemi E, Leisti S, Salo OP. Percutaneous absorption of hydrocortisone during and after the acute phase of dermatitis in children. Pediatr Dermatol. 1988;5(4):276–9.
Danby SG, AlEnezi T, Sultan A, et al. Effect of olive and sunflower seed oil on the adult skin barrier: implications for neonatal skin care. Pediatr Dermatol. 2013;30(1):42–50.
Siegfried E, Glenn E. Use of olive oil for the treatment of seborrheic dermatitis in children. Arch Pediatr Adolesc Med. 2012;166(10):967.
Williams C. Olive oil for cradle cap? Community Pract. 2010;83(11):14.
Hill K. Industrial development and application of biobased oleochemicals. Pure Appl Chem. 2007;79(11):1999–2011.
Nolan K, Marmur E. Moisturizers: reality and the skin benefits. Dermatol Ther. 2012;25(3):229–33.
Acknowledgments
The author meets the ICMJE criteria for authorship for this manuscript and has given final approval for the version to be published. The clinical investigation reported in the present publication was sponsored by G. Pohl-Boskamp GmbH & Co. KG (Hohenlockstedt, Germany).
Conflict of interest
U. R. Hengge declares that he has no conflict of interest.
Compliance with ethics guidelines
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 and 2008. Informed consent was obtained from all patients for being included in the study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Hengge, U.R. Topical, Non-Medicated LOYON® in Facilitating the Removal of Scaling in Infants and Children with Cradle Cap: a Proof-of-Concept Pilot Study. Dermatol Ther (Heidelb) 4, 221–232 (2014). https://doi.org/10.1007/s13555-014-0060-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-014-0060-3