Abstract
Background
Standard-of-care (SOC) cancer treatments are primarily aimed at reducing size and progression of a tumor. There is a need for successful supplemental anabolic therapies to combat cancer cachexia in addition to these SOC treatment modalities. Anabolic interventions, including testosterone and amino acid supplements, may be beneficial in reducing and/or reversing muscle wasting in these patient populations.
Methods
A 48-year-old Caucasian female with recurrent cervical cancer was scheduled to receive three 21-day cycles of cisplatin and topetecan chemotherapy. She qualified, consented, and enrolled into a blinded interventional pilot study where she received daily whey protein (10 g, three times per day with meals) and a weekly injection of testosterone enanthate (100 mg intramuscular) before and during the SOC chemotherapy treatment period. Body composition, serum inflammatory markers, mixed muscle protein synthesis and breakdown rates, physical function, fatigue, and quality of life were assessed before and after the intervention period.
Results
Body composition, as assessed by an increase in body weight and lean body mass and reduction in fat mass; physical function; fatigue; and quality of life each improved across the entire intervention period despite general increases in inflammatory markers and no improvements in muscle protein turnover towards the end of the intervention.
Conclusions
Concomitant treatment of oral amino acids and testosterone may be a viable therapeutic option for fighting cachexia and improving body composition and quality of life during chemotherapeutic treatment of recurrent cervical cancer. These positive outcomes may be attainable over time despite overall poor inflammatory status.
Similar content being viewed by others
1 Introduction
The rapid loss of fat and lean mass that accompanies cancer is known as cancer cachexia. The loss of muscle mass can be profound, sometimes reaching 75 % of the initial level when the patient has lost 30 % body weight, and is the most phenotypic feature of cancer cachexia [1, 2]. Cachexia affects ~50 % of cancer patients, accounts for ~25 % of cancer deaths, and is one of the principle causes of asthenia, respiratory complications, poor response to chemotherapy, increased susceptibility to infection, and poor quality of life [3–5]. The pathophysiology of cancer cachexia is multifactorial. Underlying mechanisms include systemic inflammation, nutrient scavenging by the tumor and tumor derived factors, decreased dietary intake, and decreased physical activity. Common metabolic abnormalities related to cancer cachexia are altered hormone levels [4, 5], elevated cytokines [3–13], increased muscle proteolysis, and decreased muscle protein synthesis [14]. To date, little success has been achieved toward reversing or preventing cancer cachexia.
The goal of a successful intervention is to reduce skeletal muscle wasting and improve tumor response to suppressive therapy, quality of life, general well-being, and the chance of survival. The response of skeletal muscle to the anabolic stimulus of amino acids is impaired in cachectic cancer patients due to alterations in both processes regulating muscle protein balance (i.e., synthesis vs. breakdown), making it difficult to reach a positive net balance, even acutely. While cancer patients are, at least to a limited extent, anabolically responsive to the intake of balanced amino acids [15], their skeletal muscles exhibit hyperactivation of the muscle proteolytic transcription factor, nuclear factor κB (NFκB), suggesting that the persistent inflammatory state that accompanies cancer contributes to dysregulation of muscle protein breakdown. Combating cancer-related muscle wasting may require combination therapeutic approaches targeted at improving muscle anabolism while reducing catabolism. Therefore, we sought to investigate a targeted nutritional plus hormonal therapy, attempting to maximize chronic anabolic and anticatabolic responses in skeletal muscle while minimizing the volume of the supplement. Whey proteins stimulate food intake and counteract muscle wasting in anorectic weight losing patients [16]. Testosterone also has suppressive actions on muscle proteolysis [17] and has been found capable of reducing systemic inflammatory cytokines, such as TNF-α and IL-6 in humans [18–20], and stimulating the anti-inflammatory cytokine IL-10 [21, 22]. Additionally, the use of anabolic steroids such as testosterone to stimulate protein anabolism in muscle of cancer patients is very promising and clinically relevant [2, 23–25].
Accordingly, we utilized whey protein supplementation and testosterone administration as a combination therapeutic approach in this pilot study on a single patient, with the aim of testing the feasibility and efficacy of this anabolic intervention to reduce skeletal muscle wasting and improve quality of life in recurrent cervical cancer patients undergoing chemotherapy. In addition, we sought to determine potential mechanisms underlying cachexia in this patient population, including the influence of muscle proteolytic factors such as TNF-α and NFκB. Specifically, we determined the effect of nutrition and hormone therapy on lean body mass, muscle strength, fatigue, quality of life, muscle protein synthesis and breakdown, inflammatory biomarkers, and signaling pathways involved in the regulation of muscle atrophy. Data from this single-blinded case study served as pilot data prior to initiation of a larger double-blinded clinical trial aimed at determining whether concomitant administration of testosterone plus whey protein supplement can preserve muscle mass, muscle strength, and quality of life of recurrent cervical cancer patients during the initial rapid loss of body weight and muscle that often accompanies the reinitiation of chemotherapy. We hypothesize that the antianorectic and anticachectic effects of whey proteins and the anabolic and anticatabolic properties of testosterone will enhance lean muscle mass in patients with recurrent cervical cancer by stimulating muscle protein synthesis and inhibiting muscle proteolysis.
2 Methods
2.1 Subject
Inclusion criteria for this intent-to-treat clinical trial were age between 18 and 59 years, diagnosed with recurrent cervical carcinoma, weight loss of 5 % or greater in the past 12 months or a BMI <20 kg/m2, ability to sign consent form (score >23 on the 30-item Mini Mental State Examination, MMSE) and Eastern Cooperative Oncology Group (ECOG) Performance Status of 0 to 2 (0 = fully active, 1 = reduced activity, 2 = inactive but ambulatory, 3 = activity limited to self-care, 4 = completely disabled, 5 = dead) [26]. Exclusion criteria included significant liver, renal, or heart disease; evidence of hepatitis as indicated by a threefold increase in of two out of three liver enzymes; diabetes mellitus or other untreated endocrine disease; recent (within 3 months) treatment with anabolic steroids; alcohol or drug abuse; ongoing anticoagulant therapy; androgen-secreting tumors of the ovary and adrenal or any ovarian tumor (e.g., Sertoli-Leydig); polycystic ovary syndrome (PCOS); and/or hyperthecosis, nonclassical adrenal hyperplasia, Cushing's syndrome, glucocorticoid resistance, pregnancy, hyperprolactinoma, hypothyroidism, lactose intolerance, or any other circumstance deemed exclusionary by the PI or study physician.
A 48-year-old Caucasian female with a past medical history of squamous cell carcinoma of cervix IIB initially diagnosed and treated with external radiation therapy (XRT) and brachytherapy 19 years prior, presented to the oncologist at the University of Texas Medical Branch (UTMB) with recurrent cervical cancer. The patient was having symptoms of gray-colored vaginal discharge along with some weight loss, but denied any vaginal bleeding or abdominal pain. A biopsy showed well-differentiated keratinized squamous cell carcinoma supporting the diagnosis of invasive squamous cell carcinoma, but chest X-ray and MRI of the abdomen/pelvis done at that time showed no evidence of malignancy. However, the patient was not compliant with her follow-up and was seen 7 months later when her performance status on the Gynecologic Oncology Group/Eastern Cooperative Oncology Group (GOG/ECOG) scale was 2 (=inactive but ambulatory) [26]. She was then admitted to receive three 21-day cycles of cisplatin and topotecan chemotherapy. Prior to initiation of her chemotherapy, she consented and enrolled into a 10-week blinded interventional pilot study where she received daily whey protein (10 g protein, three times per day with meals, provided in 12.6 g whey, Optimum Nutrition, Sunrise, FL) and a weekly injection of testosterone enanthate (100 mg intramuscular) before and during the standard-of-care (SOC) chemotherapy treatment. This patient was the first person that was approached by our medical and research team for inclusion in this study.
2.2 Protocol
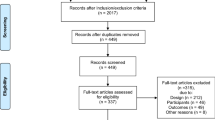
The intent-to-treat interventional protocol was scheduled around the patient's chemotherapy cycles as outlined in Fig. 1. The 10-week protocol was extended to 11 weeks of intervention to accommodate the patient's clinical status as described below. The patient consented within 48 h of diagnosis with recurrent cervical cancer and reported to the Institute for Translational Sciences-Clinical Research Center (ITS-CRC) at the University of Texas Medical Branch (UTMB) the Sunday before her first scheduled cycle of chemotherapy later that week. On the days prior to chemotherapy, fasting baseline blood was collected and the patient completed all measures outlined below. The patient was housed and fed on the ITS-CRC during each week of chemotherapy and returned home the weeks in between. While at home, the patient reported to the ITS-CRC weekly for safety blood draws and to receive an injection of testosterone, a week supply of oral whey protein supplements, a week supply of questionnaires, and an Actigraph activity monitor to be worn continuously until the next visit. Compliance of supplement intake was assessed by weekly bottle counting and encouraged through conversations with the patient.
2.3 Body composition measures
Total body and regional body composition was determined by Dual Energy X-ray Absorptiometry (iDXA, GE Lunar, Waukesha, WI). Regions of interest were automatically generated by the Lunar software as described elsewhere [27]. Where necessary, the automated regions of interest were adjusted by the same qualified technician that completed all scans. For instance, the trunk was defined as the area between the chin, the anterior superior iliac spine, and the humeral heads.
2.4 Blood measures
Total and free testosterone, estradiol, sex hormone-binding globulin (SHBG), cholesterol, HDL, LDL, triglycerides, and cytokines (IL-1β, IL-2, IL-4, IL-5, IL-6, IL-7, IL-8, IL-10, IL-12, IL-13, IFNγ, GM-CSF, and TNFα) were measured in serum. Hormone assays (testosterone and estradiol) were measured with a high-throughput continuous random access immunoassay analyzer (Immulite 2000, Siemens, Deerfield, IL). Serum cytokines were measured by immunoassay using a Millipore Human Cytokine-13 Plex Kit (Millipore, Billerica, MA). All other blood measures were measured and provided by the UTMB Clinical Laboratory.
2.5 Skeletal muscle measures
2.5.1 Mixed muscle fractional synthesis and breakdown rates (FSR and FBR)
Before beginning the stable isotope study, 10 ml of blood was drawn to determine concentrations of amino acids, glucose, hormones, fibrinogen and albumin, cytokines, and the background enrichment of phenylalanine. A bolus injection of 30 cc normal saline and a stable isotope tracer of phenylalanine, ring 13C6-phe (35 μmol/kg body weight), was then given marking time 0 of the 60-min study. Blood samples (5 ml) were drawn at 5, 10, 15, 20, 25, 30, 35, 40, 45, 50, 55, and 60 min after pulse bolus injection from a hand-heated catheter to provide an arterialized sample. Muscle biopsy samples (~200 mg) were taken at 5 and 60 min from a single 5-mm incision in the vastus lateralis of the left limb using a 5-mm Bergström needle. At 30 min, a second bolus containing 15N-phenylalanine (35 μmol/kg body weight) was injected. The injection of multiple tracers combined with arterialized and tissue sampling enables calculation of both the FSR and FBR of mixed muscle protein, as described in Zhang et al. [28].
2.5.2 Protein signaling
Several signaling cascade proteins involved in the regulation of energy and protein metabolism were measured in skeletal muscle tissue. Many anabolic responses, including those to essential amino acids, are mediated through activation of the mTOR signaling pathway [29], which is modulated through both permissive activation by Akt as well as through inhibition by AMPKα when cellular energy status is low. Akt also promotes anabolism through inhibition of catabolic pathways by blocking of GSK3β and by preventing the dephosphorylation and translocation of the catabolic regulators, FoxO1 and FoxO3 [30]. Skeletal muscle myostatin signaling through the activin receptor (ActRIIB) negatively regulates cellular turnover by upregulating Smads 2 and 3. Myostatin signaling has been implicated in TNFα-induced cancer cachexia in rats [31]. Total, and when appropriate, phosphorylated levels of the following proteins were determined using standard Western Blotting techniques: AktSer473, AMPKαThr172, FoxO1Ser256, FoxO3Ser318/321, glycogen synthase kinase 3 (GSKSer9), Smad2Ser465/467, and Smad3Ser423/425.
2.5.3 NF-kB
NFκB activation was measured by detection of p52, (NFκB1), p65 (RelA), p50, and RelB in nuclear extracts using an ELISA kit (Active Motif, Carlsbad, CA).
2.6 Physical function measures
2.6.1 Activity
To monitor total physical activity levels and intensities and to estimate energy expenditure, the patient wore an Actigraph (GTM1/GT3X) accelerometer (ActiGraph, LLC) on her ankle during the entire study [32, 33]. Daily activity data was averaged by week. Data from days with incomplete data collections (<10,000 counts/day) were excluded from analyses.
2.6.2 Resting energy expenditure
Expired gases were collected over 15 min of steady state, and O2 and CO2 concentrations were measured for the determination of resting energy expenditure (SensorMedics, Yorba Linda, CA, USA). Substrate oxidation was measured as described [34].
2.6.3 Muscle strength, power, and fatigue
Isometric and concentric isotonic knee extensor torque was determined using a Biodex System 3 dynamometer (Biodex Medical, New York). The testing protocol was designed with the intent of minimizing patient burden. The patient was seated with the waist as well as the thigh and ankle of the nonbiopsied leg secured with straps. A torso strap was not used in this patient due to the presence of an implanted venous access port (Port-A-Cath®). Following three warm-up repetitions at both 25 % and 50 % of the patient's perceived maximal effort, isometric torque during maximal voluntary contraction (MVC) was determined. All isometric efforts were 5 s in duration, with 15 s of rest between efforts. Following a 2-min rest period, isotonic MVC was similarly determined following three repetitions at both 25 % and 50 % maximal effort, using a load of 20 % of isometric MVC, through a range of motion of 75 ° (from 90 ° to 15 ° of flexion; full extension = 0 ° flexion) using the lateral femoral epicondyle to align the knee joint axis of rotation with the dynamometer axis of rotation, with one effort every 5 s. Gravity correction for the weight of the leg was performed by the Biodex Advantage software program. Following 2 min of rest, the patient performed a series of 25 maximal isotonic contractions at 20 % isometric MVC, with approximately one effort every 2 s. For both isotonic MVC and fatigue testing, loading during flexion was minimized using the Biodex software, and the subject was instructed to let her lower leg passively return to the starting position. Isometric and isotonic MVC were quantified as the peak torque and power, respectively. Skeletal muscle fatigue was evaluated by determining the absolute and relative declines in average power from the initial three to the final three isotonic contractions of the fatigue protocol.
2.6.4 Quality of life
Quality of life was assessed by using the following four questionnaires: (1) Functional Assessment of Cancer Therapy-G (FACT-G) [35] which contains 27 Likert-type items divided over four sections (physical well-being, social/family well-being, emotional well-being, and functional well-being) and (2) Medical Outcomes Study: 36-Item Short Form Survey Instrument (MOS-36) [36]. This questionnaire contains 36 questions to assess physical functioning, role of limitations due to physical health, role of limitations due to emotional problems, energy/fatigue, emotional well-being, social functioning, pain, and general health. (3) Profile of Mood States (POMS) [37] which contains 65 questions to assess six identifiable mood or affective states (tension–anxiety, depression–dejection, anger–hostility, vigor–activity, fatigue–inertia, and confusion–bewilderment) and (4) Multidimensional Fatigue Symptom Inventory-Short Form (MFSI-SF) addressing 30 questions scored to assess general fatigue, physical fatigue, emotional fatigue, mental fatigue, and vigor.
3 Results
3.1 Compliance
There was good compliance with the consumption of the supplement during the at-home periods. All supplement bottles were returned empty.
3.2 Body composition measures
Body weight increased from 40 to 43 kg, total lean mass increased from 26 to 29 kg, and trunk lean mass increased from 13 to 14 kg between baseline and week 11. Total fat mass decreased from 14 to 13 kg and trunk fat mass decreased from 6 to 5 kg during this period.
3.3 Blood measures
Total and free testosterone and estradiol concentrations in the serum increased (Table 1). Cholesterol, triglycerides, HDL, LDL cholesterol, and IGF-1 decreased. Changes in circulating TNF-α, IL-6, IL-7, IL-8, and Il-10 are shown in Table 1. All other cytokines measured remained below the detectable levels of the kit.
3.4 Skeletal muscle measures
3.4.1 Fractional synthesis and breakdown rates (FSR and FBR)
Fasting mixed muscle FSR was unchanged, but FBR was higher during the 1-h measurement after the intervention period compared to baseline (Table 1).
3.4.2 Signaling
Protein expression of skeletal muscle Akt and Smad3 were higher at week 11 when compared to baseline. There were no notable changes in the expression of AMPKα, FoxO1, FoxO3, GSK, or Smad2 (Table 1).
3.4.3 Cytokines
Canonical NFκB activation (nuclear p52 and RelA content) increased and noncanonical NFκB activation (nuclear p50 and RelB content) decreased (Fig. 2).
3.5 Physical function measures
3.5.1 Activity
Actigraph data indicated low levels of daily activity when the patient entered the study (26,853 ± 5,175 counts/day during the first week) when compared to healthy ambulatory individuals (>250,000 counts/day) as measured by us (unpublished data) and others [38] (Fig. 3). The patient increased her daily activity by week 5 (45,200 ± 3,075 counts/day) which was maintained through week 7, but returned to baseline before the completion of the intervention period (23,459 ± 2,137 counts/day during week 10). The weekly averages of the peak activity recorded during a single minute each day are also shown in Fig. 3. Because the assumption was made that daily counts <10,000 were due to incomplete data collections and were thus excluded from further analyses, it remains possible that the data presented are overestimations of actual activity levels.
Physical activity. Total daily activity was averaged for each week during 10 weeks of observation. Peak activities shown are the means of the highest activity recorded during a single minute within each day of the week. Data from days with incomplete data collections (<10,000 counts/day) were excluded from analyses
3.5.2 Resting energy expenditure
Resting oxygen consumption did not change from baseline to the end of the intervention (3.60 ± 0.02 vs. 3.65 ± 0.08 ml kg−1 min−1).
3.5.3 Muscle strength, power and fatigue
Peak isometric torque (Fig. 4a) and peak isotonic power increased (Fig. 4b). Relative muscle fatigability (final three contractions of the fatigue protocol compared to the first three contractions) improved from 20 % at baseline to 5 % in week 10 (Fig. 4c). Moreover, average peak isotonic power during the first three contractions of the fatigue protocol was increased by 40 % after 11 weeks when compared to baseline and average peak isotonic power during the last three contractions was increased by 70 % (not shown).
3.5.4 Quality of life
Self-reported quality of life improved as indicated by increased scores on the FACT-G and MOS-36, decreased affective mood scores on the POMS, and reduced fatigue according to the MSFI-SF (Table 2) [39–42].
3.6 Clinical notes and follow-up
The patient received chemotherapy in weeks 1, 4, and 7 of the study period. During the study period, the patient reported to the ITS-CRC with nausea and lack of appetite in week 3, flulike symptoms in week 5, sleep disturbances and lack of appetite in week 6, and was admitted to the hospital in week 9 for nausea, vomiting and fever. At week 10, she again presented with nausea, vomiting, and fever and was diagnosed with acute hepatitis C, and the patient was hospitalized. For this reason, her final chemotherapy session was postponed for a week and the interventional period was extended to 11 weeks. There were no signs of virilization at any time.
A large cavitating pelvic mass, identified to be the cervical carcinoma by CT and MRI of the abdomen/pelvis, had been stable in size during the previous 5 years. However, during the first week of chemotherapy, increased inflammation, fluid, and air were noted, which may have been a local extension of tumor or an abscess. The possibility of local extension was not evident in later CT scans during week 9.
The patient had a past history of lymphadenopathy in the inguinal area; however, these lymph nodes remained stable in size and distribution, and a biopsy 1 year prior to this study showed reactive lymphoid tissue but no neoplastic changes. Repeated chest X-ray and CT scans of the thorax/abdomen/pelvis did not reveal any obvious distant metastases. There likely was a partial response to chemotherapy as pelvic mass did not change in size throughout the course of the chemotherapy, no significant changes in lymphadenopathy or lymphatic spread of the cancer were noted, and no proven or definitive metastases were identified during and up to 6 weeks following conclusion of the study.
Monthly follow-ups were conducted by phone after the final test sessions were completed at week 11. Phone follow-ups were planned for up to 1 year following completion of the protocol and consisted of informal conversations with the patient to inquire about general well-being and quality of life. Four weeks after discontinuation of the intervention, the patient entered hospice care. The patient died 10 weeks following discontinuation of intervention (i.e., ~5 months from diagnosis/enrollment).
4 Discussion
4.1 Summary of findings
There is a substantial direct benefit in maintaining muscle function and mass during treatment protocols targeted at decreasing tumor size. Even successful chemotherapy often imparts an additional physiological and psychological burden to the patient such as reduced appetite, limited physical activity, and overall decreased quality of life. Targeted nutritional and/or hormonal therapies in conjunction with antitumor therapy may be beneficial in improving long-term survival of patients. In this study, we found that concomitant treatment with oral amino acids and testosterone improved functional measures such as muscle strength, power, and fatigue as well as quality of life in a patient undergoing chemotherapeutic treatment of recurrent cervical cancer. These improvements were associated with increased body weight, increased lean body mass, and decreased fat mass, which occurred despite low daily activity levels and a poor inflammatory status.
4.2 Nutrition and cancer
Cancer cachexia is a complex phenomenon involving both tumor-derived factors and systemic factors including hormones and mediators of inflammation. While cancer-associated malnutrition cannot be explained by poor nutritional intake alone, early nutritional support is paramount to prevent or retard the downward spiral of malnutrition and to improve quality of life and chance of survival [5]. Along with strategies to maintain appetite and adequate food intake, nutrient composition must be optimized to maximally induce skeletal muscle anabolism with minimal volume of food intake. Our group recently reported that skeletal muscle of ovarian cancer patients is anabolically responsive, albeit with reduced sensitivity, to oral amino acid supplementation, despite the presence of systemic inflammation [15]. The whey protein supplement used in the present study provided an over-the-counter approach that delivered the essential amino acids previously shown to improve (increase) skeletal muscle protein balance. In the present case, the patient reportedly enjoyed the whey protein supplement, which was provided in powdered form to be mixed with a beverage of the patient's choice. Although the relative effects of the whey protein supplement and the concurrently administered testosterone on muscle anabolism and catabolism cannot be distinguished in the present case, we investigated a panel of signaling pathways previously implicated in muscle anabolism and catabolism. In the present case, basal Akt and Smad3 were elevated in cytosolic fractions following the 11-week intervention period, but there were no changes in AMPKα, Smad2, FoxO1, FoxO3, or GSK. Notably, these responses to the therapeutic regimen only reflect the fasting state under which the muscle biopsies were taken. As accrual or loss of skeletal muscle mass is dependent on the integrated net balance between muscle protein synthesis and breakdown over time, complementary studies under fasting and fed conditions will be necessary to determine which signaling pathways play an important role.
4.3 Hormones and inflammation
Elevation of skeletal muscle IGF-1 production with testosterone therapy and subsequent suppression of protein breakdown has indicated that testosterone exerts anticatabolic properties [17]. Testosterone has been shown to reduce inflammatory cytokines such as TNF-α, IL-6, and IL-1B in humans [18–20]. Androgen treatment has been shown to interfere with canonical [43], but not noncanonical [44], NF-kB signaling in prostate cancer cell lines and repress IL-6 expression [45]. However, the role of NF-kB signaling in the regulation of skeletal muscle protein is complex and not well understood [46]. The leading explanation for the increase in canonical NF-kB proteins (p50/RelA) in the present study is the increased inflammatory burden of the patient towards the end of her chemotherapy treatment period, in part aggravated by acute hepatitis C. Activation of transcription factors like NF-kB by cytokines, such as TNF-α and proteolysis-inducing factor (PIF), is a first and important step for NF-kB-induced muscle proteolysis and apoptosis [47–51]. However, as we did not measure all possible activators of NF-kB signaling, it remains unclear what the direct driving factors were for the observed changes in NF-kB signaling. We noted no increases in circulating inflammatory signals, such as TNF-α or IL-1, at the time of biopsy. In contrast to the catabolic role sometimes ascribed to NF-kB, another model of skeletal muscle NF-kB signaling suggests a role of the canonical pathway (p50/RelA) in stimulating myogenesis, while the noncanonical pathway (p52/RelB) may be subsequently involved in mitochondrial biogenesis within the differentiated myotubes [52]. Activation of p50/RelA increases production of IL-6, a potential important regulator during skeletal muscle differentiation [53]. This cytokine is acutely upregulated in skeletal muscle following exercise where it may play a physiological role (myokine) in skeletal muscle anabolism [54]. In contrast, chronic systemic elevation of IL-6 is often found in catabolic disease states such as cancer cachexia, and elevations of IL-6 in late stage cachectic patients have been reported in the absence of elevated TNF-α [55]. Increases in serum IL-6 during cisplatin-based chemotherapy do not necessarily correlate to tumor size in cervical cancer [56]. However, we should acknowledge that the cytokines measured mediate numerous other responses and thus further studies are necessary to verify and further elucidate the role of NF-KB in human cancer patients. The data from the single patient reported here and the clinical complications that presented near the final data collection period are insufficient to unequivocally support any one of the possible roles of NF-kB in regulation of muscle mass and thus completion of additional subjects receiving SOC treatment either with or without anabolic support will be needed to clarify the mechanisms most likely involved. The diagnosis of acute hepatitis C towards the conclusion of our study timeframe is likely to be a major contributing factor to the increased inflammatory state and may be responsible for the acute measurements of decreased serum IGF-1 concentrations [57] and increased protein breakdown despite maintenance of LBM and muscle strength measured across the entire treatment period. Furthermore, while testosterone is considered to be protective against inflammation, more subjects are needed in the ongoing double-blinded placebo-controlled study to ascertain whether testosterone administration can demonstrate anti-inflammatory benefits in this patient population.
4.4 Goal of intervention
Successful nutrition/hormone therapy must demonstrate effectiveness in maintaining or improving functional outcomes without negatively affecting ongoing tumor-suppressive therapies. We elected to use SOC male hormone replacement doses in order to treat this female patient with supraphysiologic testosterone doses. We selected this treatment paradigm because this was a terminal patient, and our goal was to maximize the hormonal response. We understand that if testosterone is considered a therapy in women without a terminal condition, additional consideration should be given to the dose and duration of testosterone used to minimize virilization and other side effects such as the significant lowering of the patients HDL with the testosterone injections. Tumor size, as assessed by CT and pelvic examinations, did not change during treatment in this patient. Although not observed in this patient, in response to the combination therapy of whey protein and testosterone, it is important to monitor patients for sudden unforeseen changes in tumor size. However, incidence of this risk is expected to be minimal in the context of the testosterone intervention, since the expression of androgen receptor is generally much lower in cervical carcinomas when compared to normal epithelium [58]. Similarly, we do not know whether, or how, the supplemental therapy affects patient survival. Up to 30 % of cervical patients do not survive longer than 6 months following diagnosis and the onset of cisplatin + topetecan based-therapy [59].
5 Conclusion
The goal of a supplemental intervention is ultimately to improve quality of life, performance status, and chance of survival of the patient beyond that which is achieved with standard of care chemotherapy alone. Concomitant treatment of oral amino acids and testosterone may be a viable therapeutic option for fighting cachexia and improving body composition and quality of life during chemotherapeutic treatment of recurrent cervical cancer. In the case study we present here, we utilized a combination therapy approach of oral whey protein plus testosterone to improve muscle mass and quality of life during chemotherapy in a patient with recurrent cervical cancer. Clearly, a larger cohort is needed to determine whether such supplemental treatment approaches are efficacious over the long-term in improving body composition, physical function, quality of life, and cancer survival of cachectic patients when compared to standard of care alone. A double-blinded, placebo-controlled interventional study is in progress (NCT00878995).
References
Fearon KC. The Sir David Cuthbertson Medal Lecture 1991. The mechanisms and treatment of weight loss in cancer. Proc Nutr Soc. 1991;51:251–65.
Muscaritoli M, Bossola M, Aversa Z, Bellantone R, Rossi Fanelli F. Prevention and treatment of cancer cachexia: new insights into an old problem. Eur J Cancer. 2006;42:31–41.
Argiles JM, Busquets S, Lopez-Soriano FJ. The pivotal role of cytokines in muscle wasting during cancer. Int J Biochem Cell Biol. 2005;37:1609–19.
Gordon JN, Green SR, Goggin PM. Cancer cachexia. QJM. 2005;98:779–88.
Argiles JM. Cancer-associated malnutrition. Eur J Oncol Nurs. 2005;9:S39–50.
Argiles JM, Busquets S, Garcia-Martinez C, Lopez-Soriano FJ. Mediators involved in the cancer anorexia–cachexia syndrome: past, present, and future. Nutrition. 2005;21:977–85.
Argiles JM, Busquets S, Felipe A, Lopez-Soriano FJ. Molecular mechanisms involved in muscle wasting in cancer and ageing: cachexia versus sarcopenia. Int J Biochem Cell Biol. 2005;37:1084–104.
Chamberlain JS. Cachexia in cancer—zeroing in on myosin. N Engl J Med. 2004;351:2124–5.
Deans C, Wigmore SJ. Systemic inflammation, cachexia and prognosis in patients with cancer. Curr Opin Clin Nutr Metab Care. 2005;8:265–9.
DeJong CH, Busquets S, Moses AG, Schrauwen P, Ross JA, Argiles JM, Fearon KC. Systemic inflammation correlates with increased expression of skeletal muscle ubiquitin but not uncoupling proteins in cancer cachexia. Oncol Rep. 2005;14:257–63.
Martignoni ME, Kunze P, Hildebrandt W, Kunzli B, Berberat P, Giese T, Kloters O, Hammer J, Buchler MW, Giese NA, Friess H. Role of mononuclear cells and inflammatory cytokines in pancreatic cancer-related cachexia. Clin Cancer Res. 2005;11:5802–8.
Tisdale MJ. Molecular pathways leading to cancer cachexia. Physiology (Bethesda). 2005;20:340–8.
Tisdale MJ. Wasting in cancer. J Nutr. 1999;129:243S–6.
Emery PW, Edwards RH, Rennie MJ, Souhami RL, Halliday D. Protein synthesis in muscle measured in vivo in cachectic patients with cancer. Br Med J (Clin Res Ed). 1984;289:584–6.
Dillon EL, Volpi E, Wolfe RR, Sinha S, Sanford AP, Arrastia CD, Urban RJ, Casperson SL, Paddon-Jones D, Sheffield-Moore M. Amino acid metabolism and inflammatory burden in ovarian cancer patients undergoing intense oncological therapy. Clin Nutr. 2007;26:736–43.
Cangiano C, Laviano A, Meguid MM, Mulieri M, Conversano L, Preziosa I, Rossi-Fanelli F. Effects of administration of oral branched-chain amino acids on anorexia and caloric intake in cancer patients. J Natl Cancer Inst. 1996;88:550–2.
Ferrando AA, Sheffield-Moore M, Yeckel CW, Gilkison C, Jiang J, Achacosa A, Lieberman SA, Tipton K, Wolfe RR, Urban RJ. Testosterone administration to older men improves muscle function: molecular and physiological mechanisms. Am J Physiol Endocrinol Metab. 2002;282:E601–7.
Khosla S, Atkinson EJ, Dunstan CR, O'Fallon WM. Effect of estrogen versus testosterone on circulating osteoprotegerin and other cytokine levels in normal elderly men. J Clin Endocrinol Metab. 2002;87:1550–4.
Malkin CJ, Pugh PJ, Jones RD, Kapoor D, Channer KS, Jones TH. The effect of testosterone replacement on endogenous inflammatory cytokines and lipid profiles in hypogonadal men. J Clin Endocrinol Metab. 2004;89:3313–8.
Yesilova Z, Ozata M, Kocar IH, Turan M, Pekel A, Sengul A, Ozdemir IC. The effects of gonadotropin treatment on the immunological features of male patients with idiopathic hypogonadotropic hypogonadism. J Clin Endocrinol Metab. 2000;85:66–70.
Liva SM, Voskuhl RR. Testosterone acts directly on CD4+ T lymphocytes to increase IL-10 production. J Immunol. 2001;167:2060–7.
Bebo Jr BF, Schuster JC, Vandenbark AA, Offner H. Androgens alter the cytokine profile and reduce encephalitogenicity of myelin-reactive T cells. J Immunol. 1999;162:35–40.
Acharyya S, Butchbach ME, Sahenk Z, Wang H, Saji M, Carathers M, Ringel MD, Skipworth RJ, Fearon KC, Hollingsworth MA, Muscarella P, Burghes AH, Rafael-Fortney JA, Guttridge DC. Dystrophin glycoprotein complex dysfunction: a regulatory link between muscular dystrophy and cancer cachexia. Cancer Cell. 2005;8:421–32.
Chlebowski RT, Herrold J, Ali I, Oktay E, Chlebowski JS, Ponce AT, Heber D, Block JB. Influence of nandrolone decanoate on weight loss in advanced non-small cell lung cancer. Cancer. 1986;58:183–6.
Lambert CP, Sullivan DH, Evans WJ. Effects of testosterone replacement and/or resistance training on interleukin-6, tumor necrosis factor alpha, and leptin in elderly men ingesting megestrol acetate: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2003;58:165–70.
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649–55.
Kim J, Wang Z, Heymsfield SB, Baumgartner RN, Gallagher D. Total-body skeletal muscle mass: estimation by a new dual-energy X-ray absorptiometry method. Am J Clin Nutr. 2002;76:378–83.
Zhang XJ, Chinkes DL, Wolfe RR. Measurement of muscle protein fractional synthesis and breakdown rates from a pulse tracer injection. Am J Physiol Endocrinol Metab. 2002;283:E753–64.
Rennie MJ, Bohe J, Smith K, Wackerhage H, Greenhaff P. Branched-chain amino acids as fuels and anabolic signals in human muscle. J Nutr. 2006;136:264S–8.
Sandri M. Signaling in muscle atrophy and hypertrophy. Physiology (Bethesda). 2008;23:160–70.
Costelli P, Muscaritoli M, Bonetto A, Penna F, Reffo P, Bossola M, Bonelli G, Doglietto GB, Baccino FM, Rossi Fanelli F. Muscle myostatin signalling is enhanced in experimental cancer cachexia. Eur J Clin Invest. 2008;38:531–8.
Crouter SE, Clowers KG, Bassett Jr DR. A novel method for using accelerometer data to predict energy expenditure. J Appl Physiol. 2006;100:1324–31.
Pober DM, Staudenmayer J, Raphael C, Freedson PS. Development of novel techniques to classify physical activity mode using accelerometers. Med Sci Sports Exerc. 2006;38:1626–34.
Frayn KN. Calculation of substrate oxidation rates in vivo from gaseous exchange. J Appl Physiol. 1983;55:628–34.
Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, Silberman M, Yellen SB, Winicour P, Brannon J, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol. 1993;11:570–9.
Jenkinson C, Wright L, Coulter A. Criterion validity and reliability of the SF-36 in a population sample. Qual Life Res. 1994;3:7–12.
Curran SL, Andrykowski MA, Studts JL. Short form of the profile of mood states: psychometric information. Psychol Assess. 1995;7:80–3.
Bratland-Sanda S, Sundgot-Borgen J, Ro O, Rosenvinge JH, Hoffart A, Martinsen EW. “I'm not physically active—I only go for walks”: physical activity in patients with longstanding eating disorders. Int J Eat Disord. 2010;43:88–92.
Cella D, Zagari MJ, Vandoros C, Gagnon DD, Hurtz HJ, Nortier JW. Epoetin alfa treatment results in clinically significant improvements in quality of life in anemic cancer patients when referenced to the general population. J Clin Oncol. 2003;21:366–73.
Noble M, Russell C, Kraemer L, Sharratt M. UW WELL-FIT: the impact of supervised exercise programs on physical capacity and quality of life in individuals receiving treatment for cancer. Support Care Cancer. 2011;20:865–73.
Ohnishi N, Kataoka T, Okamura H. Relationships between roles and mental states and role functional QOL in breast cancer outpatients. Jpn J Clin Oncol. 2011;41:1112–8.
Prue G, Rankin J, Cramp F, Allen J, Gracey J. Fatigue in gynaecological cancer patients: a pilot study. Support Care Cancer. 2006;14:78–83.
Altuwaijri S, Lin HK, Chuang KH, Lin WJ, Yeh S, Hanchett LA, Rahman MM, Kang HY, Tsai MY, Zhang Y, Yang L, Chang C. Interruption of nuclear factor kappaB signaling by the androgen receptor facilitates 12-O-tetradecanoylphorbolacetate-induced apoptosis in androgen-sensitive prostate cancer LNCaP cells. Cancer Res. 2003;63:7106–12.
Lessard L, Saad F, Le Page C, Diallo JS, Peant B, Delvoye N, Mes-Masson AM. NF-kappaB2 processing and p52 nuclear accumulation after androgenic stimulation of LNCaP prostate cancer cells. Cell Signal. 2007;19:1093–100.
Keller ET, Chang C, Ershler WB. Inhibition of NFkappaB activity through maintenance of IkappaBalpha levels contributes to dihydrotestosterone-mediated repression of the interleukin-6 promoter. J Biol Chem. 1996;271:26267–75.
Bakkar N, Guttridge DC. NF-kappaB signaling: a tale of two pathways in skeletal myogenesis. Physiol Rev 2010;90:495–511.
Wyke SM, Tisdale MJ. NF-kappaB mediates proteolysis-inducing factor induced protein degradation and expression of the ubiquitin-proteasome system in skeletal muscle. Br J Cancer. 2005;92:711–21.
Ladner KJ, Caligiuri MA, Guttridge DC. Tumor necrosis factor-regulated biphasic activation of NF-kappa B is required for cytokine-induced loss of skeletal muscle gene products. J Biol Chem. 2003;278:2294–303.
Burckart K, Beca S, Urban RJ, Sheffield-Moore M. Pathogenesis of muscle wasting in cancer cachexia: targeted anabolic and anticatabolic therapies. Curr Opin Clin Nutr Metab Care. 2010;13:410–6.
Saini A, Faulkner S, Al-Shanti N, Stewart C. Powerful signals for weak muscles. Ageing Res Rev. 2009;8:251–67.
Zhang P, Chen X, Fan M. Signaling mechanisms involved in disuse muscle atrophy. Med Hypotheses. 2007;69:310–21.
Bakkar N, Guttridge DC. NF-kappaB signaling: a tale of two pathways in skeletal myogenesis. Physiol Rev. 2010;90:495–511.
Baeza-Raja B, Munoz-Canoves P. p38 MAPK-induced nuclear factor-kappaB activity is required for skeletal muscle differentiation: role of interleukin-6. Mol Biol Cell. 2004;15:2013–26.
Nielsen AR, Pedersen BK. The biological roles of exercise-induced cytokines: IL-6, IL-8, and IL-15. Appl Physiol Nutr Metab. 2007;32:833–9.
Iwase S, Murakami T, Saito Y, Nakagawa K. Steep elevation of blood interleukin-6 (IL-6) associated only with late stages of cachexia in cancer patients. Eur Cytokine Netw. 2004;15:312–6.
Yang YC, Wang KL, Su TH, Liao HF, Wu MH, Chen TC, Huang MC, Chen YJ. Concurrent cisplatin-based chemoradiation for cervical carcinoma: tumor response, toxicity, and serum cytokine profiles. Cancer Invest. 2006;24:390–5.
Helaly GF, Hussein NG, Refai W, Ibrahim M. Relation of serum insulin-like growth factor-1 (IGF-1) levels with hepatitis C virus infection and insulin resistance. Transl Res. 2011;158:155–62.
Noel JC, Bucella D, Fayt I, Simonart T, Buxant F, Anaf V, Simon P. Androgen receptor expression in cervical intraepithelial neoplasia and invasive squamous cell carcinoma of the cervix. Int J Gynecol Pathol. 2008;27:437–41.
Long 3rd HJ, Bundy BN, Grendys Jr EC, Benda JA, McMeekin DS, Sorosky J, Miller DS, Eaton LA, Fiorica JV. Randomized phase III trial of cisplatin with or without topotecan in carcinoma of the uterine cervix: a Gynecologic Oncology Group Study. J Clin Oncol. 2005;23:4626–33.
von Haehling S, Morley JE, Coats AJS, Anker SD. Ethical guidelines for authorship and publishing in the Journal of Cachexia, Sarcopenia and Muscle. J Cachex Sarcopenia Muscle. 2010;1:7–8.
Acknowledgments
The authors of this manuscript certify that they comply with the principles of ethical publishing in the Journal of Cachexia, Sarcopenia and Muscle [60]. This study was funded through NIH/NCI RO1 CA127971 (Sheffield-Moore).
Conflict of interest
The authors declare that they have no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Dillon, E.L., Basra, G., Horstman, A.M. et al. Cancer cachexia and anabolic interventions: a case report. J Cachexia Sarcopenia Muscle 3, 253–263 (2012). https://doi.org/10.1007/s13539-012-0066-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13539-012-0066-6