Abstract
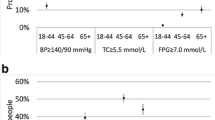
Starting in 2006, respondents in the biennial U.S. Health and Retirement Study were asked to submit biomarkers every other wave and were notified of several results. Rates of undiagnosed high blood pressure and diabetes according to these biomarkers were 1.5 % and 0.7 %, respectively. An intent-to-treat analysis suggests that collection and notification had small effects on the average respondent and may have reduced health care utilization. Among respondents who received notification of potentially dangerous biomarker levels, subsequent rates of new diagnosis and associated pharmaceutical usage increased by 20 to 40 percentage points, an order of magnitude above baseline. High blood glucose A1C was associated with a 2.2 % drop in weight and an increase in exercise among respondents without a previous diagnosis of diabetes. Notifications appear also to have altered health behaviors by spouses, suggesting household responses to health maintenance. Biomarker collection seems to have altered circumstances for an interesting minority of HRS respondents.



Similar content being viewed by others
Notes
The National Health and Nutrition Examination Survey (NHANES) notifies participants of a wide array of biomarker levels, including overweight, blood pressure, and oral health. Exploiting the random assignment of respondents to morning exams, when biomarkers that require fasting could be collected, Singleton (2013) found evidence that retirement behavior reacts to biomarker notification in the NHANES. The National Longitudinal Study of Adolescent Health (Add Health) collected biomarkers in its third wave and notified respondents of results of testing for HIV, chlamydia, and gonorrhea. By contrast, the Demographic and Health Surveys (DHS) measure HIV status in developing countries but explicitly do not inform respondents about results, ostensibly to preserve anonymity and respondents’ safety. Instead, DHS participants are offered referrals for free counseling and testing.
Participation in a panel study can change some types of behavior under certain conditions (Halpern-Manners and Warren 2012). Here, the possibility that observation becomes a treatment seems more likely than in standard cases of panel conditioning because the motivating presumption of the IRB is that information about risky levels of biomarkers should affect behavior and outcomes.
Case and Deaton (2015) identified significant and rising excess mortality among white non-Hispanic Americans aged 45–54. Chronic pain and misuse of prescribed opioids—or “too much care”—could be the culprit, suggesting that increased screening might even exacerbate the problem. However, Meara and Skinner (2015) pointed out that increasingly elevated mortality among this subgroup is not confined to diseases related to excessive drinking and drug use; it is also spread across causes such as cardiovascular disease and diabetes, precisely the targets of screenings considered here.
Compared with the likely costs involved with a blanket extension of such services, the benefits seem minimal without targeting.
Although respondents in group A2008 submitted biomarkers two years later in 2008, it is unclear whether their 2008 biomarkers would be good proxies for what their 2006 biomarkers would have been. The persistence of biomarkers over the life course, which likely depends both on biological and on socioeconomic conditions, is unknown. If high blood pressure, A1C, and cholesterol are chronic and stable among those undiagnosed, and if those undiagnosed in the HRS tend to remain undiagnosed, then the 2008 biomarker levels would be good proxies for the 2006 levels among the key subgroup A2008 − B2008. However, it is easy to speculate otherwise. Even if it were feasible, a direct comparison of A2006 with A2008 in 2006 is polluted by mode-of-interview effects because the latter is almost exclusively assessed via telephone interview. See the next section for an expanded discussion.
I restrict attention to respondents who appeared in both the 2006 and 2008 waves. This restriction effectively drops approximately 10 % of the sample submitting biomarkers across the board, of whom typically 6 % had died and the other 4 % were in nonresponse. As I discuss shortly, there did not appear to be substantial differences in attrition or mortality across these groups defined by biomarker results by 2008.
For the current level of condition diagnosis here and in the panel FE analysis later, I use the raw responses, in which respondents can dispute records from past waves. In Table 1, the change in diagnosis is calculated using the current statements about present and past diagnosis. Differences between these data definitions are minimal and do not appreciably affect results.
I use the same covariates shown in Table 2 plus nine indicators of diagnosed health conditions: high blood pressure, diabetes, cancer, lung disease, heart problems, stroke, psychological problems, memory-related disease, and arthritis. Results are available upon request.
Rosero-Bixby and Dow (2012) revealed significant effects of biomarkers on mortality in a Costa Rican panel. However, scoring above particular thresholds of biomarkers did not affect mortality and other forms of attrition over two years in the HRS, even though the levels of A1C and total cholesterol were significant predictors of death by 2008. Presumably, the information contained in the thresholds alone was picked up well by other covariates, such as health conditions.
The cause is unknown and seems worthy of future inquiry, but the size of the effect is small enough to complicate investigation. One might have expected to see the reverse—that assignment to the 2008 biomarker group would have reduced nonresponse because of efforts by interviewers to obtain the measures.
Previous knowledge of high blood pressure and diabetes can be defined by whether the respondent is taking the associated medicine. Results based on that definition are similar to those reported here.
All regressions in Tables 3–6 are linear, including those modeling dichotomous outcomes. As shown in Table 1, these outcomes tend to be quite common in the sample, removing a typical concern about applying the linear probability model. An additional motivation for using the linear model, aside from its more straightforward asymptotic characteristics in the presence of fixed effects, is that interaction terms are better defined. Results of logit models were consistent with those of the linear probability model.
The average number of doctor visits since the previous wave does not respond significantly (not shown), which could be consistent with small changes in the prevalence of a common event like this.
The large and significant negative coefficients here on abnormal cholesterol screens among those who were already taking those medications are real. These subgroups report less than 100 % usage in 2008 for unknown reasons. Given that the notification thresholds in question are not extreme, one interpretation is that the notification is not a good indicator of a persistent condition in these cases.
References
Banks, J., Muriel, A., & Smith, J. P. (2010). Attrition and health in ageing studies: Evidence from ELSA and HRS. Longitudinal and Life Course Studies, 2, 101–126.
Bindman, A. B., Grumbach, K., Osmond, D., Komaromy, M., Vranizan, K., Lurie, N., . . . Stewart, A. (1995). Preventable hospitalizations and access to health care. JAMA, 274, 305–311.
Boozer, M. A., & Philipson, T. J. (2000). The impact of public testing for human immunodeficiency virus. Journal of Human Resources, 35, 419–446.
Case, A., & Deaton, A. (2015). Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proceedings of the National Academy of Sciences, 112, 15078–15083.
Chetty, R., Stepner, M., Abraham, S., Lin, S., Scuderi, B., Turner, N., . . . Cutler, D. (2016). The association between income and life expectancy in the United States, 2001–2014. JAMA, 315, 1750–1766.
Delavande, A., & Kohler, H.-P. (2012). The impact of HIV testing on subjective expectations and risky behavior in Malawi. Demography, 49, 1011–1036.
Falba, T. A., & Sindelar, J. L. (2008). Spousal concordance in health behavior change. Health Services Research, 43, 96–116.
Godlonton, S., & Thornton, R. L. (2013). Learning from others’ HIV testing: Updating beliefs and responding to risk. American Economic Review: Papers & Proceedings, 103, 439–444.
Goldman, D. P., & Smith, J. P. (2002). Can patient self-management help explain the SES health gradient? Proceedings of the National Academy of Sciences, 99, 10929–10934.
Goldman, N. (1993). Marriage selection and mortality patterns: Inferences and fallacies. Demography, 30, 189–208.
Gong, E. (2015). HIV testing and risky sexual behavior. Economic Journal, 125, 32–60.
Guner, N., Kulikova, Y., & Llull, J. (2014). Does marriage make you healthier? (IZA Discussion Paper No. 8633). Bonn, Germany: Institute for the Study of Labor.
Gunton, J. E., Davies, L., Wilmshurst, E., Fulcher, G., & McElduff, A. (2002). Cigarette smoking affects glycemic control in diabetes. Diabetes Care, 25, 796–797.
Halpern-Manners, A., & Warren, J. R. (2012). Panel conditioning in longitudinal studies: Evidence from labor force items in the Current Population Survey. Demography, 49, 1499–1519.
Hu, Y., & Goldman, N. (1990). Mortality differentials by marital status: An international comparison. Demography, 27, 233–250.
Jiang, H. J., Russo, C. A., & Barrett, M. L. (2009). Nationwide frequency and costs of potentially preventable hospitalizations, 2006 (Healthcare Cost and Utilization Project Statistical Brief No. 72). Rockville, MD: U.S. Agency for Healthcare Research and Quality. Retrieved from http://www.hcup-us.ahrq.gov/reports/statbriefs/sb72.pdf
Juster, F. T., & Suzman, R. (1995). An overview of the Health and Retirement Study. Journal of Human Resources, 30(Suppl.), S7–S56.
Meara, E., & Skinner, J. (2015). Losing ground at midlife in America. Proceedings of the National Academy of Sciences, 112, 15006–15007.
Reczek, C., & Umberson, D. (2012). Gender, health behavior, and intimate relationships: Lesbian, gay, and straight contexts. Social Science & Medicine, 74, 1783–1790.
Rendall, M. S., Weden, M. M., Favreault, M. M., & Waldron, H. (2011). The protective effect of marriage for survival: A review and update. Demography, 48, 481–506.
Rosero-Bixby, L., & Dow, W. H. (2012). Predicting mortality with biomarkers: A population-based prospective cohort study for elderly Costa Ricans. Population Health Metrics, 10, 1–15. https://doi.org/10.1186/1478-7954-10-11.
Sattar, N., Preiss, D., Murray, H. M., Welsh, P., Buckley, B. M., de Craen, A. J., . . . Ford, I. (2010). Statins and risk of incident diabetes: A collaborative meta-analysis of randomized statin trials. Lancet, 375, 735–742.
Singleton, P. (2013). Health information and Social Security entitlements (Center for Policy Research Working Paper No. 164). Syracuse, NY: Syracuse University.
Stevenson, B., & Wolfers, J. (2007). Marriage and divorce: Changes and their driving forces. Journal of Economic Perspectives, 21(2), 27–52.
Thornton, R. L. (2008). The demand for, and impact of, learning HIV status. American Economic Review, 98, 1829–1863.
Thornton, R. L. (2012). HIV testing, subjective beliefs and economic behavior. Journal of Development Economics, 99, 300–313.
Umberson, D., Crosnoe, R., & Reczek, C. (2010). Social relationships and health behavior across life course. Annual Review of Sociology, 36, 139–157.
Weinstein, M., Vaupel, J. W., & Wachter, K. W. (Eds.). (2007). Biosocial surveys. Washington, DC: National Academies Press.
Weir, D. (2007). Elastic powers: The integration of biomarkers into the Health and Retirement Study. In M. Weinstein, J. W. Vaupel, & K. W. Wachter (Eds.), Biosocial surveys (pp. 78–95). Washington, DC: National Academies Press.
Weir, D. R. (2010, April). Socio-economic status and mortality: Perceptions and outcomes. Paper presented at the annual meeting of the Population Association of America, Dallas, TX.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
ESM 1
(PDF 639 kb)
Rights and permissions
About this article
Cite this article
Edwards, R.D. If My Blood Pressure Is High, Do I Take It to Heart? Behavioral Effects of Biomarker Collection in the Health and Retirement Study. Demography 55, 403–434 (2018). https://doi.org/10.1007/s13524-018-0650-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13524-018-0650-2