Abstract
Objective
Gestational diabetes mellitus (GDM) is a type of diabetes that occurs during pregnancy which is becoming increasingly prevalent worldwide. Notably, recent studies have shown that differences in the distribution of gut microflora are strongly associated with the pathogenesis and progression of diabetes. In this study, we aim to elucidate the association between GDM pathogenesis and distribution of gut microflora by quantifying the diversity of gut microflora in women with GDM.
Methods
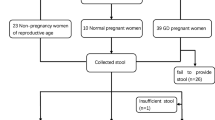
For the experimental and control groups, 19 patients with GDM during 24–28 weeks gestation and 19 healthy pregnant women were selected, respectively. High-throughput sequencing and bioinformatics analysis were used to characterize the V4 region of the 16S rRNA gene from various intestinal bacteria obtained via the subjects’ stool.
Results
The richness and diversity of the pregnant women’s intestinal floras were similar between the experimental and control groups. However, the structural specificities of the intestinal floras between the two groups were significantly different, with the distributions of the thick-walled and actinomycetes phyla being generally lower in the experimental group compared with the control group (x2 = 729.902, p < 0.001; x2 = 26.880, p < 0.001), whereas the distribution of the anaphyla phylum was higher in the experimental group (x2 = 428.233, p < 0.001; x2 = 545.707, p < 0.001) The abundance of genera of Bacillus, A. tumefaciens, Bifidobacterium, and Lactobacillus in the experimental samples was much lower than that in the control samples, whereas the abundance of Prevotella, Escherichia, and Clostridium was higher than in the control samples (x2 = 250,741.608, p < 0.001; x2 = 576.128, p < 0.001; x2 = 6.945, p = 0.080).
Conclusion
In this study, the abundance and diversity of the intestinal floras were similar in both women with GDM and healthy pregnant women. Conversely, the specificities of the intestinal floras were significantly different between the two groups, with a relative decrease in the abundance of Actinobacteria and thick-walled phyla and a relative increase in the abundance of Aspergillus and Bacteroides phyla.






Similar content being viewed by others
References
Zhang Y, Han Y, Dong Q. The effect of individualized exercise prescriptions combined with dietary management on blood glucose in the second-and-third trimester of gestational diabetes mellitus. Am J Transl Res. 2021;13(6):7388–93.
Ye Y, Xiong Y, Zhou Q, Wu J, Li X, Xiao X. Comparison of machine learning methods and conventional logistic regressions for predicting gestational diabetes using routine clinical data: a retrospective cohort study. J Diabetes Res. 2020;2020:4168340. https://doi.org/10.1155/2020/4168340.
Teng F, Wu J, Wei M, Yang Y. Expression of intercellular adhesion molecule-1 in umbilical vascular of pregnant women with gestational diabetes mellitus and the clinical significance. Exp Ther Med. 2018;15(1):914–8. https://doi.org/10.3892/etm.2017.5475.
Zhang X, Zhao X, Huo L, Yuan N, Sun J, Du J, Ji L. Risk prediction model of gestational diabetes mellitus based on nomogram in a Chinese population cohort study. Sci Rep. 2020;10(1):21223. https://doi.org/10.1038/s41598-020-78164-x.
Kang S, Kim MH, Kim MY, Hong JS, Kwak SH, Choi SH, Jang HC. Progression to gestational diabetes mellitus in pregnant women with one abnormal value in repeated oral glucose tolerance tests. Diabetes Metab J. 2019;43(5):607–14. https://doi.org/10.4093/dmj.2018.0159.
Zhou X, Xiang C, Zheng X. miR-132 serves as a diagnostic biomarker in gestational diabetes mellitus and its regulatory effect on trophoblast cell viability. Diagn Pathol. 2019;14(1):119. https://doi.org/10.1186/s13000-019-0899-9.
Li S, Wang Z, Yang Y, Yang S, Yao C, Liu K, Guo G. Lachnospiraceae shift in the microbial community of mice faecal sample effects on water immersion restraint stress. AMB Express. 2017;7(1):82. https://doi.org/10.1186/s13568-017-0383-4.
Cai J, Zhou L, Song X, Yin M. Huang F (2020) Alteration of intestinal microbiota in 3-deoxyglucosone-induced prediabetic rats[J]. Biomed Res Int. 2020;2020(6):1–11. https://doi.org/10.1155/2020/8406846.
Chen T, Zhang Y, Zhang Y, Shan C, Zhang Y, Fang K, Shi Z. Relationships between gut microbiota, plasma glucose and gestational diabetes mellitus. Journal of diabetes investigation. 2021;12(4):641–50. https://doi.org/10.1111/jdi.13373.
Meng X, Liu X, Tan J, Sheng Q, Zhang D, Li B, Zhang S. From Xiaoke to diabetes mellitus: a review of the research progress in traditional Chinese medicine for diabetes mellitus treatment. Chinese medicine. 2023;18(1):75. https://doi.org/10.1186/s13020-023-00783-z.
Wang J, Zheng J, Shi W, Du N, Xu X, Zhang Y, Zhao F. Dysbiosis of maternal and neonatal microbiota associated with gestational diabetes mellitus. Gut. 2018;67(9):1614–25. https://doi.org/10.1136/gutjnl-2018-315988.
Ferrocino I, Ponzo V, Gambino R, Zarovska A, Leone F, Monzeglio C, Bo S. Changes in the gut microbiota composition during pregnancy in patients with gestational diabetes mellitus. Sci Rep. 2018;8(1):12216. https://doi.org/10.1038/s41598-018-30735-9.
Li L, Qu M, Liu C, Xu L, Pan K, Song X, ..., Zhao X (2018) Lentinula edodes expression of a recombinant xylanase by and its effects on ruminal fermentation and microbial community in incubation of agricultural straws. Frontiers in microbiology 9:2944. doi:https://doi.org/10.3389/fmicb.2018.02944.
Lee KH, Guo J, Song Y, Ariff A, O'Sullivan M, Hales B, ..., Zhang G (2021) Dysfunctional gut microbiome networks in childhood IgE-mediated food allergy. Int J Mol Sci 22(4). doi:https://doi.org/10.3390/ijms22042079.
Cai XT, Lei MY, Huai-Tong XU (2018) Study on plasma D-dimer levels in pregnant women with gestational diabetes during the middle and late stages of pregnancy and early puerperium. China Practical Medicine.
Oli JM, Adeyemo AA, Okafor GO, Ofoegbu EN, Onyenekwe B, Chukwuka CJ, Rotimi CN. Basal insulin resistance and secretion in Nigerians with type 2 diabetes mellitus. Metab Syndr Relat Disord. 2009;7(6):595–9.
Foufelle F, Ferré P. Mechanism of storage and synthesis of fatty acids and triglycerides in white adipocytes. In: Bastard J-P, Fève B, editors. Physiology and physiopathology of adipose tissue. Springer Paris; 2013. p. 101–21. https://doi.org/10.1007/978-2-8178-0343-2_8.
Duchmann R, May E, Heike M, Knolle P, Neurath M, Zum Buschenfelde KHM. T cell specificity and cross reactivity towards enterobacteria, Bacteroides, Bifidobacterium, and antigens from resident intestinal flora in humans. Gut. 1999;44(6):812–8. https://doi.org/10.1136/gut.44.6.812.
Berger ER, Iyengar NM. Obesity and energy balance considerations in triple-negative breast cancer. Cancer J. 2021;27. https://doi.org/10.1097/PPO.0000000000000502.
Al-Khayat T, Sc M. Glucose tolerance in pregnant women inflicted with Candida albicans.
HäRtel C, Pagel J, Rupp J, Bendiks M, Guthmann F, Rieger-Fackeldey E, Zimmermann B. Prophylactic use of Lactobacillus acidophilus/Bifidobacterium infantis probiotics and outcome in very low birth weight infants. J Pediatr. 2014;165(2):285–289.e281. https://doi.org/10.1016/j.jpeds.2014.04.029.
Tang JN, Zeng ZG, Wang HN, Yang T, Zou LK. An effective method for isolation of DNA from pig faeces and comparison of five different methods. J Microbiol Methods. 2008;75(3):432–6. https://doi.org/10.1016/j.mimet.2008.07.014.
Limdi JK, O’Neill C, Mclaughlin J. Do probiotics have a therapeutic role in gastroenterology? 2006;12(034):5447–57.
Chu X, Yan P, Zhang N, Feng L, Li X, Wang Y, Yang K. Probiotics for preventing gestational diabetes mellitus in overweight or obese pregnant women: a systematic review and meta-analysis. Clinical nutrition ESPEN. 2022;50:84–92. https://doi.org/10.1016/j.clnesp.2022.05.007.
Li G, Feng H, Mao X, Deng Y, Wang X, Zhang Q, Xiao S. The effects of probiotics supplementation on glycaemic control among adults with type 2 diabetes mellitus: a systematic review and meta-analysis of randomised clinical trials. J Transl Med. 2023;21(1):442. https://doi.org/10.1186/s12967-023-04306-0.
Yun HO, Choi S, Lee G, Son JS, Sang MP. Changes in body composition are associated with metabolic changes and the risk of metabolic syndrome. J Clin Med. 2021;10(4):745.
Rong B, Wu Q, Reiter RJ, Sun C. The mechanism of oral melatonin ameliorates intestinal and adipose lipid dysmetabolism through reducing Escherichia coli-derived lipopolysaccharide - ScienceDirect. Cell Mol Gastroenterol Hepatol. 2021;12(5):1643–67.
Acknowledgments
We thank the clinicians in this group for their perseverance and dedication, and the editors for their comments on this article.
Funding
This research is supported by the Heilongjiang Provincial Health and Wellness Commission Research Project (No.2020–235).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Institutional Review Board (IRB) of Heilongjiang Provincial Hospital (096JY02).
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, X., Bian, B., Du, F. et al. Analysis of the gut microflora in women with gestational diabetes mellitus. Int J Diabetes Dev Ctries (2023). https://doi.org/10.1007/s13410-023-01262-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13410-023-01262-9