Abstract
Objective
Diabetes is a non-communicable disease, and the prevalence of diabetes is higher in low and middle-income countries. In India, diabetes prevalence has been observed, with some regional variations across the states. This study analyses the current scenario of diabetes in India among women of the reproductive age group between 15 to 49 years.
Methods
For conducting this study, data were gathered from the fifth round of the National Family Health Survey (2019–2021). It is a two-stage cross-sectional stratified sampling survey that employs the probability proportional to size methodology. A total of 6,59,010 individual reproductive-age women have been sampled for this study. Data were analyzed using the Stata version 14 software. A binary logistic model was carried out to know the relationships between diabetes and various socioeconomic and demographic variables. In addition, the adjusted odds ratio was reported with a 95% confidence interval.
Results
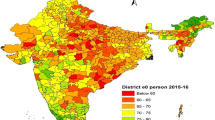
The result shows that about 1.65% of reproductive age group women in India are diabetic with the highest in Goa (4.09%) and the lowest in Nagaland (0.81%). Further, in urban areas, the women's diabetes rate is 16% higher than in the rural areas. Besides, diabetes is strongly correlated with obese reproductive age-group women who are above 35 years and reside in urban areas with higher socioeconomic status.
Conclusion
This study suggests that there is an urgent need for frequent monitoring of glycated haemoglobin (HbA1c). Besides, a spatially-optimized target-oriented policy framework is needed instead of a comprehensive national policy to tackle diabetes problems in the country.


Similar content being viewed by others
Data availability
This study is based on the secondary data source that is available in the public domain through the Demographic and Health Survey (DHS) website (https://dhsprogram.com/data/available-datasets.cfm). The relevant authorities have obtained the necessary ethical approval for this survey. As a result, no additional ethical approval is required for this study.
References
Lin X, Xu Y, Pan X, Xu J, Ding Y, Sun X, et al. Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Sci Rep. 2020;10(1):1–11.
Shang X, Li J, Tao Q, Li J, Li X, Zhang L, et al. Educational level, obesity and incidence of diabetes among chinese adult m,en and women aged 18–59 years old: an 11-year follow-up study. PLoS ONE. 2013;8(6):1–8.
IDF. IDF Diabetes Atlas, 10th Edition Committee. Diabetes Res Clin Pract. 2021;102(2):1–135.
Bellou V, Belbasis L, Tzoulaki I, Evangelou E. Risk factors for type 2 diabetes mellitus: An exposure-wide umbrella review of meta-analyses. PLoS ONE. 2018;13(3):1–27.
World Health Organization. Diabetes [Internet]. 2021 [cited 2022 May 29]. Available from: https://www.who.int/news-room/fact-sheets/detail/diabetes. Accessed 20 May 2022.
Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J. Epidemiology of type 2 diabetes - Global burden of disease and forecasted trends. J Epidemiol Glob Health. 2020;10(1):107–11.
Misra A, Gopalan H, Jayawardena R, Hills AP, Soares M, Reza-Albarrán AA, et al. Diabetes in developing countries. J Diabetes. 2019;11(7):522–39.
Maiti S, Akhtar S, Upadhyay AK, Mohanty SK. Socioeconomic inequality in awareness, treatment and control of diabetes among adults in India: Evidence from National Family Health Survey of India (NFHS), 2019–2021. Sci Rep. 2023;13(1):1–12.
Tandon N, Anjana RM, Mohan V, Kaur T, Afshin A, Ong K, et al. The increasing burden of diabetes and variations among the states of India: the Global Burden of Disease Study 1990–2016. Lancet Glob Health. 2018;6(12):e1352–62.
Corsi DJ, Subramanian SV. Association between socioeconomic status and self-reported diabetes in India: A cross-sectional multilevel analysis. BMJ Open. 2012;2(4):1–12.
Ramachandran A, Snehalatha C, Shetty AS, Nanditha A. Trends in prevalence of diabetes in Asian countries. World J Diabetes. 2012;3(6):110–7.
Bharati DR, Pal R, Kar S, Rekha R, Yamuna TV, Basu M. Prevalence and determinants of diabetes mellitus in Puducherry, South India. J Pharm Bioallied Sci. 2011;3(4):513–8.
Nordström A, Hadrévi J, Olsson T, Franks PW, Nordström P. Higher Prevalence of Type 2 Diabetes in Men Than in Women Is Associated With Differences in Visceral Fat Mass. J Clin Endocrinol Metab. 2016;101(10):3740–6.
Corsi DJ, Subramanian SV. Association between socioeconomic status and self-reported diabetes in India: A cross-sectional multilevel analysis. BMJ Open. 2012;2(4):12–23.
Pradeepa R, Anjana RM, Joshi SR, Bhansali A, Deepa M, Joshi PP, et al. Prevalence of generalized & abdominal obesity in urban & rural India- the ICMR-INDIAB study (Phase-I) [ICMR-INDIAB-3]. Indian J Med Res. 2015;142(AUGUST):139–50.
Kaveeshwar SA, Cornwall J. The current state of diabetes mellitus in India. Australas Med J. 2014;7(1):45–8.
Aziz N, Kallur SD, Nirmalan PK. Implications of the Revised Consensus Body Mass Indices for Asian Indians on Clinical Obstetric Practice. J Clin Diagn Res JCDR. 2014;8(5):OC01-3.
Mahajan K, Batra A. Obesity in adult asian indians- the ideal BMI cut-off. Indian Heart J. 2018;70(1):195.
Chaudhary M, Sharma P. Abdominal obesity in India: analysis of the National Family Health Survey-5 (2019–2021) data. Lancet Reg Health - Southeast Asia. 2023;14:1-10. Available from: https://www.thelancet.com/journals/lansea/article/PIIS2772-3682(23)00068-9/fulltext#secsectitle0010.
Misra A, Vikram NK, Gupta R, Pandey RM, Wasir JS, Gupta VP. Waist circumference cutoff points and action levels for Asian Indians for identification of abdominal obesity. Int J Obes. 2006;30(1):106–11.
Claypool KT, Chung MK, Deonarine A, Gregg EW, Patel CJ. Characteristics of undiagnosed diabetes in men and women under the age of 50 years in the Indian subcontinent: the National Family Health Survey (NFHS-4)/Demographic Health Survey 2015–2016. BMJ Open Diabetes Res Care. 2020;8(1):1–10.
Dandona L, Dandona R, Kumar GA, Shukla DK, Paul VK, Balakrishnan K, et al. Nations within a nation: variations in epidemiological transition across the states of India, 1990–2016 in the Global Burden of Disease Study. The Lancet. 2017;390(10111):2437–60.
Singh S, Puri P, Subramanian SV. Identifying spatial variation in the burden of diabetes among women across 640 districts in India: a cross-sectional study. J Diabetes Metab Disord. 2020;19(1):523–33.
Agyemang-Yeboah F, Eghan BAJ, Annani-Akollor ME, Togbe E, Donkor S, Oppong AB. Evaluation of Metabolic Syndrome and Its Associated Risk Factors in Type 2 Diabetes: A Descriptive Cross-Sectional Study at the Komfo Anokye Teaching Hospital, Kumasi, Ghana. BioMed Res Int. 2019;2(2019):1–8.
Ghassab-Abdollahi N, Nadrian H, Pishbin K, Shirzadi S, Sarbakhsh P, Saadati F, et al. Gender and urban–rural residency based differences in the prevalence of type-2 diabetes mellitus and its determinants among adults in Naghadeh: Results of IraPEN survey. PLoS ONE. 2023;18(3):1–16.
Anjana RM, Deepa M, Pradeepa R, Mahanta J, Narain K, Das HK, et al. Prevalence of diabetes and prediabetes in 15 states of India: results from the ICMR–INDIAB population-based cross-sectional study. Lancet Diabetes Endocrinol. 2017;5(8):585–96.
Geldsetzer P, Manne-Goehler J, Theilmann M, Davies JI, Awasthi A, Vollmer S, et al. Diabetes and hypertension in India a nationally representative study of 1.3 million adults. JAMA Intern Med. 2018;178(3):363–72.
Kautzky-Willer A, Dorner T, Jensby A, Rieder A. Women show a closer association between educational level and hypertension or diabetes mellitus than males: A secondary analysis from the Austrian HIS. BMC Public Health. 2012;12(1):1–9.
Anjana RM, Pradeepa R, Deepa M, Datta M, Sudha V, Unnikrishnan R, et al. Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: Phase I results of the Indian Council of Medical Research–INdia DIABetes (ICMR–INDIAB) study. Diabetologia. 2011;54(12):3022–7.
Rosiek A, Maciejewska NF, Leksowski K, Rosiek-Kryszewska A, Leksowski Ł. Effect of television on obesity and excess of weight and consequences of health. Int J Environ Res Public Health. 2015;12(8):9408–26.
Tandon A, Bordoloi B, Jaiswal R, Srivastava A, Singh R, Shafique U. Demographic and clinicopathological profile of oral squamous cell carcinoma patients of North India: A retrospective institutional study. SRM J Res Dent Sci. 2018;9(3):114–18.
Atre S. The burden of diabetes in India. Lancet Glob Health. 2019;7(4): e418.
Vennu V, Abdulrahman TA, Bindawas SM. The prevalence of overweight, obesity, hypertension, and diabetes in India: Analysis of the 2015–2016 national family health survey. Int J Environ Res Public Health. 2019;16(20):2–22.
Geldsetzer P, Manne-Goehler J, Theilmann M, Davies JI, Awasthi A, Vollmer S, et al. Diabetes and hypertension in India a nationally representative study of 1.3 million adults. JAMA Intern Med. 2018;178(3):363–72.
Daivadanam M, Absetz P, Sathish T, Thankappan KR, Fisher EB, Philip NE, et al. Lifestyle change in Kerala, India: Needs assessment and planning for a community-based diabetes prevention trial. BMC Public Health. 2013;13(1):1–16.
Sarma PS, Sadanandan R, Thulaseedharan JV, Soman B, Srinivasan K, Varma RP, et al. Prevalence of risk factors of non-communicable diseases in Kerala, India: results of a cross-sectional study. BMJ Open. 2019;9(11):1–10.
Mahajan A, Sharma S, Dhar MK, Bamezai RNK. Risk factors of type 2 diabetes in population of Jammu and Kashmir, India. J Biomed Res. 2013;27(5):372–79.
Lin BY, Genden K, Shen W, Wu PS, Yang WC, Hung HF, et al. The prevalence of obesity and metabolic syndrome in Tibetan immigrants living in high altitude areas in Ladakh, India. Obes Res Clin Pract. 2018;12(4):365–71.
Chanda S, Dogra V, Hazarika N, Bambrah H, Sudke AK, Vig A, et al. Original research: Prevalence and predictors of gestational diabetes mellitus in rural Assam: a cross-sectional study using mobile medical units. BMJ Open. 2020;10(11):1–7.
Patel NR, Kennedy A, Blickem C, Rogers A, Reeves D, Chew-Graham C. Having diabetes and having to fast: A qualitative study of British Muslims with diabetes. Health Expect. 2015;18(5):1698–708.
Hassanein M, Al-Arouj M, Hamdy O, Bebakar WMW, Jabbar A, Al-Madani A, et al. Diabetes and Ramadan: Practical guidelines. Diabetes Res Clin Pract. 2017;1(126):303–16.
Marbaniang SP, Chungkham HS, Lhungdim H. A structured additive modeling of diabetes and hypertension in Northeast India. PLoS ONE. 2022;17(1):1–20.
Kposowa AJ, Ezzat DA, Breault K. Diabetes mellitus and marital status: Evidence from the national longitudinal mortality study on the effect of marital dissolution and the death of a spouse. Int J Gen Med. 2021;14:1881–8.
Gunderson EP. Childbearing and Obesity in Women: Weight Before, During, and After Pregnancy. Obstet Gynecol Clin North Am. 2009;36(2):317–32.
Wang T, Zhao Z, Wang G, Li Q, Xu Y, Li M, et al. Age-related disparities in diabetes risk attributable to modifiable risk factor profiles in Chinese adults: a nationwide, population-based, cohort study. Lancet Healthy Longev. 2021;2(10):e618–28.
American Diabetes Association Professional Practice Committee. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2022. Diabetes Care. 2021;45(Supplement_1):S17–38.
Acknowledgment
The authors are thankful to the Demographic and Health Survey (DHS) website for permitting us to download the dataset and International Institute for Population Sciences (IIPS) for creating data available for the study.
Author information
Authors and Affiliations
Contributions
CR, SB, and VPS contributed to the conceptualization and study design. CR and SB performed the statistical analysis. CR, and SB interpreted the results and discussed the findings. CR, SB, VPS, AB, and SK drafted and finalized the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
The necessary ethical approval has been taken by the respective authorities for this cross-sectional survey (NFHS-5). Hence, there is no need to take additional ethical approval for this study.
Financial support and sponsorship
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
We don’t have any conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Roy, C., Biswas, S., Sati, V.P. et al. Bio-demographical determinants of diabetes among women in reproductive age group (15–49) in India: Evidence from National Family Health Survey (NFHS) of India, 2019–2021. Int J Diabetes Dev Ctries (2023). https://doi.org/10.1007/s13410-023-01237-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13410-023-01237-w