Abstract
Background
To date, studies on the effects of preeclampsia on perinatal outcomes in women with gestational diabetes mellitus (GDM) are comparatively few, and the results are inconsistent.
Objective
This study aimed to explore the effects of preeclampsia on perinatal outcomes in women with GDM.
Methods
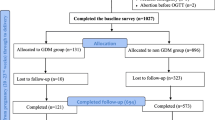
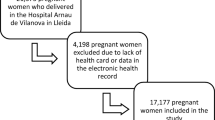
This retrospective cohort study collected data of women with GDM whose babies were delivered in a Chinese hospital between July 2017 and June 2020. We divided eligible pregnant women with GDM into two groups based on whether they were diagnosed with preeclampsia: GDM with preeclampsia group and GDM without preeclampsia group. Logistic regression analysis was performed to evaluate the risks for perinatal outcomes which were used as the dependent variables.
Results
We identified 7533 eligible women with GDM (245 in GDM with preeclampsia group and 7288 in GDM without preeclampsia group). After adjusting for covariates, preeclampsia was significantly associated with higher risks of fetal malformations (OR: 1.67, 95% CI: 1.08–2.57), fetal growth restriction (OR: 5.36, 95% CI: 2.91–9.88), cesarean section (OR: 2.48, 95% CI: 1.83–3.37), emergency cesarean section (OR: 2.32, 95% CI: 1.77–3.05), preterm birth (OR: 1.89, 95% CI: 1.27–2.81), low birth weight (LBW) (OR: 3.30, 95% CI: 2.16–5.05), small for gestational age (SGA) (OR: 3.05, 95% CI: 2.01–4.63) and neonatal hypoglycemia (OR: 1.77, 95% CI: 1.10–2.85).
Conclusion
Women with GDM complicated with preeclampsia were at higher risks of fetal malformations, fetal growth restriction, cesarean section, emergency cesarean section, preterm birth, LBW, SGA and neonatal hypoglycemia.
Similar content being viewed by others
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
International Diabetes Federation. IDF Diabetes Atlas 10th edition. https://diabetesatlas.org/atlas/tenth-edition/. Accessed 29 Mar 2022].
Abalos E, Cuesta C, Grosso AL, Chou D, Say L. Global and regional estimates of preeclampsia and eclampsia: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2013;170:1–7. https://doi.org/10.1016/j.ejogrb.2013.05.005.
Gao C, Sun X, Lu L, Liu F, Yuan J. Prevalence of gestational diabetes mellitus in mainland China: A systematic review and meta-analysis. J Diabetes Invest. 2019;10:154–62. https://doi.org/10.1111/jdi.12854.
Li F, Qin J, Zhang S, Chen L. Prevalence of hypertensive disorders in pregnancy in China: A systematic review and meta-analysis. Pregnancy hypertens. 2021;24:13–21. https://doi.org/10.1016/j.preghy.2021.02.001.
Plows J, Stanley J, Baker P, Reynolds C, Vickers M. The Pathophysiology of Gestational Diabetes Mellitus. Int J Mol Sci. 2018;19:3342. https://doi.org/10.3390/ijms19113342.
Billionnet C, Mitanchez D, Weill A, Nizard J, Alla F, Hartemann A, et al. Gestational diabetes and adverse perinatal outcomes from 716,152 births in France in 2012. Diabetologia. 2017;60:636–44. https://doi.org/10.1007/s00125-017-4206-6.
Shen M, Smith GN, Rodger M, White RR, Walker MC, Wen SW, et al. Comparison of risk factors and outcomes of gestational hypertension and pre-eclampsia. Plos One. 2017;12:e175914. https://doi.org/10.1371/journal.pone.0175914.
Sibai B, Dekker G, Kupferminc M. Pre-eclampsia. Lancet. 2005;365:785–99. https://doi.org/10.1016/S0140-6736(05)17987-2.
Östlund I, Haglund B, Hanson U. Gestational diabetes and preeclampsia. Eur J Obstet Gyn R B. 2004;113:12–6. https://doi.org/10.1016/j.ejogrb.2003.07.001.
Sun Y, Yang H, Sun WJ. Risk factors for pre-eclampsia in pregnant Chinese women with abnormal glucose metabolism. Int J Gynaecol Obstet. 2008;101:74–6. https://doi.org/10.1016/j.ijgo.2007.10.008.
Schneider S, Freerksen N, Röhrig S, Hoeft B, Maul H. Gestational diabetes and preeclampsia – Similar risk factor profiles? Early Hum Dev. 2011;88:179–84. https://doi.org/10.1016/j.earlhumdev.2011.08.004.
Sibai BM, Ross MG. Hypertension in gestational diabetes mellitus: Pathophysiology and long-term consequences. J Matern Fetal Neonatal Med. 2010;23:229–33. https://doi.org/10.3109/14767050903550899.
Chen ZY, Chen J. Risk factors and pregnancy outcomes analysis of gestational diabetes mellitus complicated with preeclampsia. Matern Child Health Care China. 2017;32:2616–8. https://doi.org/10.7620/zgfybj.j.issn.1001-4411.2017.12.38.
Shi W, Peng XX, Ma XH. Characteristics of gestational diabetes mellitus combined with pre-eclampsia and the effects on pregnancy outcomes. Chin J Med. 2018;53:1006–8. https://doi.org/10.3969/j.issn.1008-1070.2018.09.016.
Zhao J, Xu F. Analysis of pregnancy outcome of gestational diabetes mellitus complicated with preeclampsia. J Wenzhou Med Coll. 2012;42:63–5. https://doi.org/10.3969/j.issn.1000-2138.2012.01.018.
Nunes JS, Ladeiras R, Machado L, Coelho D, Duarte C, Furtado JM. The Influence of Preeclampsia, Advanced Maternal Age and Maternal Obesity in Neonatal Outcomes Among Women with Gestational Diabetes. Rev Bras Ginecol Obstet. 2020;42:607–13. https://doi.org/10.1055/s-0040-1710300.
Metzger BE, Gabbe SG, Persson B, Buchanan TA, Catalano PM, Damm P, et al. International Association of Diabetes and Pregnancy Study Groups Recommendations on the Diagnosis and Classification of Hyperglycemia in Pregnancy. Diabetes Care. 2010;33:676–82. https://doi.org/10.2337/dc09-1848.
Hypertension Disorders of Pregnancy Subgroup. Chinese Society of Obstetrics and Gynecology, Chinese Medical Association. Diagnosis and treatment guideline for hypertension disorders of pregnancy. Chin J Obstet Gynecol. 2015;50:721–8. https://doi.org/10.3760/cma.j.issn.0529-567x.2015.10.001.
Rasmussen K, Yaktine A. Weight Gain During Pregnancy: Reexamining the Guidelines. Washington DC: The National Academies Press (US); 2009.
Department of Obstetrics and Gynecology Chinese Medical Association. Guidelines for Prevention and Management of Postpartum Hemorrhage (2014). Chin J Obstet Gynecol. 2014;49:641–6. https://doi.org/10.3760/cma.j.issn.0529-567x.2014.09.001.
Fetal Medicine Subgroup, Society of perinatal Medicine, Chinese Medical Association, Obstetrics Subgroup, Society of Obstetrics and Gynecology, Chinese Medical Association. Expert consensus on fetal growth restriction. Chin J Perinat Med. 2019;22:361–80. https://doi.org/10.3760/cma.j.issn.1007-9408.2019.06.001.
Dai L, Deng C, Li Y, Zhu J, Mu Y, Deng Y, et al. Birth weight reference percentiles for Chinese. Plos One. 2014;9:e104779. https://doi.org/10.1371/journal.pone.0104779.
Balsells M, Garcia-Patterson A, Gich I, Corcoy R. Major congenital malformations in women with gestational diabetes mellitus: a systematic review and meta-analysis. Diabetes Metab Res Rev. 2012;28:252–7. https://doi.org/10.1002/dmrr.1304.
Lai FY, Johnson JA, Dover D, Kaul P. Outcomes of singleton and twin pregnancies complicated by pre-existing diabetes and gestational diabetes: A population-based study in Alberta, Canada, 2005–2011. J Diabetes. 2016;8:45–55. https://doi.org/10.1111/1753-0407.12255.
Nelson DB, Chalak LF, McIntire DD, Leveno KJ. Is preeclampsia associated with fetal malformation? A review and report of original research. J Matern Fetal Neonatal Med. 2015;28:2135–40. https://doi.org/10.3109/14767058.2014.980808.
Joo EH, Kim YR, Kim N, Jung JE, Han SH, Cho HY. Effect of Endogenic and Exogenic Oxidative Stress Triggers on Adverse Pregnancy Outcomes: Preeclampsia, Fetal Growth Restriction, Gestational Diabetes Mellitus and Preterm Birth. Int J Mol Sci. 2021;22:10122. https://doi.org/10.3390/ijms221810122.
Phaloprakarn C, Tangjitgamol S. Risk assessment for preeclampsia in women with gestational diabetes mellitus. J Perinat Med. 2009;37:617. https://doi.org/10.1515/JPM.2009.108.
Yogev Y, Xenakis EM, Langer O. The association between preeclampsia and the severity of gestational diabetes: the impact of glycemic control. Am J Obstet Gynecol. 2004;191(5):1655–60. https://doi.org/10.1016/j.ajog.2004.03.074.
Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med. 2005;352:2477–86. https://doi.org/10.1056/NEJMoa042973.
Hartling L, Dryden DM, Guthrie A, Muise M, Vandermeer B, Donovan L. Benefits and harms of treating gestational diabetes mellitus: a systematic review and meta-analysis for the US Preventive Services Task Force and the National Institutes of Health Office of Medical Applications of Research. Ann Intern Med. 2013;159:123–9. https://doi.org/10.7326/0003-4819-159-2-201307160-00661.
Funding
This work was supported by the National Natural Science Foundation of China (Grant No. 81903334).
Author information
Authors and Affiliations
Contributions
Ruixue Tian designed the study, collected and analyzed the data, and drafted the manuscript. Jingqi Xu collected the data, cleaned the data and contributed to the interpretation of the data. Jing He designed the study and managed the data. Zhen Chen contributed to the interpretation of the data and reviewed the manuscript. Yanqun Liu designed the study and managed the data. Xiaoli Chen and Zhijie Zou designed the study and revised the manuscript. All authors gave their final approval for this version of the manuscript to be published.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was approved by the ethics committee of Chongqing Health Center for Women and Children (No. 2020–022) and performed in accordance with the Declaration of Helsinki.
Informed consent
Written informed consent for participation was not required because of the retrospective, anonymous nature of the study..
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tian, R., Xu, J., He, J. et al. Effects of preeclampsia on perinatal outcomes in women with gestational diabetes mellitus: A retrospective cohort study. Int J Diabetes Dev Ctries (2023). https://doi.org/10.1007/s13410-023-01236-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13410-023-01236-x