Abstract
Objective
To retrospectively analyze the mediating effects of body composition during the first trimester on the occurrence of gestational diabetes mellitus (GDM) in early third trimester in advanced maternal age (AMA).
Methods
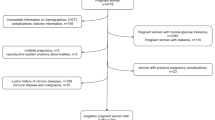
From December 2017 to May 2018, 1635 singleton pregnant women who underwent delivery in the Guiyang Maternal and Child Health Hospital were selected. The body composition data was measured by using the INBODY770 body composition instrument in the first trimester (mainly at a gestational age of 10–12 weeks). The blood glucose levels at fasting for one night and the cutoff values for them at 1 and 2 h after administration during the 75 g oral glucose tolerance test at gestational age of 24–28 weeks (the early stage of the 3rd trimester) were also collected. According to the Baron and Kenny’s criteria (the basic principle of interpreting the intermediary role), multivariate logistic regression was used to analyze the mediating effects of body composition (body fat percentage and protein percentage) between AMA and GDM occurrence.
Results
In total, 1635 subjects aged 30.93 ± 4.80 years were selected, and there were 376 women with AMA (23%). There were 983 pregnant women (39.88%) with a body fat percentage greater than 30% and 1331 (81.71%) pregnant women with a protein percentage less than 15%. The results showed significant differences in height, weight, lean body weight, body fat, body fat percentage, and GDM prevalence between AMA and low-age groups (p < 0.05). After adjusting height, parity, and AMA, the body fat percentage showed association with GDM (odds ratio, OR 1.85 (1.38 ~ 2.48); confidence interval, CI 95%, p < 0.05). After adjusting height, parity, and body weight percentage, the AMA showed association with GDM (OR (CI95%) 2.38 (1.68 ~ 3.37)). Similarly, the protein percentage showed association with GDM (OR (CI 95%) 0.50 (0.31 ~ 0.81), p < 0.05).
Conclusion
These results confirmed the mediating effects of body fat percentage and protein percentage on AMA and the occurrence of GDM. Advanced age is directly associated with increased risk of GDM, which in turn increases with higher percentage of body fat and lower percentage of protein.

Similar content being viewed by others
References
Chen Q, Carbone ET. Functionality, implementation, impact, and the role of health literacy in mobile phone apps for gestational diabetes: scoping review. JMIR Diabetes. 2017;2(2):e25.
Kapur A, Seshiah V. Women & diabetes: our right to a healthy future. Indian J Med Res. 2017;146(5):553–6.
Laopaiboon M, Lumbiganon P, Intarut N, Mori R, Ganchimeg T, Vogel JP, et al. Advanced maternal age and pregnancy outcomes: a multicountry assessment. BJOG. 2014;121(Suppl 1):49–56.
Kahveci B, Melekoqlu R, Evruke IC, Cetin C. The effect of advanced maternal age on perinatal outcomes in nulliparous singleton pregnancies. BMC Pregnancy Childbirth. 2018;18(1):343.
Yin O, Woods A, Koos B, DeVore G, Afshar Y. Central hemodynamics are associated with fetal outcomes in pregnancies of advanced maternal age. Pregnancy Hypertens. 2019;19:67–73.
Xue X, Kong BH, Duan T. Obstetrics and gynecology. 9th ed: People’s Health Publishing House; 2018. (In Chinese)
Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–82.
He Z, Xie H, Liang S, Tang Y, Ding W, Wu Y, et al. Influence of different diagnostic criteria on gestational diabetes mellitus incidence and medical expenditures in China. J Diabetes Investig. 2019;10(5):1347–57.
Waters TP, Dyer AR, Scholtens DM, Dooley SL, Herer E, Lowe LP, et al. Maternal and neonatal morbidity for women who would be added to the diagnosis of GDM using IADPSG criteria: a secondary analysis of the hyperglycemia and adverse pregnancy outcome study. Diabetes Care. 2016;39(12):2204–10.
Collier A, Abraham EC, Armstrong J, Godwin J, Monteath K, Lindsay R. Reported prevalence of gestational diabetes in Scotland: the relationship with obesity, age, socioeconomic status, smoking and macrosomia, and how many are we missing? J Diabetes Investig. 2017;8(2):161–7.
Hildén K, Hanson U, Persson M, Magnuson A, Simmons D, Fadl H. Gestational diabetes and adiposity are independent risk factors for perinatal outcomes: a population based cohort study in Sweden. Diabet Med. 2019;36(2):151–7.
Kouhkan A, Khamseh ME, Moini A, Pirjani R, Arabipoor A, Zolfaghari Z, et al. Diagnostic accuracy of body mass index and fasting glucose for the prediction of gestational diabetes mellitus after assisted reproductive technology. Int J Fertil Steril. 2019;13(1):32–7.
Najafi F, Hasani J, Izadi N, Hashemi-Nazari SS, Namvar Z, Mohammadi S, et al. The effect of prepregnancy body mass index on the risk of gestational diabetes mellitus: a systematic review and dose-response meta-analysis. Obes Rev. 2019;20(3):472–86.
Radzicka S, Pietryga M, Iciek R, Brązert J. The role of visfatin in pathogenesis of gestational diabetes (GDM). Ginekol Pol. 2018;89(9):518–21.
Segura MT, Demmelmair H, Krauss-Etschmann S, Nathan P, Dehmel S, Padilla MC, et al. Maternal BMI and gestational diabetes alter placental lipid transporters and fatty acid composition. Placenta. 2017;57:144–51.
Wang Y, Luo BR. The association of body composition with the risk of gestational diabetes mellitus in Chinese pregnant women: a case-control study. Medicine (Baltimore). 2019;98(42):e17576.
Andersson-Hall UK, Järvinen EAJ, Bosaeus MH, Gustavsson CE, Hårsmar EJ, Niklasson CA, et al. Maternal obesity and gestational diabetes mellitus affect body composition through infancy: the PONCH study. Pediatr Res. 2019;85(3):369–77.
Chavarrias M, Carlos-Vivas J, Barrantes-Martín B, Pérez-Gómez J. Effects of 8-week of fitness classes on blood pressure, body composition, and physical fitness. J Sports Med Phys Fitness. 2019c;59(12):2066–74.
Kuriyan R. Body composition techniques. Indian J Med Res. 2018;148(5):648–58.
Vrachnis N, Belitsos P, Sifakis S, Dafopoulos K, Siristatidis C, Pappa KI, et al. Role of adipokines and other inflammatory mediators in gestational diabetes mellitus and previous gestational diabetes mellitus. Int J Endocrinol. 2012;2012:549748.
Hashim M, Radwan H, Hasan H, Obaid RS, Al Ghazal H, Al Hilali M, et al. Gestational weight gain and gestational diabetes among Emirati and Arab women in the United Arab Emirates: results from the MISC cohort. BMC Pregnancy Childbirth. 2019;19(1):463.
Carolan M, Davey MA, Biro MA, Kealy M. Maternal age, ethnicity and gestational diabetes mellitus. Midwifery. 2012;28(6):778–83.
Meek CL, Devoy B, Simmons D, Patient CJ, Aiken AR, Murphy HR. Seasonal variations in incidence and maternal-fetal outcomes of gestational diabetes. Diabet Med. 2020;37(4):674–80.
Erem C, Kuzu UB, Deger O, Can G. Prevalence of gestational diabetes mellitus and associated risk factors in Turkish women: the Trabzon GDM study. Arch Med Sci. 2015;11(4):724–35.
Laine MK, Kautiainen H, Gissler M, Raina M, Aahos I, Järvinen K, et al. Gestational diabetes in primiparous women-impact of age and adiposity: a register-based cohort study. Acta Obstet Gynecol Scand. 2018;97(2):187–94.
Aydın H, Çelik Ö, Yazıcı D, Altunok Ç, Tarçın Ö, Deyneli O, et al. Prevalence and predictors of gestational diabetes mellitus: a nationwide multicentre prospective study. Diabet Med. 2019;36(2):221–7.
Heslehurst N, Ells LJ, Simpson H, Batterham A, Wilkinson J, Summerbell CD. Trends in maternal obesity incidence rates, demographic predictors, and health inequalities in 36 821 women over a 15-year period. BJOG. 2007;114(2):187–94.
Acknowledgments
We thank Guizhou University of Chinese Traditional Medicine and Guiyang Maternal and Child Health Hospital for their help and support. We also thank the women who participated in this study for their contribution and time.
Funding
This work was financed by grants from the Natural Science Foundation of China (81760336) and Guizhou Health Commission (Gzwjkj2018-1-079).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was approved by the ethics committee of Guiyang Maternal and Child Health Hospital.
Consent to participate
Informed consent was obtained from women who participated.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jing, L., Dan, Z., Huiqun, W. et al. Mediating effects of body composition at the first trimester on the occurrence of GDM at the early stage of the third trimester during the advanced maternal age. Int J Diabetes Dev Ctries 41, 121–126 (2021). https://doi.org/10.1007/s13410-020-00845-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-020-00845-0