Abstract
Background
At present, stroke is a major health burden and the leading cause of death and long-term disability in the elderly. Ischemic stroke is the most common stroke type in the Thai population. Causes of ischemic stroke are likely to be multifactorial.
Objective
The purpose of this study was to determine the association between hemoglobin A1c (HbA1c) and acute ischemic stroke (AIS) among Thai patients with type-2 diabetes (PTDs).
Methods
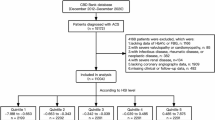
A hospital-based case-control study was conducted among PTDs attending the Bhuddasothorn hospital with 100 cases and 300 controls from 2013 to 2016. Cases were defined as PTDs who had an AIS and diagnosed by neurologists and computed tomography (CT) scan and controls were PTDs who did not have AIS. Cases and controls were matched by gender, age (± 5 years), residential area, and attending duration. Data were collected using a questionnaire comprising 2 parts: demographic characteristics and medical data.
Results
Conditional logistic regression was applied to estimate the effect of HbA1c on acute ischemic stroke among PTDs. Univariable conditional logistic regression showed risk factors for AIS among the PTDs comprised history of dyslipidemia, history of atrial fibrillation, diastolic blood pressure, systolic blood pressure, HbA1c, history of CVD, FPG, creatinine, and microvascular complications (p < 0.05). For multivariable conditional logistic regression, after controlling for potential confounders, it revealed a HbA1c of 8–8.9% and higher increased the risk of AIS by a factor of 7.9 and 10.9 times, respectively (OR = 7.9, 95%CI = 3.0–20.9; OR = 10.9, 95%CI = 4.3–27.9).
Conclusions
Ongoing surveillance of HbA1c among PTDs should be conducted alongside knowledge sharing of glycemic control and stroke prevention as an essential measure to prevent developing AIS risk.

Similar content being viewed by others
References
Strong K, Mathers CD, Bonita R. Preventing stroke: saving lives around the world. Lancet Neurol. 2007;6:182–7.
Johnston SC, Mendis S, Mathers CD. Global variation in stroke burden and mortality: estimates from monitoring, surveillance, and modelling. Lancet Neurol. 2009;8:345–54.
Mackay J, Mensah GA. The atlas of heart disease and stroke. Geneva: World Health Organization; 2004.
Feigin VL, Krishnamurthi R. Epidemiology and risk factors: global burden of stroke. In: Grotta JC, Albers GW, Broderick JP, et al., editors. Stroke: pathophysiology, diagnosis and management. 6th ed. Beijing: Elsevier; 2016. p. 165–206.
Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, et al. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet. 2014;383(9913):245–54.
Murray CJ, Ezzati M, Flaxman AD, Lim S, Lozano R, Michaud C, et al. GBD 2010: design, definitions, and metrics. Lancet. 2012;380(9859):2063–6.
Bennett DA. Methodology of the global and regional burden of stroke study. Neuroepidemiology. 2012;38(1):30–40.
Bureau of policy and strategies, Ministry of Public Health. Thailand Health Profile 2011–2015. Bangkok: The War Veterans Organization of Thailand; 2016.
Bureau of policy and strategies, Ministry of Public Health. Public Health Statistics 2010. Bangkok: The War Veterans Organization of Thailand; 2010.
Bureau of policy and strategies, Ministry of Public Health. Public Health Statistics 2015. Bangkok: The War Veterans Organization of Thailand; 2016.
Suwanwela NC. Stroke epidemiology in Thailand. J Stroke. 2014;16:1–7.
Nilanont Y, Nidhinandana S, Suwanwela NC, Hanchaiphiboolkul S, Pimpak T, Tatsanavivat P, et al. Quality of acute ischemic stroke care in Thailand: a prospective multicenter countrywide cohort study. J Stroke Cerebrovasc Dis. 2014;23:213–9.
Hanchaiphiboolkul S, Puthkhao P, Towanabut S, Tantirittisak T, Wangphonphatthanasiri K, Termglicnchan T, et al. Factors predicting high estimated 10-year stroke risk: Thai Epidemiology Stroke Study. J Stroke Cerebrovasc Dis. 2014;23:1969–74.
Dhamasaroja P. Baseline characterisitics of patients with acute ischemic stroke in suburban area of Thailand. J Stroke Cerebrovasc Dis. 2008;17:82–5.
Ay H. Classification of ischemic stroke. In: Grotta JC, Albers GW, Broderick JP, Kasner SE, Lo EH, Mendelow AD, Sacco RL, Wong LKS, editors. Stroke: pathology, diagnosis, and management. 6th ed. Beijing: Elsevier; 2016. p. 295–307.
Amarenco P, Bogousslavsky J, Caplan LR, Donnan GA, Hennerici MG. Classification of stroke subtypes. Cerebrovasc Dis. 2009;27:493–501.
World Health Organization. Use of glycated haemoglobin (HbA1c) in the diagnosis of diabetes mellitus: abbreviated report of a WHO Consultation. WHO/NMH/CHP/CPM/11.1. Geneva: WHO; 2001.
Dupont WD. Power calculations for matched case-control studies. Biometrics. 1988;44:1157–68.
Sacco RL, Shi T, Zamanillo MC, Kargman DE. Predictors of mortality and recurrence after hospitalized cerebral infarction in an urban community: the Northern Manhattan Stroke Study. Neurology. 1994;44:626–34.
Najarian RM, Sulivan LM, Kannel WB, Wilson PW, D’Aqostino RB, Wolf PA. Metabolic syndrome compared with type 2 diabetes mellitus as a risk factor for stroke: the Framingham Offspring Study. Arch Intern Med. 2006;166:106–11.
Air EL, Kissela BM. Diabetes, the metabolic syndrome, and ischemic stroke; epidemiology and possible mechanisms. Diabetes Care. 2007;30:3131–40.
Banerjee C, Moon YP, Paik MC, Rundek T, Mora McLaughlin C, Vieira JR, et al. Duration of diabetes and risk of ischemic stroke: the Northern Manhattan Study. Stroke. 2012;43:1212–7.
Turner RC, Cull CA, Frighi V, Holman RR. Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies (UKPDS 49). UK Prospective Diabetes Study (UKPDS) Group. JAMA. 1999;281:2005–12.
Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009;360:129–39.
Holman RR, Paul SK, Bethel MA, Neil HA, Matthews DR. Long-term follow-up after tight control of blood pressure in type 2 diabetes. N Engl J Med. 2008;359:1565–76.
UK Prospective Diabetes Study Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352:837–53.
Gerstein HC, Miller ME, Byington RP, Goff DC Jr, Bigger JT, Buse JB, et al. Action to control cardiovascular risk in diabetes study group. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358:2545–59.
Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M, et al. Advance Collaborative Group. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358:2560–72.
Martin A, Rojas S, Chamorro A, Falcón C, Bargalló N, Planas AM. Why does acute hyperglycemia worsen the outcome of transient focal cerebral ischemia? Role of corticosteroids, inflammation, and protein O-glycosylation. Stroke. 2006;37:1288–95.
Bazzano LA, Green T, Harrison TN, Reynolds K. Dietary approaches to prevent hypertension. Curr Hypertens Rep. 2013;15:694–702.
Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. DASH-Sodium Collaborative Research Group. Effects on blood pressure reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-sodium collaborative research group. N Engl J Med. 2001;344:3–10.
O’Donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, Rao-Melacini P, et al. Rick factors for ischemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet. 2010;376:112–23.
Wijdicks EF, Sheth KN, Carter BS, Greer DM, Kasner SE, Kimberly WT, et al. Recommendations for the management of cerebral and cerebellar infarction with swelling: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:1222–38.
Kannel WB, Wilson PW, Zhang TJ. The epidemiology of impaired glucose tolerance and hypertension. Am Heart J. 1991;121:1268–73.
Seshadri S, Wolf PA. Modifiable risk factors and determinants of stroke. In: Grotta JC, Albers GW, Broderick JP, Kasner SE, Lo EH, Mendelow AD, Sacco RL, Wong LKS, editors. Stroke: pathology, diagnosis, and management. 6th ed. Beijing: Elsevier; 2016. p. 217–33.
Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359:1577–89.
Meschia JF, Bushnell C, Boden-Albala R, Braun LT, Bravata DM, Chaturvedi S, et al. Guidelines for the primary prevention of stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:3754–832.
Lawes CM, Bennett DA, Feigin VL, Rodgers A. Blood pressure and stroke: an overview of published reviews. Stroke. 2004;35:1024.
Furie KL, Kasner SE, Adams RJ, Albers GW, Bush RL, Fagan SC, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack. A guideline for healthcare professionals from the American Heart Association/American Stroke Association council on stroke. Stroke. 2011;42:227–76.
Lyden P, Raman R, Liu L, Grotta J, Broderick J, Olson S, et al. NIHSS training and certification using a new digital video disk in reliable. Stroke. 2005;36:2446–9.
Johnston SC, Rothwell PM, Nguyen Huynh MN, Giles MF, Elkins JS, Bernstein AL, et al. Validation and refinement of scores to predict very early stroke risk after transient ischemic attack. Lancet. 2007;369:283–92.
Thai CV risk score. Accessed 29 Jan 2018, at https://med.mahidol.ac.th/cardio_vascular_risk/thai_cv_risk_score/.
Brainin M, Teuschl Y, Matz K. Comman risk factors and prevention. In: Brainin M, Heiss WD, editors. Textbook of stroke medicine. 1st ed. New York: Cambridge University Press; 2010. p. 89–104.
Goldstein LB, Sacco RL. Preventing a first stroke. In: Grotta JC, Albers GW, Broderick JP, Kasner SE, Lo EH, Mendelow AD, Sacco RL, Wong LKS, editors. Stroke: pathology, diagnosis, and management. 6th ed. Beijing: Elsevier; 2016. p. 280–91.
Acknowledgments
The authors would like to express their thanks to the participants and staff for their cooperation and participation in the study, and also wish to extend our deep appreciation to those who are not mentioned here for their kindness and encouragement. This study was supported for publication by the Faculty of Public Health, Mahidol University, Bangkok, Thailand.
Author information
Authors and Affiliations
Contributions
W.C. carried out the data collection and drafted the manuscript. W.B. undertook the literature searches. All authors conceived the study idea, participated in its design, and performed the statistical analyses. All authors have read and approved the final version to be published.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest on finance and non-finance.
Ethical approval
The study protocol was reviewed and approved by the Ethics Committee for Research in Human Subjects of the Faculty of Public Health, Mahidol University (171/2557), the Ethics Committee for Research in Human Subjects of the Chachoengsao Public Health Office (PH_CCO_REC 004/58), and the Ethics Committee for Research of the Bhuddasothorn hospital (BSH-IRB 005/2558). The information was collected using medical records. Confidentiality was well maintained using an anonymous technique throughout the study to ensure privacy and the results were analyzed as a whole group.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chaveepojnkamjorn, W., Boorasri, W., Viwatwongkasem, C. et al. Association between hemoglobin A1c and acute ischemic stroke among patients with type-2 diabetes: a case-control study. Int J Diabetes Dev Ctries 40, 555–560 (2020). https://doi.org/10.1007/s13410-020-00806-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-020-00806-7