Abstract
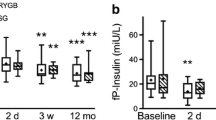
This study aims to investigate the changing characteristics of glucose regulation after gastric surgery for normal gastric cancer patients with type 2 diabetes mellitus (T2DM) (T2DM group) and without T2DM (normal group) in a tertiary hospital located in western China. We conducted a case-control study which retrospectively collected the data of 73 patients: (1) diagnosed as gastric cancer, (2) underwent sub-gastrectomy and Billroth II gastrointestinal anastomosis between October 2007 and December 2012, and (3) did not suffer a recurrent cancer and with sufficient clinical data. Fasting blood glucose (FBG), glycated hemoglobin (HbA1c), insulin sensitive index (HOMA-IS), insulin resistance index (HOMA-IR), and beta cell function index (HOMA-BCF) were compared at baseline and postoperative 7, 14, 28, 56, 120, and 356 days. Baseline FBG, HbA1c, HOMA-IS, HOMA-IR, and HOMA-BCF in the T2DM group were significantly higher than those in the normal group. Immediate postoperative glucose changed significantly, and it became stable and normal during follow-up period in both the T2DM and normal group that there was no significance anymore after postoperative 28 days between them. Normal patients with T2DM would benefit from gastric surgery in glucose control, and it may involve not only decreased food intake and weight loss but also gastrointestinal reconstruction.





Similar content being viewed by others
References
Adeghate E, Schattner P, Dunn E. An update on the etiology and epidemiology of diabetes mellitus. Ann N Y Acad Sci. 2006;1084:1–29.
Zuo H, Shi Z, Hussain A. Prevalence, trends and risk factors for the diabetes epidemic in china: a systematic review and meta-analysis. Diabetes Res Clin Pract. 2014;104(1):63–72.
Du T, Sun X, Huo R, et al. Visceral adiposity index, hypertriglyceridemic waist and risk of diabetes: the china health and nutrition survey 2009. Int J Obes. 2014;38(6):840–7.
Tseng CH. Diabetes conveys a higher risk of gastric cancer mortality despite an age-standardised decreasing trend in the general population in Taiwan. Gut. 2011;60:774e779.
Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2015;38(1):140–9.
Musella M, Milone M, Bellini M, Sosa Fernandez L, Leongito M, et al. Effect of bariatric surgery on obesity-related infertility. Surg Obes Relat Dis. 2012;8:445–9.
Klein S, Ghosh A, Cremieux PY, et al. Economic impact of the clinical benefits of bariatric surgery in diabetes patients with BMI≥ 35 kg/m2. Obesity. 2011;19(3):581–7.
Lifshitz F, Hall J. Reduction in the incidence of type II diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403.
Heymsfield S, Segal K, Hauptman J, Lucas C, Boldrin M, et al. Effects of weight loss with orlistat on glucose tolerance and progression to type 2 diabetes in obese adults. Arch Intern Med. 2000;160:1321–6.
Picot J, Jones J, Colquitt J, Gospodarevskaya E, Loveman E, et al. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess. 2009;13:1–190.
Zhu Z, Shan X, Cheng Y, et al. Clinical course of diabetes after gastrectomy according to type of reconstruction in patients with concurrent gastric cancer and type 2 diabetes. Obes Surg. 2015;25(4):673–9.
Liu T, Xie G, Tian Q, et al (2015) Radical gastrectomy combined with modified gastric bypass surgery for gastric cancer patients with type 2 diabetes. Cell Biochem Biophys: 1–6
Zimmet P, Shaw J, Alberti K. Preventing type 2 diabetes and the dysmetabolic syndrome in the real world: a realistic view. Diabet Med. 2003;20:693–702.
Emoto M, Nishizawa Y, Maekawa K, Hiura Y, Kanda H, et al. Homeostasis model assessment as a clinical index of insulin resistance in type 2 diabetic patients treated with sulfonylureas. Diabetes Care. 1999;22:818–22.
Levy J, Matthews D, Hermans M. Correct homeostasis model assessment (HOMA) evaluation uses the computer program. Diabetes Care. 1998;21:2191–2.
O’Brien PE, McPhail T, Chaston TB, Dixon JB. Systematic review of medium-term weight loss after bariatric operations. Obes Surg. 2006;16:1032–40.
Schauer PR, Burguera B, Ikramuddin S, Cottam D, Gourash W, et al. Effect of laparoscopic roux-en Y gastric bypass on type 2 diabetes mellitus. Ann Surg. 2003;238:467.
Li Q, Chen L, Yang Z, Huang Y, He M, et al. Metabolic effects of bariatric surgery in type 2 diabetic patients with body mass index < 35 kg/m2. Diabetes Obes Metab. 2012;14:262–70.
Shimizu H, Timratana P, Schauer P, Rogula T. Review of metabolic surgery for type 2 diabetes in patients with a BMI <35 Kg/M 2. J Obes. 2012;2012:147256.
Dixon J, le Roux C, Rubino F, Zimmet P. Bariatric surgery for type 2 diabetes. Lancet. 2012;379:2300–11.
Mingrone S, Panunzi A, Mingrone G, Panunzi S, de Gaetano A, Guidone C, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012;366:1577–85.
Camastra S, Manco M, Mari A, Greco A, Frascerra S, et al. β-cell function in severely obese type 2 diabetic patients long-term effects of bariatric surgery. Diabetes Care. 2007;30:1002–4.
Rao RS, Kini S. GIP and bariatric surgery. Obes Surg. 2011;21:244–52.
Rubino F, Schauer P, Kaplan L, Cummings D. Metabolic surgery to treat type 2 diabetes: clinical outcomes and mechanisms of action. Annu Rev Med. 2010;61:393–411.
Buchwald H, Avidor Y, Braunwald E, Jensen M, Pories W, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37.
Ali M, Bullard K, Saaddine J, Cowie C, Imperatore G, et al. Achievement of goals in US diabetes care, 1999–2010. N Engl J Med. 2013;368:1613–24.
Bakris G. Clinical guidelines: blood pressure goals in T2DM: a Latin American perspective. Nat Rev Endocrinol. 2013;9:138–9.
Massi-Benedetti M. Changing targets in the treatment of type 2 diabetes. Curr Med Res Opin. 2006;22:S5–S13.
Guo X, Liu X, Wang M, Wei F, Zhang Y, et al. The effects of bariatric procedures versus medical therapy for obese patients with type 2 diabetes: meta-analysis of randomized controlled trials. BioMed Res Int. 2013;2013:410609.
Compliance with ethical standards
Funding
This study was funded by Gansu Provincial Health Department of Research Projects (grant number WST07-07).
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Authors’ contributions
Zhang YC, Wang HL, Zhang YW, and Xu XD were involved in the study conception and design. Wei FX, Han W, and Zhang HH participated in the acquisition of data. Wei ZG, Zhang YW, Wang MC, and Xu XD were involved in the analysis and interpretation of data. Wei FX and Han W participated in the drafting of manuscript. Zhang YC and Wang HL were involved in the critical revision of manuscript.
Conflict of interest
You Cheng Zhang, Feng Xian Wei, Wei Han, Hui Lin Wang, Man Cai Wang, Ya Wu Zhang, Xiao Dong Xu, and Hui Han Zhang declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, Y.C., Wei, F.X., Han, W. et al. Impact of sub-gastrectomy on glucose regulation in gastric cancer patients with T2DM: a follow-up study. Int J Diabetes Dev Ctries 36, 89–94 (2016). https://doi.org/10.1007/s13410-015-0437-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-015-0437-6