Abstract
Purpose
Aberrant fibroblast growth factor receptor (FGFR) expression is thought to contribute to the development of many types of cancer. As yet, however, their impact on the course and prognosis of head and neck cancer remains to be determined. Here, we aimed to investigate the effects of expression of the FGFR family members FGFR1 and FGFR3, as well as their downstream PI3K/AKT signal-regulated kinases, on the aggressiveness and prognosis of laryngeal cancer.
Methods
In total 137 surgically removed squamous cell laryngeal cancer (SCLC) and 100 matched non-cancerous laryngeal mucosa (NCLM) samples were assessed for mRNA expression using quantitative real-time PCR. The corresponding proteins were analyzed by Western blotting. SLUG expression was assessed by immunohistochemistry. The expression data were subsequently related to tumor front grading (TFG), local/nodal recurrences, prognosis and overall survival.
Results
The FGFR1, FGFR3 and PI3K/AKT kinase mRNA and protein levels were found to be significantly higher in the SCLC than the NCLM samples (p < 0.05). A high FGFR1 mRNA/protein expression level was found to be associated with an increased invasion rate, according to TFG scale and SLUG level, a high local/nodal recurrence rate and a poor prognosis (p < 0.05). Similarly, we found that a high FGFR3 mRNA/protein expression level was associated with a shorter survival time (p < 0.05). In addition, we found that high PI3K/AKT kinase mRNA/protein levels were associated with a high TFG (p < 0.05). We also found that FGFR1/3 mRNA and FGFR1 protein levels were inversely associated with overall survival (log-rank test: FGFR1 mRNA p = 0.03, FGFR3 mRNA p = 0.04, FGFR1 protein p = 0.03). Subsequent multivariate analyses revealed that high FGFR3 mRNA expression may serve as an independent poor prognostic factor (HR 2.32, 95% CI 1.03–6.59; p = 0.04). We also found that the p-PI3K regulatory kinase protein level was significantly associated with survival in the cohort studied (HR 1.78, 95% CI 0.64–8.53; p = 0.03).
Conclusions
From our data we conclude that FGFR1 and FGFR3, as well as its downstream regulatory PI3K/AKT kinases, may serve as potential biomarkers for the invasiveness and prognosis of laryngeal cancer. The expression of FGFR1/3-PI3K/AKT regulatory pathway members may be instrumental for the identification of patients at risk for an unfavorable clinical outcome.



Similar content being viewed by others
References
B.W. Stewart, C.P. Wild, World Cancer Report 2014 (Lyon, France, International Agency for Research on Cancer, 2015), IARC Publications Website: http://publications.iarc.fr/Non-Series-Publications/World-Cancer-Reports/World-Cancer-Report-2014
K.D. Miller, R.L. Siegel, C.C. Lin, A.B. Mariotto, J.L. Kramer, J.H. Rowland, K.D. Stein, R. Alteri, A. Jemal, Cancer treatment and survivorship statistics. CA Cancer J. Clin. 66, 271–289 (2016)
R.L. Siegel, K.D. Miller, A. Jemal, Cancer statistics. CA Cancer J. Clin. 66, 7–30 (2016)
S. Bhattacharyya, V. Sekar, B. Majumder, D.G. Mehrotra, S. Banerjee, A.K. Bhowmick, N. Alam, G.K. Mandal, J. Biswas, P.K. Majumder, N. Murmu, CDKN2A-p53 mediated antitumor effect of Lupeol in head and neck cancer. Cell Oncol 40, 145–155 (2017). https://doi.org/10.1007/s13402-016-0311-7
L. Kadletz, G. Heiduschka, R. Wiebringhaus, E. Gurnhofer, U. Kotowski, G. Haymerle, M. Brunner, C. Barry, L. Kenner, ELMO3 expression indicates a poor prognosis in head and neck squamous cell carcinoma-a short report. Cell Oncol 40, 193–198 (2017). https://doi.org/10.1007/s13402-016-0310-8
L. Zhou, L.T. Yao, Z.Y. Liang, W.X. Zhou, L. You, Q.Q. Shao, S. Huang, J.C. Guo, Y.P. Zhao, Nuclear translocation of fibroblast growth factor receptor 3 and its significance in pancreatic cancer. Int. J. Clin. Exp. Pathol. 8, 14640–11468 (2015)
X. Liu, W. Zhang, D. Geng, J. He, Y. Zhao, L. Yu, Clinical significance of fibroblast growth factor receptor-3 mutations in bladder cancer: a systematic review and meta-analysis. Genet. Mol. Res. 13, 1109–1120 (2014)
J.Y. Sung, J.M. Sun, B. Chang Jeong, S. Il Seo, S. Soo Jeon, H. Moo Lee, H. Yong Choi, S. Young Kang, Y.L. Choi, G. Young Kwon, FGFR3 overexpression is prognostic of adverse outcome for muscle-invasive bladder carcinoma treated with adjuvant chemotherapy. Urol. Oncol. 32, 49.e23–49.e31 (2014). https://doi.org/10.1016/j.urolonc.2013.07.015
C. Poyet, T. Hermanns, Q. Zhong, E. Drescher, D. Eberli, M. Burger, F. Hofstaedter, A. Hartmann, R. Stöhr, E.C. Zwarthoff, T. Sulser, P.J. Wild, Positive fibroblast growth factor receptor 3 immunoreactivity is associated with low-grade non-invasive urothelial bladder cancer. Oncol. Lett. 10, 2753–2760 (2015)
E.A. Guancial, L. Werner, J. Bellmunt, A. Bamias, T.K. Choueiri, R. Ross, F.A. Schutz, R.S. Park, R.J. O'Brien, M.S. Hirsch, J.A. Barletta, D.M. Berman, R. Lis, M. Loda, E.C. Stack, L.A. Garraway, M. Riester, F. Michor, P.W. Kantoff, J.E. Rosenberg, FGFR3 expression in primary and metastatic urothelial carcinoma of the bladder. Cancer Med. 3, 835–844 (2014)
K. Koole, P.M. van Kempen, J.E. Swartz, T. Peeters, P.J. van Diest, R. Koole, R.J. van Es, S.M. Willems, Fibroblast growth factor receptor 3 protein is overexpressed in oral and oropharyngeal squamous cell carcinoma. Cancer Med. 5, 275–284 (2016)
F. Göke, M. Bode, A. Franzen, R. Kirsten, D. Goltz, A. Göke, R. Sharma, D. Boehm, W. Vogel, P. Wagner, C. Lengerke, G. Kristiansen, J. Kirfel, T. Van Bremen, F. Bootz, L.E. Heasley, A. Schröck, S. Perner, Fibroblast growth factor receptor 1 amplification is a common event in squamous cell carcinoma of the head and neck. Mod. Pathol. 26, 1298–1306 (2013)
H.S. Kim, S.E. Lee, Y.S. Bae, D.J. Kim, C.G. Lee, J. Hur, H. Chung, J.C. Park, D.H. Jung, S.K. Shin, S.K. Lee, Y.C. Lee, H.R. Kim, Y.W. Moon, J.H. Kim, Y.M. Shim, S.S. Jewell, H. Kim, Y.L. Choi, B.C. Cho, Fibroblast growth factor receptor 1 gene amplification is associated with poor survival in patients with resected esophageal squamous cell carcinoma. Oncotarget 6, 2562–2572 (2015)
S. Bertz, C. Abeé, S. Schwarz-Furlan, J. Alfer, F. Hofstädter, R. Stoehr, A. Hartmann, A.K. Gaumann, Increased angiogenesis and FGFR protein expression indicate a favourable prognosis in bladder cancer. Virchows Arch. 465, 687–695 (2014)
M. Inokuchi, Y. Fujimori, S. Otsuki, Y. Sato, M. Nakagawa, K. Kojima, Therapeutic targeting of fibroblast growth factor receptors in gastric cancer. Gastroenterol Res Pract 2015, 796380 (2015). https://doi.org/10.1155/2015/796380
M. Katoh, FGFR inhibitors: effects on cancer cells, tumor microenvironment and whole-body homeostasis. Int. J. Mol. Med. 38, 3–15 (2016)
A. Desai, A.A. Adjei, FGFR signaling as a target for lung cancer therapy. J. Thorac. Oncol. 11, 9–20 (2016)
R. Dienstmann, J. Rodon, A. Prat, J. Perez-Garcia, B. Adamo, E. Felip, J. Cortes, A.J. Iafrate, P. Nuciforo, J. Tabernero, Genomic aberrations in the FGFR pathway: opportunities for targeted therapies in solid tumors. Ann. Oncol. 25, 552–563 (2014)
F. Biello, G. Burrafato, E. Rijavec, C. Genova, G. Barletta, A. Truini, S. Coco, M.G. Bello, A. Alama, F. Boccardo, F. Grossi, Fibroblast growth factor receptor (FGFR): a new target for non-small cell lung cancer therapy. Anticancer Agents Med. Chem. 16, 1142–1154 (2016)
C. Hierro, J. Rodon, J. Tabernero, Fibroblast growth factor (FGF) Receptor/FGF inhibitors: novel targets and strategies for optimization of response of solid tumors. Semin. Oncol. 42, 801–819 (2015)
T. Helsten, M. Schwaederle, R. Kurzrock, Fibroblast growth factor receptor signaling in hereditary and neoplastic disease: biologic and clinical implications. Cancer Metastasis Rev. 34, 479–496 (2015)
E. Martino, D. Tomlinson, M. Knowles, A decade of FGF receptor research in bladder cancer: past, present, and future. Adv. Urol. 2012, 429213 (2012). https://doi.org/10.1155/2012/429213
D. Tomlinson, E. Baxter, P. Loadman, M.A. Hull, M.A. Knowles, FGFR1-induced epithelial to mesenchymal transition through MAPK/PLCγ/COX-2-mediated mechanisms. PLoS One 7, e38972 (2012). https://doi.org/10.1371/journal.pone.0038972
A. Parish, M. Schwaederle, G. Daniels, D. Piccioni, P. Fanta, R. Schwab, K. Shimabukuro, B.A. Parker, T. Helsten, R. Kurzrock, Fibroblast growth factor family aberrations in cancers: clinical and molecular characteristics. Cell Cycle 14, 2121–2128 (2015)
W. Zhou, Y. Zhu, S. Chen, R. Xu, K. Wang, Fibroblast growth factor receptor 1 promotes MG63 cell proliferation and is associated with increased expression of cyclin-dependent kinase 1 in osteosarcoma. Mol. Med. Rep. 13, 713–719 (2016)
L. Huang, Z. Huang, Y. Fan, L. He, M. Ye, K. Shi, B. Ji, J. Huang, Y. Wang, Q. Li, FOXC1 promotes proliferation and epithelial-mesenchymal transition in cervical carcinoma through the PI3K-AKT signal pathway. Am. J. Transl. Res. 9, 1297–1306 (2017)
C. Wang, W. Gu, Y. Zhang, Y. Ji, Y. Wen, X. Xu, Nicotine promotes cervical carcinoma cell line HeLa migration and invasion by activating PI3k/Akt/NF-κB pathway in vitro. Exp Toxicol Pathol 69, 402–407 (2017). https://doi.org/10.1016/j.etp.2017.03.006
L. Chen , H. Fu H, Y. Luo, L. Chen, R. Cheng, N. Zhang, H. Guo, cPLA2α mediates TGF-β-induced epithelial-mesenchymal transition in breast cancer through PI3k/Akt signaling. Cell Death Dis (2017) doi: https://doi.org/10.1038/cddis.2017.152, 8, 4, e2728
Y. Li, G. Guo, J. Song, B7-H3 promotes the migration and invasion of human bladder cancer cells via the PI3K/Akt/STAT3 signaling pathway. J. Cancer 8, 816–824 (2017)
J. Gao, B.A. Aksoy, U. Dogrusoz, G. Dresdner, B. Gross, S.O. Sumer, Y. Sun, A. Jacobsen, R. Sinha, E. Larsson, E. Cerami, C. Sander, N. Schultz, Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci Signal 6(269), pl1 (2013). https://doi.org/10.1126/scisignal.2004088
The Cancer Genome Atlas Network (TCGA), Comprehensive genomic characterization of head and neck squamous cell carcinomas. Nature 517, 576–582 (2015). https://doi.org/10.1038/nature14129 (online document http://www.cbioportal.org/study?id=hnsctcga#summary. Accessed 14 September 2017)
L.G.T. Morris, R. Chandramohan, L. West, A. Zehir, D. Chakravarty, D.G. Pfister, R.J. Wong, N.Y. Lee, E.J. Sherman, S.S. Baxi, I. Ganly, B. Singh, J.P. Shah, A.R. Shaha, J.O. Boyle, S.G. Patel, B.R. Roman, C.A. Barker, S.M. McBride, T.A. Chan, S. Dogan, D.M. Hyman, M.F. Berger, D.B. Solit, N. Riaz, A.L. Ho, The molecular landscape of recurrent and metastatic head and neck cancers insights from a precision oncology sequencing platform. JAMA Oncol. https://doi.org/10.1001/jamaoncol.2016.1790 (online document http://www.cbioportal.org/study?id=hncmskcc2016# summary. Accessed 14 September 2017)
N. Stransky, A.M. Egloff, A.D. Tward, A.D. Kostic, K. Cibulskis, A. Sivachenko, G.V. Kryukov, M.S. Lawrence, C. Sougnez, A. McKenna, E. Shefler, A.H. Ramos, P. Stojanov, S.L. Carter, D. Voet, M.L. Cortés, D. Auclair, M.F. Berger, G. Saksena, C. Guiducci, R.C. Onofrio, M. Parkin, M. Romkes, J.L. Weissfeld, R.R. Seethala, L. Wang, C. Rangel-Escareño, J.C. Fernandez-Lopez, A. Hidalgo-Miranda, J. Melendez-Zajgla, W. Winckler, K. Ardlie, S.B. Gabriel, M. Meyerson, E.S. Lander, G. Getz, T.R. Golub, L.A. Garraway, J.R. Grandis, The mutational landscape of head and neck squamous cell carcinoma. Science 333, 1157–1160 (2011) (online document http://www.cbioportal.org/study?id=hnsc broad#summary. Accessed 14 Sept 2017)
N.A. Ipenburg, K. Koole, K.S. Liem, P.M. van Kempen, R. Koole, P.J. van Diest, R.J. van Es, S.M. Willems, Fibroblast growth factor receptor family members as prognostic biomarkers in head and neck squamous cell carcinoma: a systematic review. Target Oncol. 11, 17–27 (2016)
F. Göke, A. Franzen, T.K. Hinz, L.A. Marek, P. Yoon, R. Sharma, M. Bode, A. von Maessenhausen, B. Lankat-Buttgereit, A. Göke, C. Golletz, R. Kirsten, D. Boehm, W. Vogel, E.K. Kleczko, J.R. Eagles, F.R. Hirsch, T. Van Bremen, F. Bootz, A. Schroeck, J. Kim, A.C. Tan, A. Jimeno, L.E. Heasley, S. Perner, FGFR1 expression levels predict BGJ398 sensitivity of FGFR1-dependent head and neck squamous cell cancers. Clin. Cancer Res. 21, 4356–4364 (2015)
B.N. Tillman, M. Yanik, A.C. Birkeland, C.J. Liu, D.H. Hovelson, A.K. Cani, N. Palanisamy, S. Carskadon, T.E. Carey, C.R. Bradford, S.A. Tomlins, J.B. McHugh, M.E. Spector, J.C. Brenner, Fibroblast growth factor family aberrations as a putative driver of head and neck squamous cell carcinoma in an epidemiologically low-risk patient as defined by targeted sequencing. Head Neck 38(Suppl 1), E1646–E1652 (2016). https://doi.org/10.1002/hed.24292
Y. Yu, T. Hall, S. Eathiraj, M.J. Wick, B. Schwartz, G. Abbadessa, In-vitro and in-vivo combined effect of ARQ 092, an AKT inhibitor, with ARQ 087, a FGFR inhibitor. Anti-Cancer Drugs 28, 503–513 (2017). https://doi.org/10.1097/CAD.0000000000000486
S. Feng, L. Shao, P. Castro, I. Coleman, P.S. Nelson, P.D. Smith, B.R. Davies, M. Ittmann, Combination treatment of prostate cancer with FGF receptor and AKT kinase inhibitors. Oncotarget 8, 6179–6192 (2017)
J.J. Wheler, J.T. Atkins, F. Janku, S.L. Moulder, P.J. Stephens, R. Yelensky, V. Valero, V. Miller, R. Kurzrock, F. Meric-Bernstam, Presence of both alterations in FGFR/FGF andPI3K/AKT/mTOR confer improved outcomes for patients with metastatic breast cancer treated with PI3K/AKT/mTOR inhibitors. Oncoscience 3, 164–172 (2016)
J.W. Lin, X. Li, M.L. Qiu, R.G. Luo, J.B. Lin, B. Liu, PI3K overexpression and PIK3CA mutations are associated with age, tumor staging, and other clinical characteristics in Chinese patients with esophageal squamous cell carcinoma. Genet Test. Mol. Biomarkers 21, 236–241 (2017)
S.B. Edge, C.C. Compton, The American joint committee on cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann. Surg. Oncol. 17, 1471–1474 (2010)
L. Barnes, J.W. Eveson, P. Reichart. IARC WHO classification of tumours. Pathology and genetics of head and neck tumours. Third edition. (2005) ISBN-13: 9789283224174
K. Starska, E. Forma, P. Jóźwiak, M. Bryś, I. Lewy-Trenda, E. Brzezińska-Błaszczyk, A. Krześlak, Gene and protein expression of glucose transporter 1 and glucose transporter 3 in human laryngeal cancer-the relationship with regulatory hypoxia-inducible factor-1α expression, tumor invasiveness, and patient prognosis. Tumour Biol. 36, 2309–2321 (2015)
K. Starska, E. Forma, M. Nowacka-Zawisza, I. Lewy-Trenda, P. Ciesielski, W. Pietruszewska, M. Skóra, M. Bryś, The c.*229C > T gene polymorphism in 3'UTR region of the topoisomerase IIβ binding protein 1 gene and LOH in BRCA1/2 regions and their effect on the risk and progression of human laryngeal carcinoma. Tumour Biol. 37, 4541–4557 (2016)
K. Starska, E. Forma, P. Jóźwiak, I. Lewy-Trenda, M. Danilewicz, O. Stasikowska-Kanicka, M. Skóra, K. Kolary, J. Miazga, A. Krześlak, M. Bryś, Gene/protein expression of CAPN1/2-CAST system members is associated with ERK1/2 kinases activity as well as progression and clinical outcome in human laryngeal cancer. Tumour Biol. 37, 13185–13203 (2016)
E. Forma, K. Wójcik-Krowiranda, P. Jóźwiak, A. Szymczyk, A. Bieńkiewicz, M. Bryś, A. Krześlak, Topoisomerase IIβ binding protein 1 c.*229C>T (rs115160714) gene polymorphism and endometrial cancer risk. Pathol. Oncol. Res. 20, 597–602 (2014)
S. Zheng, C. Yang, M. Lu, Q. Liu, T. Liu, F. Dai, X. Gao, I. Sheyhidin, X. Lu, PIK3CA promotes proliferation and motility but is unassociated with lymph node metastasis or prognosis in esophageal squamous cell carcinoma. Hum. Pathol. 53, 121–129 (2016)
T. Helsten, S. Elkin, E. Arthur, B.N. Tomson, J. Carter, R. Kurzrock, The FGFR landscape in cancer: analysis of 4,853 tumors by next-generation sequencing. Clin. Cancer. Res. 22, 259–267 (2016)
J. Taeger, C. Moser, C. Hellerbrand, M.E. Mycielska, G. Glockzin, H.J. Schlitt, E.K. Geissler, O. Stoeltzing, S.A. Lang, Targeting FGFR/PDGFR/VEGFR impairs tumor growth, angiogenesis, and metastasis by effects on tumor cells, endothelial cells, and pericytes in pancreatic cancer. Mol. Cancer Ther. 10, 2157–2167 (2011)
R. Paduch, The role of lymphangiogenesis and angiogenesis in tumor metastasis. Cell Oncol 39, 397–410 (2016). https://doi.org/10.1007/s13402-016-0281-9
Acknowledgements
This work was supported, in part, by a grant from the statutory fund of the Department of Cytobiochemistry, Faculty of Biology and Environmental Protection, University of Łódź, Poland (506/811) and by the National Science Council, Poland (N403 043 32/2326).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the Bioethical Commission of the Medical University of Łódź, Poland (approval No RNN/80/16/KE). Informed consent was obtained from all participants included in the study.
Competing interests
The authors declare that they have no competing interests.
Electronic supplementary material
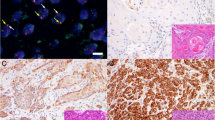
Supplementary Fig. 1
Spearman rank analysis results for FGFR1 and FGFR3 mRNA/protein expression level in relation to PI3K/AKT measured by real-time PCR and Western blotting analyses in laryngeal cancers. a Spearman rank analysis results for FGFR1 gene level in relation to PI3K and b AKT genes. c Spearman rank analysis results for FGFR1 protein level in relation to total-PI3K and d AKT proteins as well as for e phospho-PI3K and f AKT proteins. g Spearman rank analysis results for FGFR3 mRNA expression level in relation to PI3K and h AKT genes. i Spearman rank analysis results for FGFR3 protein expression level in relation to total-PI3K and j AKT proteins as well as for k phospho-PI3K and l AKT proteins. (EPS 4571 kb)
Supplementary Fig. 2
Expression of FGFR1, FGFR3, PI3K and AKT mean mRNA measured by real-time PCR in laryngeal cancers. a A comparison between subgroups with tumor size (pT status) according to FGFR1 and g FGFR3 genes. b A comparison between subgroups with total score of tumor front grading according to FGFR1 and h FGFR3 transcripts. c A comparison between subgroups with depth of invasion according to to FGFR1 and i FGFR3 genes. d A comparison between subgroups with mode of invasion according to FGFR1 and j FGFR3 transcripts. e A comparison between subgroups with local recurrences according to FGFR1 and k FGFR3 genes. f A comparison between subgroups with five-year disease-free (5y–DF) survival according to FGFR1 and l FGFR3 transcripts. Graphs represent mean ± standard deviation. P values were calculated by the Mann-Whitney U-test. *P < 0.05, **p < 0.01 (EPS 4428 kb)
Supplementary Fig. 3
Expression of FGFR1/3 and phospho-PI3K/AKT mean protein levels measured by Western blotting in laryngeal cancers. a A comparison between subgroups with tumor size (pT status) according to FGFR1 and g FGFR3 proteins. b A comparison between subgroups with total score of tumor front grading according to FGFR1 and h FGFR3 proteins. c A comparison between subgroups with depth of invasion according to to FGFR1 and i FGFR3 proteins. d A comparison between subgroups with mode of invasion according to FGFR1 and j FGFR3 proteins. e A comparison between subgroups with local recurrences according to FGFR1 and k FGFR3 proteins. f A comparison between subgroups with five-year disease-free (5y–DF) survival according to FGFR1 and l FGFR3 proteins. Graphs represent mean ± standard deviation. P values were calculated by the Mann-Whitney U-test. *P < 0.05, **p < 0.01 (EPS 4186 kb)
Rights and permissions
About this article
Cite this article
Starska, K., Forma, E., Lewy-Trenda, I. et al. Fibroblast growth factor receptor 1 and 3 expression is associated with regulatory PI3K/AKT kinase activity, as well as invasion and prognosis, in human laryngeal cancer. Cell Oncol. 41, 253–268 (2018). https://doi.org/10.1007/s13402-017-0367-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13402-017-0367-z