Abstract
Background
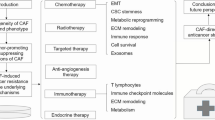
Cytotoxic chemotherapy improves survival for some, but not all, cancer patients. Non-responders may experience unnecessary toxicity and cancer progression, thus creating an urgent need for biomarkers that can predict the response to chemotherapy. So far, the search for such biomarkers has primarily been focused on the cancer cells and less on their surrounding stroma. This stroma is known to act as a key regulator of tumour progression and, in addition, has been associated with drug delivery and drug efficacy. Fibroblasts represent the major cell type in cancer-associated stroma and they secrete extracellular matrix proteins as well as growth factors. This Medline-based literature review summarises the results from studies on epithelial cancers and aimed at investigating relationships between the quantity and quality of the intra-tumoral stroma, the cancer-associated fibroblasts, the proteins they produce and the concomitant response to chemotherapy. Biomarkers were selected for review that are known to affect cancer-related characteristics and patient prognosis.
Results
The current literature supports the hypothesis that biomarkers derived from the tumour stroma may be useful to predict response to chemotherapy. This notion appears to be related to the overall quantity and cellularity of the intra-tumoural stroma and the predominant constituents of the extracellular matrix.
Conclusion
Increasing evidence is emerging showing that tumour-stroma interactions may not only affect tumour progression and patient prognosis, but also the response to chemotherapy. The tumour stroma-derived biomarkers that appear to be most appropriate to determine the patient’s response to chemotherapy vary by tumour origin and the availability of pre-treatment tissue. For patients scheduled for adjuvant chemotherapy, the most promising biomarker appears to be the PLAU: SERPINE complex, whereas for patients scheduled for neo-adjuvant chemotherapy the tumour stroma quantity appears to be most relevant.


Similar content being viewed by others
Abbreviations
- CAF:
-
cancer associated fibroblast
- CMF:
-
cyclophosphamide methotrexate and 5-fluorouracil
- CTGF:
-
connective tissue growth factor
- ECM:
-
extracellular matrix
- EFEMP1:
-
fibulin 3
- ELISA:
-
enzyme linked immunosorbent assay
- FBLN1:
-
fibulin 1
- FN1:
-
fibronectin
- HA:
-
hyaluronan
- HGF:
-
hepatocyte growth factor
- MMP:
-
matrix metalloproteinase
- PTK:
-
protein tyrosine kinase
- SCLC:
-
small cell lung cancer
- SDC1:
-
syndecan 1
- SERPINE1:
-
serine protease inhibitor type-1
- SPARC:
-
secreted protein, acidic, cysteine-rich
- TIMP1:
-
tissue inhibitor of metalloproteinase-1
- PLAU:
-
urokinase-type plasminogen activator
References
D. Hanahan, R.A. Weinberg, S. Francisco, The hallmarks of cancer. Cell. 100, 57–70 (2000)
G. Chong, D. Cunningham, Oesophageal cancer: preoperative chemotherapy. Ann. Oncol. 15(Suppl 4), iv87–iv91 (2004)
N. Tamura, T. Hasebe, N. Okada, T. Houjoh, S. Akashi-Tanaka, C. Shimizu, T. Shibata, Y. Sasajima, M. Iwasaki, T. Kinoshita, Tumor histology in lymph vessels and lymph nodes for the accurate prediction of outcome among breast cancer patients treated with neoadjuvant chemotherapy. Cancer Sci. 100, 1823–1833 (2009)
The Cochrane Collaboration: Advanced Bladder Cancer Meta-analysis Collaboration, Neoadjuvant chemotherapy for invasive bladder cancer (Review). The Cochrane Library. (2008).
E. Kent, M. Hussain, Neoadjuvant Therapy for Prostate Cancer: An Oncologist’s Perspective. Rev Urol. 5(Suppl 3), S28–S37 (2003)
T. Delaunoit, S.R. Alberts, D.J. Sargent, E. Green, R.M. Goldberg, J. Krook, C. Fuchs, R.K. Ramanathan, S.K. Williamson, R.F. Morton, B.P. Findlay, Chemotherapy permits resection of metastatic colorectal cancer: experience from Intergroup N9741. Ann. Oncol. 16, 425–429 (2005)
Network National Comprehensive Cancer, Network National Comprehensive Cancer. Clinical practice guidelines in oncology, ovarian cancer including fallopian tube cancer and primary peritoneal cancer version 2. Clinical Practice Guidelines in Oncology. (2011).
S. Heinrich, M. Schäfer, A. Weber, T.F. Hany, U. Bhure, B.C. Pestalozzi, P. Clavien, Neoadjuvant chemotherapy generates a significant tumor response in resectable pancreatic cancer without increasing morbidity: results of a prospective phase II trial. Ann. Surg. 248, 1014–1022 (2008)
S. Burdett, L. Stewart, Rydzewska, Chemotherapy and surgery versus surgery alone in non-small cell lung cancer. Cochrane Database Syst Rev. (2007).
J. Neoptolemos, J. Dunn, D. Stocken, J. Almond, K. Link, H. Beger, C. Bassi, M. Falconi, P. Pederzoli, C. Dervenis, L. Fernandez-Cruz, F. Lacaine, A. Pap, D. Spooner, D. Kerr, H. Friess, M. Büchler, Adjuvant chemoradiotherapy and chemotherapy in resectable pancreatic cancer: a randomised controlled trial. Lancet. 358, 1576–1585 (2001)
J. Pignon, H. Tribodet, G. Scagliotti, J. Douillard, F. Shepherd, R. Stephens, A. Dunant, V. Torri, R. Rosell, L. Seymour, S.G. Spiro, E. Rolland, R. Fossati, D. Aubert, K. Ding, D. Waller, T. Le Chevalier, Lung adjuvant cisplatin evaluation: a pooled analysis by the LACE Collaborative Group. J. Clin. Oncol. 26, 3552–3559 (2008)
G. Bonadonna, E. Brusamolino, P. Valagussa, A. Rossi, L. Brugnatelli, C. Brambilla, M. De Lena, G. Tancini, E. Bajetta, R. Musumeci, U. Veronesi, Combination chemotherapy as an adjuvant treatment in operable breast cancer. N. Engl. J. Med. 294, 405–410 (1976)
R. Gray, J. Barnwell, C. McConkey, R. Hills, N. Williams, D. Kerr, Adjuvant chemotherapy versus observation in patients with colorectal cancer: a randomised study. Lancet 370, 2020–2029 (2007)
S. Wöhrer, M. Raderer, M. Hejna, Palliative chemotherapy for advanced gastric cancer. Ann. Oncol. 15, 1585–1595 (2004)
P. Simmonds, Palliative chemotherapy for advanced colorectal cancer: systematic review and meta-analysis. Colorectal Cancer Collaborative Group. BMJ 321, 531–535 (2000)
I. Smith, Palliative chemotherapy for advanced non-small cell lung cancer. BMJ. 308, 429–430 (1994)
T. Petit, C. Borel, J.P. Ghnassia, J.F. Rodier, A. Escande, R. Mors, P. Haegelé, Chemotherapy response of breast cancer depends on HER-2 status and anthracycline dose intensity in the neoadjuvant setting. Clin. Cancer Res. 7, 1577–1581 (2001)
F. Penault-Llorca, A. Vincent-Salomon, Roles of the pathologist in neoadjuvant chemotherapy: evaluation of response, prognostic and predictive factors. Ann Pathol. 23, 555–563 (2003)
M.G. Daidone, R. Silvestrini, A. Luisi, M. Mastore, E. Benini, S. Veneroni, C. Brambilla, L. Ferrari, M. Greco, S. Andreola, Changes in biological markers after primary chemotherapy for breast cancers. Int. J. Cancer. 61, 301–305 (1995)
V. Cavaillès, A. Gompel, M.C. Portois, S. Thénot, N. Mabon, F. Vignon, Comparative activity of pulsed or continuous estradiol exposure on gene expression and proliferation of normal and tumoral human breast cells. J. Mol. Endocrinol. 28, 165–175 (2002)
D. Hanahan, R.A. Weinberg, Hallmarks of cancer: the next generation. Cell. 144, 646–674 (2011)
M. Allen, J. Jones, Jekyll and Hyde: the role of the microenvironment on the progression of cancer. J. Pathol. 223, 162–176 (2011)
B. Elenbaas, R.A. Weinberg, Heterotypic signaling between epithelial tumor cells and fibroblasts in carcinoma formation. Exp. Cell Res. 264, 169–184 (2001)
T.D. Tlsty, P.W. Hein, Know thy neighbor: stromal cells can contribute oncogenic signals. Curr. Opin. Genet. Dev. 11, 54–59 (2001)
A.F. Olumi, G.D. Grossfeld, S.W. Hayward, P.R. Carroll, T.D. Tlsty, G.R. Cunha, Carcinoma-associated fibroblasts direct tumor progression of initiated human prostatic epithelium. Cancer Res. 59, 5002–5011 (1999)
H. Kiaris, I. Chatzistamou, C. Kalofoutis, H. Koutselini, C. Piperi, A. Kalofoutis, Tumour-stroma interactions in carcinogenesis: basic aspects and perspectives. Mol. Cell. Biochem. 261, 117–122 (2004)
A. Orimo, P.B. Gupta, D.C. Sgroi, F. Arenzana-Seisdedos, T. Delaunay, R. Naeem, V.J. Carey, A.L. Richardson, R A Weinberg, Stromal fibroblasts present in invasive human breast carcinomas promote tumor growth and angiogenesis through elevated SDF-1/CXCL12 secretion. Cell. 121, 335–348 (2005)
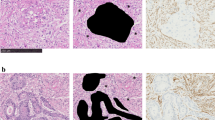
N.P. West, M. Dattani, P. Mcshane, G. Hutchins, J. Grabsch, W. Mueller, D. Treanor, P. Quirke, The proportion of tumour cells is an independent predictor for survival in colorectal cancer patients. Br. J. Cancer. 102, 1519–1523 (2010)
A. Labiche, N. Heutte, P. Herlin, J. Chasle, P. Gauduchon, N. Elie, Stromal compartment as a survival prognostic factor in advanced ovarian carcinoma. Int. J. Gynecol. Cancer. 20, 28–33 (2010)
Y. Wu, H. Grabsch, T. Ivanova, I.B. Tan, J. Murray, C.H. Ooi, A.I. Wright, Nicholas P West, G.G.A. Hutchins, J. Wu, M. Lee, J. Lee, J.H. Koo, K.G. Yeoh, N. van Grieken, B. Ylstra, S.Y. Rha, J.A. Ajani, J.H. Cheong, S.H. Noh, et al., Comprehensive genomic meta-analysis identifies intra-tumoural stroma as a predictor of survival in patients with gastric cancer. Gut. (2012).
E.M. De Kruijf, J.G.H. van Nes, C.J.H. van de Velde, H. Putter, V.T.H.B.M. Smi, G.J. Liefers, P.J.K. Kuppen, R.A. Tollenaar, W.E. Mesker, Tumor-stroma ratio in the primary tumor is a prognostic factor in early breast cancer patients, especially in triple-negative carcinoma patients. Breast Cancer Res. Treat. 125, 687–696 (2011)
E.F.W. Courrech Staal, V.T.H.B.M. Smit, M.-L.F. van Velthuysen, J.M.J. Spitzer-Naaykens, M.W.J.M. Wouters, W.E. Mesker, R.A. Tollenaar, J.W. van Sandick, Reproducibility and validation of tumour stroma ratio scoring on oesophageal adenocarcinoma biopsies. Eur. J. Cancer. 47, 375–382 (2011)
Y. Zhang, H. Tang, J. Cai, T. Zhang, J. Guo, D. Feng, Z. Wang, Ovarian cancer-associated fibroblasts contribute to epithelial ovarian carcinoma metastasis by promoting angiogenesis, lymphangiogenesis and tumor cell invasion. Cancer Lett. 303, 47–55 (2011)
R. Kalluri, M. Zeisberg, Fibroblasts in cancer. Nat. Rev. Cancer. 6, 392–401 (2006)
T. Sethi, R.C. Rintoul, S.M. Moore, A.C. MacKinnon, D. Salter, C. Choo, E.R. Chilvers, I. Dransfield, S.C. Donnelly, R. Strieter, C. Haslett, Extracellular matrix proteins protect small cell lung cancer cells against apoptosis: a mechanism for small cell lung cancer growth and drug resistance in vivo. Nat. Med. 5, 662–668 (1999)
F. Andre, N. Berrada, C. Desmedt, Implication of tumor microenvironment in the resistance to chemotherapy in breast cancer patients. Curr Opin Oncol. 22, 547–551 (2010)
A. Ostman, M. Augsten, Cancer-associated fibroblasts and tumor growth–bystanders turning into key players. Curr. Opin. Genet. Dev. 19, 67–73 (2009)
K. Pietras, K. Rubin, T. Sjöblom, T. Sjo, E. Buchdunger, M. Sjo, Inhibition of PDGF receptor signaling in tumor stroma enhances antitumor effect of chemotherapy. Cancer Res. 62, 5476–5484 (2002)
K. Pietras, A. Östman, M. Sjöquist, M. Sjo, O. Arne, E. Buchdunger, R.K. Reed, C. Heldin, K. Rubin, Inhibition of platelet-derived growth factor receptors reduces interstitial hypertension and increases transcapillary transport in tumors. Cancer Res. 61, 2929–2934 (2001)
M. Sonnenberg, H. van der Kuip, S. Haubeis, P. Fritz, W. Schroth, G. Friedel, W. Simon, T.E. Mürdter, W.E. Aulitzky, Highly variable response to cytotoxic chemotherapy in carcinoma-associated fibroblasts (CAFs) from lung and breast. BMC cancer. 8, 364 (2008)
D. Lafkas, G. Trimis, A.G. Papavassiliou, Hippokratis Kiaris, P53 mutations in stromal fibroblasts sensitize tumors against chemotherapy. Int. J. Cancer. 123, 967–971 (2008)
I. Nakajima, Immunohistochemical study of the extracellular matrix in non-small cell lung cancer: relation to lymph node metastasis and prognosis. Hokkaido Igaku Zasshi. 66, 356–368 (1991)
W.E. Mesker, J.M.C. Junggeburt, K. Szuhai, P. de Heer, H. Morreau, H.J. Tanke, R.A. Tollenaar, The carcinoma-stromal ratio of colon carcinoma is an independent factor for survival compared to lymph node status and tumor stage. Cell. Oncol. 29, 387–398 (2007)
A.M. Maeshima, T. Niki, A. Maeshima, T. Yamada, H. Kondo, Y. Matsuno, Modified scar grade: a prognostic indicator in small peripheral lung adenocarcinoma. Cancer. 95, 2546–2554 (2002)
E.F.W. Courrech Staal, M.W.J.M. Wouters, J.W. van Sandick, M.M. Takkenberg, V.T.H.B.M. Smit, J.M.C. Junggeburt, J.M.J. Spitzer-Naaykens, T. Karsten, H.H. Hartgrink, W.E. Mesker, R.A. Tollenaar, The stromal part of adenocarcinomas of the oesophagus: does it conceal targets for therapy? Eur. J. Cancer 46, 720–728 (2010)
N. Yanagisawa, R. Li, D. Rowley, H. Liu, D. Kadmon, B.J. Miles, T.M. Wheeler, G.E. Ayala, Stromogenic prostatic carcinoma pattern (carcinomas with reactive stromal grade 3) in needle biopsies predicts biochemical recurrence-free survival in patients after radical prostatectomy. Human pathology. 39, 282–291 (2008)
G. Ayala, J.A. Tuxhorn, T.M. Wheeler, A. Frolov, P.T. Scardino, M. Ohori, M. Wheeler, J. Spitler, D.R. Rowley, Reactive stroma as a predictor of biochemical-free recurrence in prostate cancer. Clin. Cancer Res. 9, 4792–4801 (2003)
F. Xing, J. Saidou, K. Watabe, Cancer associated fibroblasts (CAFs) in tumor microenvironment. Front. Biosci. 15, 166–179 (2010)
O. De Wever, P. Demetter, M. Mareel, M. Bracke, Stromal myofibroblasts are drivers of invasive cancer growth. Int. J. Cancer. 123, 2229–2238 (2008)
K. Pietras, A. Ostman, Hallmarks of cancer: interactions with the tumor stroma. Exp. Cell Res. 316, 1324–1331 (2010)
O.E. Franco, A.K. Shaw, D.W. Strand, S.W. Hayward, Cancer associated fibroblasts in cancer pathogenesis. Semin. Cell Dev. Biol. 21, 33–39 (2010)
K. Räsänen, A. Vaheri, Activation of fibroblasts in cancer stroma. Exp. Cell Res. 316, 2713–2722 (2010)
T. Hasebe, S. Sasaki, S. Imoto, A. Ochiai, Highly proliferative fibroblasts forming fibrotic focus govern metastasis of invasive ductal carcinoma of the breast. Mod. Pathol. 14(325–37) (2001)
T. Hasebe, H. Tsuda, S. Hirohashi, Y. Shimosato, Y. Tsubono, H. Yamamoto, K. Mukai, Fibrotic focus in infiltrating ductal carcinoma of the breast: a significant histopathological prognostic parameter for predicting the long-term survival of the patients. Breast Cancer Res. Treat. 49(195–208) (1998)
T. Hasebe, S. Sasaki, S. Imoto, K. Mukai, T. Yokose, A. Ochiai, Prognostic significance of fibrotic focus in invasive ductal carcinoma of the breast: a prospective observational study. Mod. Pathol. 15(502–16) (2002)
J.P.A. Baak, C.G.A. Colpaert, P.J. van Diest, E. Janssen, B. van Diermen, E. Albernaz, P.B. Vermeulen, E.A. Van Marck, Multivariate prognostic evaluation of the mitotic activity index and fibrotic focus in node-negative invasive breast cancers. Eur. J. Cancer. 41, 2093–2101 (2005)
C. Colpaert, P. Vermeulen, P. van Beest, G. Goovaerts, J. Weyler, P. Van Dam, L. Dirix, E. Van Marck, Intratumoral hypoxia resulting in the presence of a fibrotic focus is an independent predictor of early distant relapse in lymph node-negative breast cancer patients. Histopathology. 39, 416–425 (2001)
T. Hasebe, S. Sasaki, S. Imoto, A. Ochiai, Proliferative activity of intratumoral fibroblasts is closely correlated with lymph node and distant organ metastases of invasive ductal carcinoma of the breast. Am. J. Pathol. 156(1701–10) (2000)
C. Wenger, V. Ellenrieder, B. Alber, U. Lacher, A. Menke, H. Hameister, M. Wilda, T. Iwamura, H.G. Beger, G. Adler, T.M. Gress, Expression and differential regulation of connective tissue growth factor in pancreatic cancer cells. Oncogene. 18, 1073–1080 (1999)
L.F. Lau, S.C. Lam, The CCN family of angiogenic regulators: the integrin connection. Exp. Cell Res. 248, 44–57 (1999)
F. Yang, J.A. Tuxhorn, S.J. Ressler, S.J. McAlhany, T.D. Dang, D.R. Rowley, Stromal expression of connective tissue growth factor promotes angiogenesis and prostate cancer tumorigenesis. Cancer Res. 65, 8887–8895 (2005)
K.S. Frazier, G.R. Grotendorst, Expression of connective tissue growth factor mRNA in the fibrous stroma of mammary tumors. Int J Biochem Cell Biol. 29, 153–161 (1997)
A. Koliopanos, Helmut Friess, F.F. di Mola, W.-H. Tang, D. Kubulus, D. Brigstock, A. Zimmermann, M.W. Büchler, Connective tissue growth factor gene expression alters tumor progression in esophageal cancer. World J Surg. 26, 420–427 (2002)
A.B. Kasaragod, M.S. Lucia, G. Cabirac, G.R. Grotendorst, K.R. Stenmark, Connective tissue growth factor expression in pediatric myofibroblastic tumors. Pediatr. Dev. Pathol. 4, 37–45
T. Shakunaga, T. Ozaki, N. Ohara, K. Asaumi, T. Doi, K. Nishida, A. Kawai, T. Nakanishi, M. Takigawa, H. Inoue, Expression of connective tissue growth factor in cartilaginous tumors. Cancer. 89, 1466–1473 (2000)
M.-Y. Wang, P.-S. Chen, E. Prakash, H.-C. Hsu, H.-Y. Huang, M.-T. Lin, K.-J. Chang, M.-L. Kuo, Connective tissue growth factor confers drug resistance in breast cancer through concomitant up-regulation of Bcl-xL and cIAP1. Cancer Res. 69, 3482–3491 (2009)
M.P. Alfaro, D.L. Deskins, M. Wallus, J. Dasgupta, J.M. Davidson, L.B. Nanney, M. A Guney, M. Gannon, P.P. Young, A physiological role for connective tissue growth factor in early wound healing. Lab. Invest. [Epub ahead of print] (2012).
J. Taylor-Papadimitriou, J. Burchell, J. Hurst, Production of fibronectin by normal and malignant human mammary epithelial cells. Cancer Res. 41, 2491–2500 (1981)
C.-W. Pan, Z.-J. Shen, T.-T. Wu, X.-Y. Tang, M. Wang, J. Sun, Y. Shao, Cell adhesion to fibronectin induces mitomycin C resistance in bladder cancer cells. BJU international. 104, 1774–1779 (2009)
F. Thomas, J.M.P. Holly, R. Persad, A. Bahl, C.M. Perks, Fibronectin confers survival against chemotherapeutic agents but not against radiotherapy in DU145 prostate cancer cells: involvement of the insulin like growth factor-1 receptor. Prostate. 70, 856–865 (2010)
P.S. Hodkinson, T. Elliott, W.S. Wong, R.C. Rintoul, A.C. Mackinnon, C. Haslett, T. Sethi, ECM overrides DNA damage-induced cell cycle arrest and apoptosis in small-cell lung cancer cells through beta1 integrin-dependent activation of PI3-kinase. Cell Death Differ. 13, 1776–1788 (2006)
H. Miyamoto, T. Murakami, K. Tsuchida, H. Sugino, H. Miyake, S. Tashiro, Tumor-stroma interaction of human pancreatic cancer: acquired resistance to anticancer drugs and proliferation regulation is dependent on extracellular matrix proteins. Pancreas. 28, 38–44 (2004)
W.S. Argraves, L.M. Greene, M.A. Cooley, W.M. Gallagher, Fibulins: physiological and disease perspectives. EMBO reports. 4, 1127–1131 (2003)
A.J. Obaya, S. Rua, A. Moncada-Pazos, S. Cal, The dual role of fibulins in tumorigenesis. Cancer letters. 325, 132–138 (2012)
S.M. Pupa, S. Giuffré, F. Castiglioni, L. Bertola, M. Cantú, I. Bongarzone, P. Baldassari, R. Mortarini, W.S. Argraves, A. Anichini, S. Menard, E. Tagliabue, Regulation of breast cancer response to chemotherapy by fibulin-1. Cancer Res. 67, 4271–4277 (2007)
A. Sadr-Nabavi, J. Ramser, J. Volkmann, J. Naehrig, F. Wiesmann, B. Betz, H. Hellebrand, S. Engert, S. Seitz, R. Kreutzfeld, T. Sasaki, N. Arnold, R. Schmutzler, M. Kiechle, D. Niederacher, N. Harbeck, E. Dahl, A. Meindl, Decreased expression of angiogenesis antagonist EFEMP1 in sporadic breast cancer is caused by aberrant promoter methylation and points to an impact of EFEMP1 as molecular biomarker. Int. J. Cancer. 124, 1727–1735 (2009)
E.F. Roark, D.R. Keene, C.C. Haudenschild, S. Godyna, C.D. Little, W S Argraves, The association of human fibulin-1 with elastic fibers: an immunohistological, ultrastructural, and RNA study. J. Histochem. Cytochem. 43, 401–411 (1995)
A.R. Albig, J.R. Neil, W.P. Schiemann, Fibulins 3 and 5 antagonize tumor angiogenesis in vivo. Cancer Res. 66, 2621–2629 (2006)
R.K. Sironen, M. Tammi, R. Tammi, P.K. Auvinen, M. Anttila, V.-M. Kosma, Hyaluronan in human malignancies. Exp. Cell Res. 317, 383–391 (2011)
R.H. Tammi, A. Kultti, Veli-Matti Kosma, R. Pirinen, P. Auvinen, M.I. Tammi, Hyaluronan in human tumors: pathobiological and prognostic messages from cell-associated and stromal hyaluronan. Semin. Cancer Biol. 18, 288–295 (2008)
P. Gibbs, P.R. Clingan, V. Ganju, A.H. Strickland, S.S. Wong, N.C. Tebbutt, C.R. Underhill, R.M. Fox, S.P. Clavant, J. Leung, M. Pho, T.J. Brown, Hyaluronan-Irinotecan improves progression-free survival in 5-fluorouracil refractory patients with metastatic colorectal cancer: a randomized phase II trial. Cancer Chemother. Pharmacol. 67, 153–163 (2011)
Y. Xie, K.L. Aillon, S. Cai, J.M. Christian, N.M. Davies, C.J. Berkland, M.L. Forrest, Pulmonary delivery of cisplatin-hyaluronan conjugates via endotracheal instillation for the treatment of lung cancer. Int J Pharm. 392, 156–163 (2010)
S. Misra, S. Ghatak, B.P. Toole, Regulation of MDR1 expression and drug resistance by a positive feedback loop involving hyaluronan, phosphoinositide 3-kinase, and ErbB2. J. Biol. Chem. 280, 20310–20315 (2005)
P. Auvinen, R. Tammi, J. Parkkinen, M. Tammi, U. Agren, R. Johansson, P. Hirvikoski, M. Eskelinen, V.M. Kosma, Hyaluronan in peritumoral stroma and malignant cells associates with breast cancer spreading and predicts survival. Am. J. Pathol. 156(529–36) (2000)
R. Pirinen, R. Tammi, M. Tammi, P. Hirvikoski, J.J. Parkkinen, R. Johansson, J. Böhm, S. Hollmén, V.M. Kosma, Prognostic value of hyaluronan expression in non-small-cell lung cancer: Increased stromal expression indicates unfavorable outcome in patients with adenocarcinoma. Int. J. Cancer. 95(12–7) (2001)
K. Matsumoto, K. Date, H. Ohmichi, T. Nakamura, Hepatocyte growth factor in lung morphogenesis and tumor invasion: role as a mediator in epithelium-mesenchyme and tumor-stroma interactions. Cancer Chemother. Pharmacol. 38(Suppl), S42–S47 (1996)
J. Yamashita, M. Ogawa, S. Yamashita, K. Nomura, M. Kuramoto, T. Saishoji, Immunoreactive hepatocyte growth factor is a strong and independent predictor of recurrence and survival in human breast cancer. Cancer. 54, 1630–1633 (1994)
Q. Zeng, S. Chen, Z. You, Y. Fan, T.E. Carey, D. Saims, C.-Y. Wang, Hepatocyte growth factor inhibits anoikis in head and neck squamous cell carcinoma cells by activation of ERK and Akt signaling independent of NFkappa. B. J. Biol. Chem 277, 25203–25208 (2002)
S. Fan, J.A. Wang, R.Q. Yuan, S. Rockwell, J. Andres, A. Zlatapolskiy, I.D. Goldberg, E.M. Rosen, Scatter factor protects epithelial and carcinoma cells against apoptosis induced by DNA-damaging agents. Oncogene. 17, 131–141 (1998)
M. Mildner, L. Eckhart, B. Lengauer, E. Tschachler, Hepatocyte growth factor/scatter factor inhibits UVB-induced apoptosis of human keratinocytes but not of keratinocyte-derived cell lines via the phosphatidylinositol 3-kinase/AKT pathway. J. Biol. Chem. 277, 14146–14152 (2002)
A. Rasola, Hepatocyte growth factor sensitizes human ovarian carcinoma cell lines to paclitaxel and cisplatin. Cancer Res. 64, 1744–1750 (2004)
L.A. Shuman Moss, S. Jensen-Taubman, W.G. Stetler-Stevenson, Matrix metalloproteinases: changing roles in tumor progression and metastasis. Am. J. Pathol. 181, 1895–1899 (2012)
R. Poulsom, M. Pignatelli, W.G. Stetler-Stevenson, L.A. Liotta, P.A. Wright, R.E. Jeffery, J.M. Longcroft, L. Rogers, G.W. Stamp, Stromal expression of 72 kda type IV collagenase (MMP-2) and TIMP-2 mRNAs in colorectal neoplasia. Am. J. Pathol. 141(389–96) (1992)
C. Pyke, E. Ralfkiaer, K. Tryggvason, K. Danø, Messenger RNA for two type IV collagenases is located in stromal cells in human colon cancer. Am. J. Pathol. 142, 359–365 (1993)
H. Liu, T. Zhang, X. Li, J. Huang, B. Wu, X. Huang, Y. Zhou, J. Zhu, J. Hou, Predictive value of MMP-7 expression for response to chemotherapy and survival in patients with non-small cell lung cancer. Cancer Sci. 99(2185–92) (2008)
G.I. Murray, M.E. Duncan, P. O’Neil, J.A. McKay, W.T. Melvin, J.E. Fothergill, Matrix metalloproteinase-1 is associated with poor prognosis in oesophageal cancer. J. Pathol. 185, 256–261 (1998)
B. Fingleton, T. Vargo-Gogola, H.C. Crawford, L.M. Matrisian, Matrilysin [MMP-7] expression selects for cells with reduced sensitivity to apoptosis. Neoplasia. 3, 459–68
N. Mitsiades, W.H. Yu, V. Poulaki, M. Tsokos, I. Stamenkovic, Matrix metalloproteinase-7-mediated cleavage of Fas ligand protects tumor cells from chemotherapeutic drug cytotoxicity. Cancer Res. 61, 577–581 (2001)
V. Almendro, E. Ametller, S. García-Recio, O. Collazo, I. Casas, J.M. Augé, J. Maurel, P. Gascón, The role of MMP7 and its cross-talk with the FAS/FASL system during the acquisition of chemoresistance to oxaliplatin. PloS ONE. 4, e4728 (2009)
M. Egeblad, Z. Werb, New functions for the matrix metalloproteinases in cancer progression. Nature reviews. Nature reviews. Cancer. 2, 161–174 (2002)
Y. Jiang, I.D. Goldberg, Y.E. Shi, Complex roles of tissue inhibitors of metalloproteinases in cancer. Oncogene 21, 2245–2252 (2002)
M.N. Holten-Andersen, U. Hansen, N. Brünner, H.J. Nielsen, M. Illemann, B.S. Nielsen, Localization of tissue inhibitor of metalloproteinases 1 (TIMP-1) in human colorectal adenoma and adenocarcinoma. Int. J. Cancer. 113, 198–206 (2005)
A.-S. Schrohl, M.E. Meijer-van Gelder, M.N. Holten-Andersen, I.J. Christensen, M.P. Look, H.T. Mouridsen, N. Brünner, J.A. Foekens, Primary tumor levels of tissue inhibitor of metalloproteinases-1 are predictive of resistance to chemotherapy in patients with metastatic breast cancer. Clin. Cancer Res. 12, 7054–7058 (2006)
G.L. Willemoe, P.B. Hertel, A. Bartels, M.-B. Jensen, E. Balslev, B.B. Rasmussen, H. Mouridsen, B. Ejlertsen, N. Brünner, Lack of TIMP-1 tumour cell immunoreactivity predicts effect of adjuvant anthracycline-based chemotherapy in patients (n=647) with primary breast cancer. A Danish Breast Cancer Cooperative Group Study. Eur. J. Cancer. 45, 2528–2536 (2009)
N.M. Sørensen, P. Byström, I.J. Christensen, A. Berglund, H.J. Nielsen, N. Brünner, B. Glimelius, TIMP-1 is significantly associated with objective response and survival in metastatic colorectal cancer patients receiving combination of irinotecan, 5-fluorouracil, and folinic acid. Clin. Cancer Res 13, 4117–4122 (2007)
K.D. Steffensen, M. Waldstrøm, R.K. Christensen, A. Bartels, N. Brünner, A. Jakobsen, Lack of relationship between TIMP-1 tumour cell immunoreactivity, treatment efficacy and prognosis in patients with advanced epithelial ovarian cancer. BMC cancer. 10, 185 (2010)
A.D. Bradshaw, Diverse biological functions of the SPARC family of proteins. The international journal of biochemistry & cell biology. 44, 480–488 (2012)
I.T. Tai, M.J. Tang, SPARC in cancer biology: its role in cancer progression and potential for therapy. Drug resistance updates: reviews and commentaries in antimicrobial and anticancer chemotherapy. 11, 231–246 (2008)
M. Rahman, A.P.K. Chan, I.T. Tai, A peptide of SPARC interferes with the interaction between caspase8 and Bcl2 to resensitize chemoresistant tumors and enhance their regression in vivo. PloS ONE. 6, e26390 (2011)
M.J. Tang, I.T. Tai, A novel interaction between procaspase 8 and SPARC enhances apoptosis and potentiates chemotherapy sensitivity in colorectal cancers. J. Biol. Chem. 282, 34457–34467 (2007)
J.M. Chan, S.H. Ho, I.T. Tai, Secreted protein acidic and rich in cysteine-induced cellular senescence in colorectal cancers in response to irinotecan is mediated by P53. Carcinogenesis. 31, 812–819 (2010)
C. Atorrasagasti, M. Malvicini, J.B. Aquino, L. Alaniz, M. Garcia, M. Bolontrade, M. Rizzo, O.L. Podhajcer, G. Mazzolini, Overexpression of SPARC obliterates the in vivo tumorigenicity of human hepatocellular carcinoma cells. Int. J. Cancer. 126, 2726–2740 (2010)
I.T. Tai, M. Dai, D.A. Owen, L.B. Chen, Genome-wide expression analysis of therapy-resistant tumors reveals SPARC as a novel target for cancer therapy. J. Clin. Invest. 115, 1492–1502 (2005)
S.L. Bull Phelps, J. Carbon, A. Miller, E. Castro-Rivera, S. Arnold, R.A. Brekken, J.S. Lea, Secreted protein acidic and rich in cysteine as a regulator of murine ovarian cancer growth and chemosensitivity. Am. J. Obstet. Gynecol 200, 180.e1–7 (2009)
H.-C. Jeung, S.Y. Rha, C.K. Im, S.J. Shin, J.B. Ahn, W.I. Yang, J.K. Roh, S.H. Noh, H.C. Chung, A randomized phase 2 study of docetaxel and S-1 versus docetaxel and cisplatin in advanced gastric cancer with an evaluation of SPARC expression for personalized therapy. Cancer. 117, 2050–2057 (2011)
A. Francki, K. Motamed, T.D. McClure, M. Kaya, C. Murri, D.J. Blake, J.G. Carbon, E.H. Sage, SPARC regulates cell cycle progression in mesangial cells via its inhibition of IGF-dependent signaling. J. Cell. Biochem. 88, 802–811 (2003)
B.J. Schiemann, J.R. Neil, W.P. Schiemann, SPARC inhibits epithelial cell proliferation in part through stimulation of the transforming growth factor-beta-signaling system. Mol. Biol. Cell. 14, 3977–3988 (2003)
A. Francki, A.D. Bradshaw, J.A. Bassuk, C.C. Howe, W.G. Couser, E.H. Sage, SPARC regulates the expression of collagen type I and transforming growth factor-beta1 in mesangial cells. J. Cell. Biochem. 274(32145–52) (1999)
M. Bernfield, M. Götte, P.W. Park, O. Reizes, M.L. Fitzgerald, J. Lincecum, M. Zako, Functions of cell surface heparan sulfate proteoglycans. Annu. Rev. Biochem. 68, 729–777 (1999)
M. Götte, Syndecans in inflammation. FASEB J. 17, 575–591 (2003)
T. Maeda, C.M. Alexander, A. Friedl, Induction of syndecan-1 expression in stromal fibroblasts promotes proliferation of human breast cancer cells. Cancer Res. 64, 612–621 (2004)
B.J. Burbach, Y. Ji, A.C. Rapraeger, Syndecan-1 ectodomain regulates matrix-dependent signaling in human breast carcinoma cells. Exp. Cell Res. 300, 234–247 (2004)
M. Barbareschi, P. Maisonneuve, D. Aldovini, M.G. Cangi, L. Pecciarini, F. Angelo Mauri, S. Veronese, O. Caffo, A. Lucenti, P.D. Palma, E. Galligioni, C. Doglioni, High syndecan-1 expression in breast carcinoma is related to an aggressive phenotype and to poorer prognosis. Cancer. 98, 474–483 (2003)
C. Martin Götte, M. Kersting, J. Ruggiero, A.H. Tio, L. Tulusan, P. Kiesel, Wülfing, Predictive value of syndecan-1 expression for the response to neoadjuvant chemotherapy of primary breast cancer. Anticancer Res. 26, 621–627 (2006)
E. Tsanou, E. Ioachim, E. Briasoulis, A. Charchanti, K. Damala, V. Karavasilis, N. Pavlidis, N.J. Agnantis, Clinicopathological study of the expression of syndecan-1 in invasive breast carcinomas. correlation with extracellular matrix components. J. Exp. Clin. Cancer Res. 23, 641–650 (2004)
E.J. Kantelhardt, M. Vetter, M. Schmidt, C. Veyret, D. Augustin, V. Hanf, C. Meisner, D. Paepke, M. Schmitt, F. Sweep, G. von Minckwitz, P.-M. Martin, F. Jaenicke, C. Thomssen, N. Harbeck, Prospective evaluation of prognostic factors uPA/PAI-1 in node-negative breast cancer: phase III NNBC3-Europe trial (AGO, GBG, EORTC-PBG) comparing 6 × FEC versus 3 × FEC/3 × Docetaxel. BMC cancer. 11, 140 (2011)
E. Dublin, A. Hanby, N.K. Patel, R. Liebman, D. Barnes, Immunohistochemical expression of uPA, uPAR, and PAI-1 in breast carcinoma. Fibroblastic expression has strong associations with tumor pathology. Am. J. Pathol. 157, 1219–1227 (2000)
N. Harbeck, R.E. Kates, M. Schmitt, Clinical relevance of invasion factors urokinase-type plasminogen activator and plasminogen activator inhibitor type 1 for individualized therapy decisions in primary breast cancer is greatest when used in combination. J. Clin. Oncol. 20(1000–7) (2002)
N. Harbeck, R.E. Kates, M.P. Look, M. Kiechle, F. Ja, M. Schmitt, J.A. Foekens, Enhanced Benefit from Adjuvant Chemotherapy in Breast Cancer Patients Classified High-Risk according to Urokinase-type Plasminogen Activator (uPA) and Plasminogen Activator Inhibitor Type 1 (n = 3424. Cancer Res. 62(4617–22) (2002)
P. Manders, V.C.G. Tjan-Heijnen, P.N. Span, N. Grebenchtchikov, A.J. Geurts-Moespot, D.T.H. van Tienoven, L.V.A.M. Beex, F.C.G.J. Sweep, The complex between urokinase-type plasminogen activator (uPA) and its type-1 inhibitor (PAI-I) independently predicts response to first-line endocrine therapy in advanced breast cancer. Thromb. Haemost. 91, 514–521 (2004)
S. Borstnar, A. Sadikov, B. Mozina, T. Cufer, High levels of uPA and PAI-1 predict a good response to anthracyclines. Breast Cancer Res. Treat. 121, 615–624 (2010)
P. Manders, Predictive impact of urokinase-type plasminogen activator: plasminogen activator inhibitor type-1 complex on the efficacy of adjuvant systemic therapy in primary breast cancer. Cancer Res. 64, 659–664 (2004)
S. Ohno, M. Tachibana, T. Fujii, S. Ueda, H. Kubota, N. Nagasue, Role of stromal collagen in immunomodulation and prognosis of advanced gastric carcinoma. Int. J. Cancer. 97, 770–774 (2002)
N. Harbeck, R.E. Kates, M. Schmitt, K. Gauger, M. Kiechle, F. Jänicke, C. Thomssen, M.P. Look, J.A. Foekens, Urokinase-type plasminogen activator and its inhibitor type 1 predict disease outcome and therapy response in primary breast cancer. Clin. Breast Cancer 5, 348–352 (2004)
S. McAllister, A. Gifford, A. Greiner, S. Kelleher, M. Saelzler, T. Ince, F. Reinhardt, L. Harris, B. Hylander, E. Repasky, R. Weinberg, Systemic endocrine instigation of indolent tumor growth requires osteopontin. Cell. 133, 994–1005 (2008)
A.S. Schrohl, I.J. Christensen, A.N. Pedersen, V. Jensen, H. Mouridsen, G. Murphy, J.A. Foekens, N. Brunner, Mads Nikolaj Holten-Andersen, Tumor tissue concentrations of the proteinase inhibitors tissue inhibitor of metalloproteinases-1 (TIMP-1) and plasminogen activator inhibitor type 1 (PAI-1) are complementary in determining prognosis in primary breast cancer. Mol. Cell Proteomics. 2(164–72) (2003)
F. Jänicke, A. Prechtl, C. Thomssen, N. Harbeck, C. Meisner, M. Untch, C.G. Sweep, H.K. Selbmann, H. Graeff, M. Schmitt, Randomized adjuvant chemotherapy trial in high-risk, lymph node-negative breast cancer patients identified by urokinase-type plasminogen activator and plasminogen activator inhibitor type 1. J. Natl. Cancer Inst. 93(913–20) (2001)
C. Chuaysri, P. Thuwajit, A. Paupairoj, S. Chau-In, T. Suthiphongchai, C. Thuwajit, Alpha-smooth muscle actin-positive fibroblasts promote biliary cell proliferation and correlate with poor survival in cholangiocarcinoma. Oncol. Rep. 21, 957–969 (2009)
T. Tsujino, I. Seshimo, Hirofumi Yamamoto, C.Y. Ngan, K. Ezumi, I. Takemasa, M. Ikeda, M. Sekimoto, N. Matsuura, M. Monden, Stromal myofibroblasts predict disease recurrence for colorectal cancer. Clin. Cancer Res. 13, 2082–2090 (2007)
M. Erkan, C.W. Michalski, S. Rieder, C. Reiser-Erkan, I. Abiatari, A. Kolb, N.A. Giese, I. Esposito, H. Friess, J. Kleeff, The activated stroma index is a novel and independent prognostic marker in pancreatic ductal adenocarcinoma. Clin. Gastroenterol. Hepatol. 6, 1155–1161 (2008)
H. Zhong, A.M. De Marzo, E. Laughner, M. Lim, D.A. Hilton, D. Zagzag, P. Buechler, W.B. Isaacs, G.L. Semenza, J.W. Simons, Overexpression of hypoxia-inducible factor 1 alpha in common human cancers and their metastases. Cancer Res. 59, 5830–5835 (1999)
D.M. Brizel, G.S. Sibley, L.R. Prosnitz, R.L. Scher, M.W. Dewhirst, Tumor hypoxia adversely affects the prognosis of carcinoma of the head and neck. Int. J. Radiat. Oncol. Biol. Phys. 38, 285–289 (1997)
K. Sundfør, H. Lyng, E.K. Rofstad, Tumour hypoxia and vascular density as predictors of metastasis in squamous cell carcinoma of the uterine cervix. Br. J. Cancer. 78, 822–827 (1998)
M. Bacac, P. Provero, N. Mayran, J.-C. Stehle, C. Fusco, I. Stamenkovic, A mouse stromal response to tumor invasion predicts prostate and breast cancer patient survival. PloS ONE. 1, e32 (2006)
K. Utispan, P. Thuwajit, Y. Abiko, K. Charngkaew, A. Paupairoj, S. Chau-in, C. Thuwajit, Gene expression profiling of cholangiocarcinoma-derived fibroblast reveals alterations related to tumor progression and indicates periostin as a poor prognostic marker. Mol. Cancer. 9, 13 (2010)
T. Yamanashi, Y. Nakanishi, G. Fujii, Y. Akishima-Fukasawa, Y. Moriya, Y. Kanai, M. Watanabe, S. Hirohashi, Podoplanin expression identified in stromal fibroblasts as a favorable prognostic marker in patients with colorectal carcinoma. Oncology. 77, 53–62 (2009)
M. Leivonen, J. Lundin, S. Nordling, K. von Boguslawski, C. Haglund, Prognostic value of syndecan-1 expression in breast cancer. Oncology. 67, 11–18 (2004)
J.R. Infante, H. Matsubayashi, N. Sato, J. Tonascia, A.P. Klein, T.A. Riall, C. Yeo, C. Iacobuzio-Donahue, M. Goggins, Peritumoral fibroblast SPARC expression and patient outcome with resectable pancreatic adenocarcinoma. J. Clin. Oncol. 25, 319–325 (2007)
A.H. Ree, V.A. Florenes, J.P. Berg, G.M. Maelandsmo, J.M. Nesland, O. Fodstad, High levels of messenger RNAs for tissue inhibitors of metalloproteinases (TIMP-1 and TIMP-2) in primary breast carcinomas are associated with development of distant metastases. Clin. Cancer Res. 3, 1623–1628 (1997)
K. McCarthy, T. Maguire, G. McGreal, E. McDermott, N. O’Higgins, M.J. Duffy, High levels of tissue inhibitor of metalloproteinase-1 predict poor outcome in patients with breast cancer. Int. J. Cancer. 84, 44–48 (1999)
M.P. Look, W.L.J. van Putten, M.J. Duffy, N. Harbeck, I.J. Christensen, C. Thomssen, R. Kates, F. Spyratos, M. Fernö, S. Eppenberger-Castori, C.G.J.F. Sweep, K. Ulm, J. Peyrat, P. Martin, H. Magdelenat, N. Brünner, C. Duggan, B.W. Lisboa, P. Bendahl, V. Quillien et al., Pooled analysis of prognostic impact of urokinase-type plasminogen activator and its inhibitor PAI-1 in 8377 breast cancer patients. J. Natl. Cancer Inst 94, 116–128 (2002)
P.A. Andreasen, L. Kjøller, L. Christensen, M.J. Duffy, The urokinase-type plasminogen activator system in cancer metastasis: a review. Int. J. Cancer. 72, 1–22 (1997)
M. Schmitt, N. Harbeck, C. Thomssen, O. Wilhelm, V. Magdolen, U. Reuning, K. Ulm, H. Höfler, F. Jänicke, H. Graeff, Clinical impact of the plasminogen activation system in tumor invasion and metastasis: prognostic relevance and target for therapy. Thromb. Haemost. 78(285–96) (1997)
M.J. Duffy, T.M. Maguire, E.W. McDermott, N. O’Higgins, Urokinase plasminogen activator: a prognostic marker in multiple types of cancer. J Surg Oncol. 71(130–5) (1999)
C.Y. Ngan, H. Yamamoto, I. Seshimo, T. Tsujino, M. Man-i, J.-I. Ikeda, K. Konishi, I. Takemasa, M. Ikeda, M. Sekimoto, N. Matsuura, M. Monden, Quantitative evaluation of vimentin expression in tumour stroma of colorectal cancer. Br. J. Cancer 96, 986–992 (2007)
S. Al-Saad, K. Al-Shibli, T. Donnem, M. Persson, R.M. Bremnes, L.-T. Busund, The prognostic impact of NF-kappaB p105, vimentin, E-cadherin and Par6 expression in epithelial and stromal compartment in non-small-cell lung cancer. Br. J. Cancer. 99, 1476–1483 (2008)
L.-K. Liu, X.-Y. Jiang, X.-X. Zhou, D.-M. Wang, X.-L. Song, H.-B. Jiang, Upregulation of vimentin and aberrant expression of E-cadherin/beta-catenin complex in oral squamous cell carcinomas: correlation with the clinicopathological features and patient outcome. Mod. Pathol. 23, 213–224 (2010)
S. Otsuki, M. Inokuchi, M. Enjoji, T. Ishikawa, Y. Takagi, K. Kato, H. Yamada, K. Kojima, K. Sugihara, Vimentin expression is associated with decreased survival in gastric cancer. Oncol. Rep. 25, 1235–1242 (2011)
T. Hasebe, H. Tsuda, Y. Tsubono, S. Imoto, K. Mukai, Fibrotic focus in invasive ductal carcinoma of the breast: a histopathological prognostic parameter for tumor recurrence and tumor death within three years after the initial operation. Jpn. J. Cancer Res. 88(590–9) (1997)
A. Neesse, P. Michl, K.K. Frese, C. Feig, N. Cook, M.A. Jacobetz, M.P. Lolkema, M. Buchholz, K.P. Olive, T.M. Gress, D.A. Tuveson, Stromal biology and therapy in pancreatic cancer. Gut 60, 861–868 (2011)
I.G. Schauer, A.K. Sood, S. Mok, Cancer-associated fibroblasts and their putative role in potentiating the initiation and development of epithelial ovarian cancer. Neoplasia. 13, 393–405 (2011)
H. Breuninger, G. Schaumburg-Lever, J. Holzschuh, H.P. Horny, Desmoplastic squamous cell carcinoma of skin and vermilion surface: a highly malignant subtype of skin cancer. Cancer. 79, 915–919 (1997)
L.A. Hazlehurst, W.S. Dalton, Mechanisms associated with cell adhesion mediated drug resistance (CAM-DR) in hematopoietic malignancies. Cancer Metastasis Rev. 20, 43–50 (2001)
H.F. Dvorak, Tumors: wounds that do not heal. Similarities between tumor stroma generation and wound healing. N. Engl. J. Med. 315, 1650–1659 (1986)
S. Grotegut, R. Kappler, S. Tarimoradi, F. Lehembre, Hepatocyte growth factor protects hepatoblastoma cells from chemotherapy-induced apoptosis by AKT activation. Int. J. Oncol. 36, 1261–1267 (2010)
Acknowledgements
This work was funded by the Jean Shanks Foundation.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hale, M.D., Hayden, J.D. & Grabsch, H.I. Tumour-microenvironment interactions: role of tumour stroma and proteins produced by cancer-associated fibroblasts in chemotherapy response. Cell Oncol. 36, 95–112 (2013). https://doi.org/10.1007/s13402-013-0127-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13402-013-0127-7