Abstract
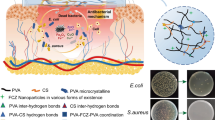
Recently, nanoclays have gained amount of attention as being the potential nanomaterials in the wound healing field. Due to having a high specific area, high adsorption of several therapeutic agents, good chemical inertness, and low cost, these nanomaterials are more interested in using. In this paper, we thoroughly introduced common types of nanoclays such as halloysite, kaolinite, montmorillonite, and bentonite. Interesting physical and chemical characteristics of these nanoclays are described. Further, the methods through which nanoclays are processed to form hydrogels are described. These included methods are not limited to in situ free radical polymerization, supramolecular assembly, freeze-thawing, and grafting. Finally, in this paper clay-based hydrogels and their unique properties such as antimicrobial properties and their application in wound healing are thoroughly discussed.



Modified from reference




Modified from reference


Similar content being viewed by others
References
Ruiz-Hitzky, E.; Darder, M.; Fernandes, F.M.; Wicklein, B.; Alcântara, A.C.; Aranda, P.: Fibrous clays based bionanocomposites. Prog. Polym. Sci. 38(10–11), 1392–1414 (2013)
Petrulyte, S.: Advanced textile materials and biopolymers in wound management. Dan. Med. Bull. 55(1), 72–77 (2008)
Davidson, J.R.: Current concepts in wound management and wound healing products. Vet. Clin.: Small Anim. Pract. 45(3), 537–564 (2015)
Cockbill SM, Turner TD. The development of wound management products. Krasner DL, Rodeheaver GT, Sibbald RG: Chronic wound care: a clinical source book for healthcare professionals 4th ed Malvern, PA: HMP Communications. 2007:233–48
Hadisi, Z.; Nourmohammadi, J.; Nassiri, S.M.: The antibacterial and anti-inflammatory investigation of Lawsonia Inermis-gelatin-starch nano-fibrous dressing in burn wound. Int. J. Biol. Macromol. 107, 2008–2019 (2018)
Mishra, R.; Ramasamy, K.; Lim, S.; Ismail, M.; Majeed, A.: Antimicrobial and in vitro wound healing properties of novel clay based bionanocomposite films. J. Mater. Sci. - Mater. Med. 25(8), 1925–1939 (2014)
Kalantari, K.; Mostafavi, E.; Saleh, B.; Soltantabar, P.; Webster, T.J.: Chitosan/PVA hydrogels incorporated with green synthesized cerium oxide nanoparticles for wound healing applications. Eur. Polymer J. 134, 109853 (2020)
Tottoli, E.M.; Dorati, R.; Genta, I.; Chiesa, E.; Pisani, S.; Conti, B.: Skin wound healing process and new emerging technologies for skin wound care and regeneration. Pharmaceutics 12(8), 735 (2020)
Moeini, A.; Pedram, P.; Makvandi, P.; Malinconico, M.; d’Ayala, G.G.: Wound healing and antimicrobial effect of active secondary metabolites in chitosan-based wound dressings: a review. Carbohyd. Polym. 233, 115839 (2020)
Ye, S.; Jiang, L.; Wu, J.; Su, C.; Huang, C.; Liu, X., et al.: Flexible amoxicillin-grafted bacterial cellulose sponges for wound dressing: in vitro and in vivo evaluation. ACS Appl. Mater. Interfaces 10(6), 5862–5870 (2018)
Hakkarainen, T.; Koivuniemi, R.; Kosonen, M.; Escobedo-Lucea, C.; Sanz-Garcia, A.; Vuola, J., et al.: Nanofibrillar cellulose wound dressing in skin graft donor site treatment. J. Control. Release 244, 292–301 (2016)
Rosińczuk J, Taradaj J, Dymarek R, Sopel M: Mechanoregulation of wound healing and skin homeostasis. Chronic Wounds, Wound Dressings and Wound Healing.S 2021:461–77
Kamoun, E.A.; Kenawy, E.-R.S.; Chen, X.: A review on polymeric hydrogel membranes for wound dressing applications: PVA-based hydrogel dressings. J. Adv. Res. 8(3), 217–233 (2017)
Mirhoseini, M.; Kianezhad, M.A.; Rezaeipour, B.; Ghasemi, M.; Rezanejad Gatabi, Z.; Nia, H.S., et al.: The synergistic effect of topical insulin and clindamycin on acute dermal wound healing in rat model: a histological study. J. Histotechnol. 244(2), 1–10 (2021)
Cañedo-Dorantes, L.; Cañedo-Ayala, M.: Skin acute wound healing: a comprehensive review. Int. J. Inflamm. (2019). https://doi.org/10.1155/2019/3706315
Suarato, G.; Bertorelli, R.; Athanassiou, A.: Borrowing from Nature: biopolymers and biocomposites as smart wound care materials. Front. Bioeng. Biotechnol. 6, 137 (2018)
Daunton C, Kothari S, Smith L, Steele D: A history of materials and practices for wound management. Wound Practice & Research: Journal of the Australian Wound Management Association. 2012;20(4)
Winter, G.D.: Formation of the scab and the rate of epithelization of superficial wounds in the skin of the young domestic pig. Nature 193(4812), 293–294 (1962)
Moura, L.I.; Dias, A.M.; Carvalho, E.; de Sousa, H.C.: Recent advances on the development of wound dressings for diabetic foot ulcer treatment—a review. Acta Biomater. 9(7), 7093–7114 (2013)
Madaghiele, M.; Demitri, C.; Sannino, A.; Ambrosio, L.: Polymeric hydrogels for burn wound care: Advanced skin wound dressings and regenerative templates. Burns & Trauma 2(4), 2321–3868 (2014)
Ahmed, E.M.: Hydrogel: preparation, characterization, and applications: a review. J. Adv. Res. 6(2), 105–121 (2015)
Sharma, S.; Jain, P.; Tiwari, S.: Dynamic imine bond based chitosan smart hydrogel with magnified mechanical strength for controlled drug delivery. Int. J. Biol. Macromol. 160, 489–495 (2020)
Karoyo, A.H.; Wilson, L.D.: A review on the design and hydration properties of natural polymer-based hydrogels. Materials. 14(5), 1095 (2021)
Mondal, S.; Das, S.; Nandi, A.K.: A review on recent advances in polymer and peptide hydrogels. Soft Matter 16(6), 1404–1454 (2020)
Xiang, J.; Shen, L.; Hong, Y.: Status and future scope of hydrogels in wound healing: synthesis, materials and evaluation. Eur. Polymer J. 130, 109609 (2020)
Zhang, Y.; An, R.; Han, L.; Wang, X.; Shi, L.; Ran, R.: Novel self-healing, shape-memory, tunable double-layer actuators based on semi-ipn and physical double-network hydrogels. Macromol. Mater. Eng. 303(12), 1800505 (2018)
Macdougall, L.J.; Pérez-Madrigal, M.M.; Shaw, J.E.; Inam, M.; Hoyland, J.A.; O’Reilly, R., et al.: Self-healing, stretchable and robust interpenetrating network hydrogels. Biomater. Sci. 6(11), 2932–2937 (2018)
Kumari, P.V.K.; Rao, Y.S.; Akhila, S.: Role of nanocomposites in drug delivery. GSC Biol. Pharm. Sci. 8(3), 94–103 (2019)
Sharma R, Raina K. Structural and Electrical studies on ferroelectric polymer nanocomposites 2011
Gaskell, E.E.; Hamilton, A.R.: Antimicrobial clay-based materials for wound care. Future Med. Chem. 6(6), 641–655 (2014)
Williams, L.B.; Metge, D.W.; Eberl, D.D.; Harvey, R.W.; Turner, A.G.; Prapaipong, P., et al.: What makes a natural clay antibacterial? Environ. Sci. Technol. 45(8), 3768–3773 (2011)
Beal GW, Cocke D. Process and composition of a gel for wound disinfection and promotion of healing. Google Patents (2014)
Ambrogi, V.; Pietrella, D.; Nocchetti, M.; Casagrande, S.; Moretti, V.; De Marco, S., et al.: Montmorillonite–chitosan–chlorhexidine composite films with antibiofilm activity and improved cytotoxicity for wound dressing. J. Colloid Interface Sci. 491, 265–272 (2017)
Barua, S.; Chattopadhyay, P.; Aidew, L.; Buragohain, A.K.; Karak, N.: Infection-resistant hyperbranched epoxy nanocomposite as a scaffold for skin tissue regeneration. Polym. Int. 64(2), 303–311 (2015)
Sandri, G.; Bonferoni, M.C.; Ferrari, F.; Rossi, S.; Aguzzi, C.; Mori, M., et al.: Montmorillonite–chitosan–silver sulfadiazine nanocomposites for topical treatment of chronic skin lesions: In vitro biocompatibility, antibacterial efficacy and gap closure cell motility properties. Carbohyd. Polym. 102, 970–977 (2014)
Shen, M.; Li, L.; Sun, Y.; Xu, J.; Guo, X.; Prud’homme, R.K.: Rheology and adhesion of poly (acrylic acid)/ laponite nanocomposite hydrogels as biocompatible adhesives. Langmuir 30(6), 1636–1642 (2014)
Kokabi, M.; Sirousazar, M.; Hassan, Z.M.: PVA–clay nanocomposite hydrogels for wound dressing. Eur. Polymer J. 43(3), 773–781 (2007)
Shanmugapriya, K.; Kim, H.; Saravana, P.S.; Chun, B.-S.; Kang, H.W.: Fabrication of multifunctional chitosan-based nanocomposite film with rapid healing and antibacterial effect for wound management. Int. J. Biol. Macromol. 118, 1713–1725 (2018)
Noori, S.; Kokabi, M.; Hassan, Z.: Poly (vinyl alcohol)/chitosan/honey/clay responsive nanocomposite hydrogel wound dressing. J. Appl. Polym. Sci. 135(21), 46311 (2018)
Sirousazar, M.; Jahani-Javanmardi, A.; Kheiri, F.; Hassan, Z.M.: In vitro and in vivo assays on egg white/polyvinyl alcohol/clay nanocomposite hydrogel wound dressings. J. Biomater. Sci. Polym. Ed. 27(16), 1569–1583 (2016)
Han, L.; Lu, X.; Liu, K.; Wang, K.; Fang, L.; Weng, L.-T., et al.: Mussel-inspired adhesive and tough hydrogel based on nanoclay confined dopamine polymerization. ACS Nano 11(3), 2561–2574 (2017)
Perioli, L.; Dorigato, A.; Pagano, C.; Leoni, M.; Pegoretti, A.: Thermo-mechanical and adhesive properties of polymeric films based on ZnAl-hydrotalcite composites for active wound dressings. Polym. Eng. Sci. 59(S1), E112–E119 (2019)
Zou, Q.; Cai, B.; Li, J.; Li, J.; Li, Y.: In vitro and in vivo evaluation of the chitosan/Tur composite film for wound healing applications. J. Biomater. Sci. Polym. Ed. 28(7), 601–615 (2017)
Wang, W Wang, A Nanoscale clay minerals for functional ecomaterials: fabrication, applications, and future trends. In: Handbook of Ecomaterials, pp. 1-82, Springer, (2019)
Massaro, M.; Colletti, C.G.; Lazzara, G.; Riela, S.: The use of some clay minerals as natural resources for drug carrier applications. J. Funct. Biomater. 9(4), 58 (2018)
Sposito, G.; Skipper, N.T.; Sutton, R.; Park, S.-h; Soper, A.K.; Greathouse, J.A.: Surface geochemistry of the clay minerals. Proc. Nat. Acad. Sci. 96(7), 3358–3364 (1999)
Schaef, H.T.; Loganathan, N.; Bowers, G.M.; Kirkpatrick, R.J.; Yazaydin, A.O.; Burton, S.D., et al.: Tipping point for expansion of layered aluminosilicates in weakly polar solvents: supercritical CO2. ACS Appl. Mater. Interfaces 9(42), 36783–36791 (2017)
Vaiana CA: Bio-Functionalized Clay Nanoparticles for Wound Healing Applications: Wright State University (2011)
Tamer, T.M.; Sabet, M.M.; Omer, A.M.; Abbas, E.; Eid, A.I.; Mohy-Eldin, M.S., et al.: Hemostatic and antibacterial PVA/Kaolin composite sponges loaded with penicillin–streptomycin for wound dressing applications. Sci. Rep. 11(1), 1–15 (2021)
Liu, M.; Shen, Y.; Ao, P.; Dai, L.; Liu, Z.; Zhou, C.: The improvement of hemostatic and wound healing property of chitosan by halloysite nanotubes. RSC Adv. 4(45), 23540–23553 (2014)
Haraguchi, K.: Nanocomposite hydrogels. Curr. Opin. Solid State Mater. Sci. 11(3–4), 47–54 (2007)
Pereira, A.G.; Rodrigues, F.H.; Paulino, A.T.; Martins, A.F.; Fajardo, A.R.: Recent advances on composite hydrogels designed for the remediation of dye-contaminated water and wastewater: a review. J. Clean. Prod. 284, 124 (2020)
Iliescu, R.I.; Andronescu, E.; Voicu, G.; Ficai, A.; Covaliu, C.I.: Hybrid materials based on montmorillonite and citostatic drugs: preparation and characterization. Appl. Clay Sci. 52(1–2), 62–68 (2011)
Suresh, R.; Borkar, S.; Sawant, V.; Shende, V.; Dimble, S.: Nanoclay drug delivery system. Int. J. Pharm. Sci. Nanotechnol. 3(2), 901–906 (2010)
Dabbaghianamiri M: Polymer/cay Nanocomposite Self-assembly for Gas Barrier Films Application: Texas State University (2017)
Ahmad, N.H.; Mohamed, M.A.; Yusoff, S.F.M.: Improved adsorption performance of rubber-based hydrogel: optimisation through response surface methodology, isotherm, and kinetic studies. J. Sol-Gel Sci. Technol. 94(2), 322–334 (2020)
Khan, S.A.; Khan, T.A.: Clay-hydrogel nanocomposites for adsorptive amputation of contaminants from aqueous phase: a review. J. Environ. Chem. Eng. 9, 105 (2021)
Gaharwar, A.K.; Kishore, V.; Rivera, C.; Bullock, W.; Wu, C.J.; Akkus, O., et al.: Physically crosslinked nanocomposites from silicate-crosslinked PEO: mechanical properties and osteogenic differentiation of human mesenchymal stem cells. Macromol. Biosci. 12(6), 779–793 (2012)
Zhao, L.Z.; Zhou, C.H.; Wang, J.; Tong, D.S.; Yu, W.H.; Wang, H.: Recent advances in clay mineral-containing nanocomposite hydrogels. Soft Matter 11(48), 9229–9246 (2015)
Tavakoli, J.; Gascooke, J.; Xie, N.; Tang, B.Z.; Tang, Y.: Enlightening freeze–thaw process of physically cross-linked poly (vinyl alcohol) hydrogels by aggregation-induced emission fluorogens. ACS Appl. Polym. Mater. 1(6), 1390–1398 (2019)
Ibrahim, S.M.; El-Naggar, A.A.: Preparation of poly (vinyl alcohol)/clay hydrogel through freezing and thawing followed by electron beam irradiation for the treatment of wastewater. J. Thermoplast. Compos. Mater. 26(10), 1332–1348 (2013)
Wang, Y.; Qi, Y.; Chen, C.; Zhao, C.; Ma, Y.; Yang, W.: Layered Co-Immobilization of β-Glucosidase and Cellulase on Polymer Film by Visible-Light-Induced Graft Polymerization. ACS Appl. Mater. Interfaces. 11(47), 44913–44921 (2019)
Li, B.; Zhang, Y.; Wu, C.; Guo, B.; Luo, Z.: Fabrication of mechanically tough and self-recoverable nanocomposite hydrogels from polyacrylamide grafted cellulose nanocrystal and poly (acrylic acid). Carbohyd. Polym. 198, 1–8 (2018)
Sharma, G.; Thakur, B.; Naushad, M.; Kumar, A.; Stadler, F.J.; Alfadul, S.M., et al.: Applications of nanocomposite hydrogels for biomedical engineering and environmental protection. Environ. Chem. Lett. 16(1), 113–146 (2018)
Ninan, N.; Muthiah, M.; Park, I.-K.; Wong, T.W.; Thomas, S.; Grohens, Y.: Natural polymer/inorganic material based hybrid scaffolds for skin wound healing. Polym. Rev. 55(3), 453–490 (2015)
Kim, Y.S.; Liu, M.; Ishida, Y.; Ebina, Y.; Osada, M.; Sasaki, T., et al.: Thermoresponsive actuation enabled by permittivity switching in an electrostatically anisotropic hydrogel. Nat. Mater. 14(10), 1002–1007 (2015)
Sandri G Bonferoni M Rossi S Ferrari F Aguzzi C Viseras C et al: Clay minerals for tissue regeneration, repair, and engineering. Wound Healing Biomaterials, pp. 385-402, Elsevier, (2016)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rezanejad Gatabi, Z., Heshmati, N., Mirhoseini, M. et al. The Application of Clay-Based Nanocomposite Hydrogels in Wound Healing. Arab J Sci Eng 48, 8481–8494 (2023). https://doi.org/10.1007/s13369-022-06959-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13369-022-06959-3