Abstract
Human immunodeficiency virus (HIV) mainly attacks lymphocytes of the human immune system. The untreated infection leads to acquired immune deficiency syndrome (AIDS). Ritonavir (RTV) belongs to protease inhibitors (PIs), the crucial contributors of the combination therapy used in the treatment of HIV that is called highly active antiretroviral therapy (HAART). Formulations targeting the lymphatic system (LS) play a key role in delivering and maintaining therapeutic drug concentrations in HIV reservoirs. In our previous study, we developed RTV-loaded nanostructured lipid carriers (NLCs), which contain the natural antioxidant alpha-tocopherol (AT). In the current study, the cytotoxicity of the formulation was studied in HepG2, MEK293, and H9C2 cell lines. The formulation efficacy to reach the LS was evaluated through a cycloheximide-injected chylomicron flow blockade model in Wistar rats. Biodistribution and toxicity studies were conducted in rodents to understand drug distribution patterns in various organs and to establish the safety profile of the optimized formulation (RTV-NLCs). From the MTT assay, it was found that the cell viability of the formulation is comparable with the pure drug (RTV-API). More than 2.5-folds difference in AUC was observed in animals treated with RTV-NLCs with and without cycloheximide injection. Biodistribution studies revealed higher drug exposure in the lymphoidal organs with the RTV-NLCs. No significant increase in serum biomarkers for hepatotoxicity was observed in rats dosed with the RTV-NLCs. The current study reveals the lymphatic uptake of the RTV-NLCs and their safety in rodents. As the tissue distribution of RTV-NLCs is high, hence re-adjusting the RTV-NLCs dose to get the response equivalent to RTV-API may be more beneficial with respect to its safety and efficacy.
Graphical Abstract








Similar content being viewed by others
Data availability
All the datasets supporting the findings of this research are available from the author's upon reasonable request.
References
Moyle GJ, Gazzard BG, Cooper DA, Gatell J. Antiretroviral therapy for HIV infection. A knowledge-based approach to drug selection and use. Drugs. 1998;55(3):383–404. https://doi.org/10.2165/00003495-199855030-00005.
Xu H, Krakow S, Shi Y, Rosenberg J, Gao P. In vitro characterization of ritonavir formulations and correlation to in vivo performance in dogs. Eur J Pharm Sci. 2018;115:286–95. https://doi.org/10.1016/j.ejps.2018.01.026.
Mehta C, Narayan R, Aithal G, Pandiyan S, Bhat P, Dengale S, et al. Molecular simulation driven experiment for formulation of fixed dose combination of Darunavir and Ritonavir as anti-HIV nanosuspension. J Mol Liq. 2019;293:111469. https://doi.org/10.1016/j.molliq.2019.111469.
De Espíndola B, Beringhs AO, Sonaglio D, Stulzer HK, Silva MAS, Ferraz HG, et al. Liquisolid pellets: a pharmaceutical technology strategy to improve the dissolution rate of Ritonavir. Saudi Pharm J. 2019;27(5):702–12. https://doi.org/10.1016/j.jsps.2019.04.005.
Kumar S, Narayan R, Ahammed V, Nayak Y, Naha A, Nayak UY. Development of ritonavir solid lipid nanoparticles by Box Behnken design for intestinal lymphatic targeting. J Drug Delivery Sci Technol. 2018;44:181–9. https://doi.org/10.1016/j.jddst.2017.12.014.
EMA. Norvir [Internet]. Eur Med Agency. 2018 [cited 2023 Jul 2]. Available from: https://www.ema.europa.eu/en/medicines/human/EPAR/norvir.
Reyskens KMSE, Fisher T-L, Schisler JC, O'Connor WG, Rogers AB, Willis MS, et al. Cardio-metabolic effects of HIV Protease inhibitors (Lopinavir/Ritonavir). PLoS ONE. 2013;8(9):e73347. https://doi.org/10.1371/journal.pone.0073347.
Sulkowski MS. Hepatotoxicity associated with antiretroviral therapy in adults infected with human immunodeficiency virus and the role of hepatitis C or B virus infection. JAMA. 2000;283(1):74. https://doi.org/10.1001/jama.283.1.74.
Kuang C-C, Wang Y, Hu P-C, Gao F-F, Bu L, Wen X-M, et al. Ritonavir-induced hepatotoxicity and ultrastructural changes of hepatocytes. Ultrastruct Pathol. 2014;38(5):329–34. https://doi.org/10.3109/01913123.2014.914114.
Périard D, Telenti A, Sudre P, Cheseaux JJ, Halfon P, Reymond MJ, et al. Atherogenic dyslipidemia in HIV-infected individuals treated with protease inhibitors. The Swiss HIV Cohort Study Circulation. 1999;100(7):700–5. https://doi.org/10.1161/01.cir.100.7.700.
Purnell JQ, Zambon A, Knopp RH, Pizzuti DJ, Achari R, Leonard JM, et al. Effect of Ritonavir on lipids and post-heparin lipase activities in normal subjects. AIDS. 2000;14(1):51–7. https://doi.org/10.1097/00002030-200001070-00006.
Sulkowski MS. Drug-induced liver injury associated with antiretroviral therapy that includes HIV-1 protease inhibitors. Clin Infect Dis. 2004;38(Suppl 2):S90-97. https://doi.org/10.1086/381444.
Managuli RS, Raut SY, Reddy MS, Mutalik S. Targeting the intestinal lymphatic system: a versatile path for enhanced oral bioavailability of drugs. Expert Opin Drug Delivery. 2018;15(8):787–804. https://doi.org/10.1080/17425247.2018.1503249.
Darwis Y, Ali Khan A, Mudassir J, Mohtar N. Advanced drug delivery to the lymphatic system: lipid-based nanoformulations. IJN. 2013;2733. https://doi.org/10.2147/IJN.S41521.
Cohen OJ, Pantaleo G, Lam GK, Fauci AS. Studies on lymphoid tissue from HIV-infected individuals: implications for the design of therapeutic strategies. Springer Semin Immunopathol. 1997;18(3):305–22. https://doi.org/10.1007/BF00813500.
Singh I, Swami R, Khan W, Sistla R. Delivery systems for lymphatic targeting. Focal Contr Drug Del. 2014;429–58. https://doi.org/10.1007/978-1-4614-9434-8_20.
Désormeaux A, Bergeron MG. Lymphoid tissue targeting of anti-HIV drugs using liposomes. Methods Enzymol. 2005;391:330–51. https://doi.org/10.1016/S0076-6879(05)91019-7.
Mishra A, Vuddanda PR, Singh S. Intestinal lymphatic delivery of Praziquantel by solid lipid nanoparticles: formulation design, in vitro and in vivo studies. J Nanotechnol. 2014;2014:1–12. https://doi.org/10.1155/2014/351693.
Humberstone AJ, Charman WN. Lipid-based vehicles for the oral delivery of poorly water soluble drugs. Adv Drug Deliv Rev. 1997;25(1):103–28. https://doi.org/10.1016/S0169-409X(96)00494-2.
Gurumukhi VC, Bari SB. Quality by design (QbD)–based fabrication of atazanavir-loaded nanostructured lipid carriers for lymph targeting: bioavailability enhancement using chylomicron flow block model and toxicity studies. Drug Deliv and Transl Res. 2022;12(5):1230–52. https://doi.org/10.1007/s13346-021-01014-4.
Patel P, Patel M. Enhanced oral bioavailability of nintedanib esylate with nanostructured lipid carriers by lymphatic targeting: In vitro, cell line and in vivo evaluation. Eur J Pharm Sci. 2021;159:105715. https://doi.org/10.1016/j.ejps.2021.105715.
Gurumukhi VC, Bari SB. Development of ritonavir-loaded nanostructured lipid carriers employing quality by design (QbD) as a tool: characterizations, permeability, and bioavailability studies. Drug Deliv Transl Res. 2021. https://doi.org/10.1007/s13346-021-01083-5.
Walimbe CA, More SS, Walawalkar RU, Shah RR, Ghodke D. Optimisation of nanostructured lipid carriers of ritonavir. Inventi Rapid: NDDS. 2012;2012(4):1–8.
Javan F, Vatanara A, Azadmanesh K, Nabi-Meibodi M, Shakouri M. Encapsulation of Ritonavir in solid lipid nanoparticles: in-vitro anti-HIV-1 activity using lentiviral particles. J Pharm Pharmacol. 2017;69(8):1002–9. https://doi.org/10.1111/jphp.12737.
Ahammed V, Narayan R, Paul J, Nayak Y, Roy B, Shavi GV, et al. Development and in vivo evaluation of functionalized ritonavir proliposomes for lymphatic targeting. Life Sci. 2017;183:11–20. https://doi.org/10.1016/j.lfs.2017.06.022.
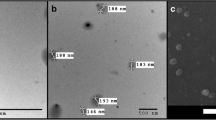
Jitta SR, Bhaskaran NA, Salwa, Kumar L. Anti-oxidant containing nanostructured lipid carriers of Ritonavir: development, optimization, and in vitro and in vivo evaluations. AAPS PharmSciTech. 2022;23(4):88. https://doi.org/10.1208/s12249-022-02240-w.
Shrivastava S, Gidwani B, Kaur CD. Development of mebendazole loaded nanostructured lipid carriers for lymphatic targeting: optimization, characterization, in-vitro and in-vivo evaluation. Parti Sci Technol. 2021;39(3):380–90. https://doi.org/10.1080/02726351.2020.1750515.
Bhalekar MR, Upadhaya PG, Madgulkar AR, Kshirsagar SJ, Dube A, Bartakke US. In-vivo bioavailability and lymphatic uptake evaluation of lipid nanoparticulates of Darunavir. Drug Delivery. 2016;23(7):2581–6. https://doi.org/10.3109/10717544.2015.1037969.
Shafran SD, Mashinter LD, Roberts SE. The effect of low-dose ritonavir monotherapy on fasting serum lipid concentrations. HIV Med. 2005;6(6):421–5. https://doi.org/10.1111/j.1468-1293.2005.00328.x.
Onabajo OO, Lewis MG, Mattapallil JJ. GALT CD4+PD-1hi T follicular helper (Tfh) cells repopulate after antiretroviral therapy. Cell Immunolo. 2021;366:104396. https://doi.org/10.1016/j.cellimm.2021.104396.
Qin C, Chu Y, Feng W, Fromont C, He S, Ali J, et al. Targeted delivery of lopinavir to HIV reservoirs in the mesenteric lymphatic system by lipophilic ester prodrug approach. J Controlled Release. 2021;329:1077–89. https://doi.org/10.1016/j.jconrel.2020.10.036.
Scholz EMB, Kashuba ADM. The lymph node reservoir: physiology, HIV infection, and Antiretroviral therapy. Clin Pharmacol Ther. 2021;109(4):918–27. https://doi.org/10.1002/cpt.2186.
Dahan A, Hoffman A. Evaluation of a chylomicron flow blocking approach to investigate the intestinal lymphatic transport of lipophilic drugs. Eur J Pharm Sci. 2005;24(4):381–8. https://doi.org/10.1016/j.ejps.2004.12.006.
Liao H, Gao Y, Lian C, Zhang Y, Wang B, Yang Y, et al. Oral absorption and lymphatic transport of baicalein following drug–phospholipid complex incorporation in self-microemulsifying drug delivery systems. IJN. 2019;14:7291–306. https://doi.org/10.2147/IJN.S214883.
Qiao J, Ji D, Sun S, Zhang G, Liu X, Sun B, et al. Oral bioavailability and lymphatic transport of pueraria flavone-loaded self-emulsifying drug-delivery systems containing sodium taurocholate in rats. Pharmaceutics. 2018;10(3):147. https://doi.org/10.3390/pharmaceutics10030147.
Desai J, Thakkar H. Enhanced oral bioavailability and brain uptake of Darunavir using lipid nanoemulsion formulation. Colloids Surf B Biointerfaces. 2019;175:143–9. https://doi.org/10.1016/j.colsurfb.2018.11.057.
Nielsen PB, Müllertz A, Norling T, Kristensen HG. Comparison of the lymphatic transport of a lipophilic drug from vehicles containing α-tocopherol and/or triglycerides in rats. J Pharm Pharmacol. 2010;53(11):1439–45. https://doi.org/10.1211/0022357011777972.
Shete H, Chatterjee S, De A, Patravale V. Long chain lipid based tamoxifen NLC. Part II: pharmacokinetic, biodistribution and in vitro anticancer efficacy studies. Int J Pharm. 2013;454(1):584–92. https://doi.org/10.1016/j.ijpharm.2013.03.036.
Sulkowski MS. Hepatotoxicity associated with antiretroviral therapy containing HIV-1 protease inhibitors. Semin Liver Dis. 2003;23(2):183–94. https://doi.org/10.1055/s-2003-39949.
Anghel L, Baroiu L, Beznea A, Grigore G. The therapeutic relevance of vitamin E. Revista de Chimie. 2019;70:3711–3. https://doi.org/10.37358/RC.19.10.7630.
Graham SM, Baeten JM, Richardson BA, Bankson DD, Lavreys L, Ndinya-Achola JO, et al. Higher pre-infection vitamin E levels are associated with higher mortality in HIV-1-infected Kenyan women: a prospective study. BMC Infec Dis. 2007;7(1):63. https://doi.org/10.1186/1471-2334-7-63.
Ijaz M, Akhtar N. Fatty acids based α-Tocopherol loaded nanostructured lipid carrier gel: in vitro and in vivo evaluation for moisturizing and anti-aging effects. J Cosmet Dermatol. 2020;19(11):3067–76. https://doi.org/10.1111/jocd.13346.
Caddeo C, Manca ML, Peris JE, Usach I, Diez-Sales O, Matos M, et al. Tocopherol-loaded transfersomes: in vitro antioxidant activity and efficacy in skin regeneration. Int J Pharm. 2018;551(1–2):34–41. https://doi.org/10.1016/j.ijpharm.2018.09.009.
Palipoch S, Punsawad C, Koomhin P, Suwannalert P. Hepatoprotective effect of curcumin and alpha-tocopherol against cisplatin-induced oxidative stress. BMC Complement Altern Med. 2014;14:111. https://doi.org/10.1186/1472-6882-14-111.
Beach RS, Mantero-Atienza E, Shor-Posner G, Javier JJ, Szapocznik J, Morgan R, et al. Specific nutrient abnormalities in asymptomatic HIV-1 infection. AIDS. 1992;6(7):701–8. https://doi.org/10.1097/00002030-199207000-00013.
Tang AM, Graham NM, Semba RD, Saah AJ. Association between serum vitamin A and E levels and HIV-1 disease progression. AIDS. 1997;11(5):613–20. https://doi.org/10.1097/00002030-199705000-00009.
Acknowledgements
The authors thank the Department of Pharmaceutics and Pharmacology of MCOPS, MAHE, Manipal, Karnataka, India, for providing facilities to conduct the study.
Funding
The ICMR, New Delhi, India, provided a Senior Research Fellowship (SRF) to authors Mr. Srinivas Reddy Jitta, Ms. Navya Ajitkumar Bhaskaran, and Ms. Sri Pragnya Cheruku, and the AICTE, New Delhi, India, provided National Doctoral Fellowship (NDF) to Ms. Salwa.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Srinivas Reddy Jitta, Salwa, Navya Ajitkumar Bhaskaran, Shirleen Miriam Marques, Lalit Kumar, SriPragnya Cheruku, Vanishree Rao, Pravesh Sharma, Onkar Kulkarni. The first draft of the manuscript was written by Srinivas Reddy Jitta and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. Srinivas Reddy Jitta: methodology; formal analysis; data acquisition; original draft. Salwa: methodology; formal analysis; data acquisition. Navya Ajitkumar Bhaskaran: methodology; formal analysis; data acquisition. Shirleen Miriam Marques: formal analysis; data acquisition. Dr Lalit Kumar: conceptualization; data curation; formal analysis; funding acquisition; investigation; methodology; project administration; resources; supervision; validation; visualization; roles/writing-original draft; writing—review and editing. Sri Pragnya Cheruku: formal analysis; data acquisition. Vanishree Rao: formal analysis; data acquisition. Pravesh Sharma: formal analysis; data acquisition. Onkar Prakash Kulkarni: formal analysis; data acquisition.
Corresponding author
Ethics declarations
Ethics approval
All animal studies were conducted with prior approval from the Institutional animal ethical committee (approval No. IAEC/KMC/51/2018 and IAEC/KMC/72/2021).
Animal studies
All institutional and national guidelines for the care and use of laboratory animals were followed.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jitta, S.R., Salwa, Bhaskaran, N.A. et al. Enhanced tissue distribution of ritonavir-loaded nanostructured lipid carriers—recommending its dose reduction. Drug Deliv. and Transl. Res. 14, 116–130 (2024). https://doi.org/10.1007/s13346-023-01386-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-023-01386-9