Abstract
Tranylcypromine (logP = 1.34, MW = 133.19 g/mol) is a monoamine oxidase inhibitor used in treating major depressive disorder and is available only as oral tablets. Transdermal delivery of tranylcypromine minimizes hepatic and gastrointestinal side effects associated with oral dosing and prevents systemic side effects improving patient compliance. A two-day suspension-based transdermal delivery method was developed in this study, and the delivery of tranylcypromine across dermatomed porcine ear skin was evaluated. Different penetration enhancers were screened, namely, isopropyl myristate, oleyl alcohol, oleic acid, and a combination of oleic acid and oleyl alcohol. Isopropyl myristate was chosen as the penetration enhancer, and suspension-based transdermal patches were formulated with acrylate and polyisobutylene pressure-sensitive adhesives by the solvent evaporation method. The release liner and backing membrane were chosen, and the drying time for each patch was optimized. The optimized patches were characterized for their adhesive properties, drying time, peel test, shear strength, and uniformity in drug content. In vitro permeation studies were performed on dermatomed porcine ear skin using vertical static Franz diffusion cells, and the receptor samples were collected at predetermined time points for 48 h. The samples were analyzed in a validated UPLC method. Acrylate-based suspension patch delivered a significantly higher amount of drug (712 ± 21.46 μg/cm2) as compared to passive delivery from drug dissolved in propylene glycol (461.49 ± 75.55 μg/cm2), reaching the two-day therapeutic target. However, the PIB-based suspension patch delivered 559.25 ± 12.37 μg/cm2 of tranylcypromine across the skin but did not reach the required target.
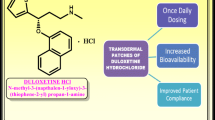
Graphical Abstract







Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are included in the manuscript.
Abbreviations
- ANOVA:
-
Analysis of variance
- IPM:
-
Isopropyl myristate
- LOD :
-
Limit of detection
- LOQ:
-
Limit of quantification
- OA:
-
Oleic acid
- PBS:
-
Phosphate-buffered saline
- PIB:
-
Polyisobutylene
- PG:
-
Propylene glycol
- PSA:
-
Pressure sensitive adhesive
- TDS:
-
Transdermal delivery system
- UPLC:
-
Ultra-performance liquid chromatography
References
Mayoclinic. Depression (major depressive disorder). https://www.mayoclinic.org/diseases-conditions/depression/symptoms-causes/syc-20356007. 2018.
Kang H-J, Kim S-Y, Bae K-Y, Kim S-W, Shin I-S, Yoon J-S, et al. Comorbidity of depression with physical disorders: research and clinical implications. Chonnam Med J. 2015;51:8–18.
Brody DJ, Pratt LA, Hughes JP. Prevalence of depression among adults aged 20 and over: United States, 2013–2016. NCHS data brief. 2018.
World Health Organization. Depression. 2018. https://www.who.int/news-room/fact-sheets/detail/depression. Accessed 5 July 2022.
Andrews G. Should depression be managed as a chronic disease? Br Med J. 2001;322:419–21.
Volz HP, Gleiter CH. Monoamine oxidase inhibitors: a perspective on their use in the elderly. Drugs Aging. 1998;13(5):341–55.
Quitkin F, Stewart J, McGrath P, Harrison W, Markowitz J, Tricamo E, et al. Phenelzine vs imipramine in the treatment of probable atypical depression: defining syndrome boundaries of selective MAOI responders. Am J Psychiatry. 1988;145(3):306–11.
Lee KC, Chen JJ. Transdermal selegiline for the treatment of major depressive disorder. Neuropsychiatr Dis Treat. 2007;3(5):527–37.
Kiani C. Tranylcypromine: its pharmacology, safety, and efficacy. Am J Psychiatry Resid J. 2020;3–5.
U.S. Food and Drug Administration. EMSAM® (Selegiline Transdermal System). 2007.
Saroha K, Yadav B, Sharma B. Transdermal patch: a discrete dosage form. Int J Curr Pharm Res. 2011;3(3):98–108.
Chemicalize - Instant Cheminformatics. Tranylcypromine. https://chemicalize.com/app/calculation. 2022. Accessed 08 July 2022.
Pubchem. Tranylcypromine. https://pubchem.ncbi.nlm.nih.gov/compound/Tranylcypromine#section=Color-Form. 2022. Accessed 10 July 2022.
Ulrich S, Ricken R, Adli M. Tranylcypromine in mind (Part I): Review of pharmacology. Eur Neuropsychopharmacol. 2017;27(8):697–713.
U.S. Food and Drug Administration. Parnate. 2018. Accessed 10 July 2022.
Margetts L, Sawyer R. Transdermal drug delivery: principles and opioid therapy. Contin Educ Anaesthesia, Crit Care Pain. 2007;7(5):171–6.
US Food and Drug Administration. Transdermal and topical delivery systems - product development and quality considerations, Food and Drug Administration, Draft Guidance. 2019. Accessed 10 July 2022.
Nalamachu S, Gudin J. Characteristics of analgesic patch formulations. J Pain Res. 2020;13:2343–54.
Cilurzo F, Gennari CGM, Minghetti P. Adhesive properties: a critical issue in transdermal patch development. Expert Opin Drug Deliv. 2012;9(1):33–45.
Dandekar AA, Garimella HT, German CL, Banga AK. Microneedle mediated iontophoretic delivery of tofacitinib citrate. Pharm Res. 2022;(0123456789).
Cilurzo F, Gennari CGM, Minghetti P. Adhesive properties: a critical issue in transdermal patch development. Expert Opin Drug Deliv. 2011;9(1):33–45.
Pizzi A, Mittal KL. Handbook of adhesive technology. 3rd ed. Marcel Dekker, Inc. 2003;223–262.
Sharma M. Transdermal and intravenous nano drug delivery systems: present and future. Applications of targeted nano drugs and delivery systems: nanoscience and nanotechnology in drug delivery. Elsevier Inc. 2018;499–550.
Alkilani AZ, McCrudden MTC, Donnelly RF. Transdermal drug delivery: innovative pharmaceutical developments based on disruption of the barrier properties of the stratum corneum. Pharmaceutics. 2015;7(4):438–70.
Touitou E. Drug delivery across the skin. Expert Opin Biol Ther. 2002;2(7):723–33.
Vora D, Dandekar A, Bhattaccharjee S, Singh ON, Agrahari V, Peet MM, et al. Formulation development for transdermal delivery of raloxifene, a chemoprophylactic agent against breast cancer. Pharmaceutics. 2022;14:680.
Hadgraft J. Percutaneous absorption: possibilities and problems. Int J Pharm. 1983;16:255–70.
Walker RB, Smith EW. The role of percutaneous penetration enhancers. Adv Drug Deliv Rev. 1996;18(3):295–301.
Ganti SS, Bhattaccharjee SA, Murnane KS, Blough BE, Banga AK. Formulation and evaluation of 4-benzylpiperidine drug-in-adhesive matrix type transdermal patch. Int J Pharm. 2018;550:71–8.
Carvalho ALM, Silva JA, Lira AAM, Almeida EDP, Nunes R de S, Sarmento VHV, et al. Third-generation transdermal delivery systems containing zidovudine: effect of the combination of different chemical enhancers and a microemulsion system. AAPS PharmSciTech. 2018;19(7):3219–27.
Arellano A, Santoyo S, Martín C, Ygartua P. Influence of propylene glycol and isopropyl myristate on the in vitro percutaneous penetration of diclofenac sodium from carbopol gels. Eur J Pharm Sci. 1998;7:129–35.
Suh H, Jun HW. Effectiveness and mode of action of isopropyl myristate as a permeation enhancer for naproxen through shed snake skin. J Pharm Pharmacol. 1996;48:812–6.
Pastore MN, Kalia YN, Horstmann M, Roberts MS. Transdermal patches: history, development and pharmacology. Br J Pharmacol. 2015;172:2179–209.
Suksaeree J, Siripornpinyo P, Chaiprasit S. Formulation, characterization, and in vitro evaluation of transdermal patches for inhibiting crystallization of mefenamic acid. J Drug Deliv. 2017;1–7.
Jain P, Banga AK. Inhibition of crystallization in drug-in-adhesive-type transdermal patches. Int J Pharm. 2010;394:68–74.
Kenneth J. Miller, II SKG, Bhatia KS. Fentanyl suspension-based silicone adhesive formulations and devices fortransidermal delivery of fentanyl. Unites States; US 7,556,823 B2, 2009;1–17.
Park CW, Son DD, Kim JY, Oh TO, Ha JM, Rhee YS, et al. Investigation of formulation factors affecting in vitro and in vivo characteristics of a galantamine transdermal system. Int J Pharm. 2012;436:32–40.
Valia KH, Rossi MT, Kydonieus A. KAT Transdermals LLC. Selegiline transdermal system. USA. US9539201B2 (Patent). 2017.
Sun S, Li M, Liu A. A review on mechanical properties of pressure sensitive adhesives. Int J Adhes Adhes. 2013;41:98–106.
Banerjee S, Chattopadhyay P, Ghosh A, Datta P, Veer V. Aspect of adhesives in transdermal drug delivery systems. Int J Adhes Adhes. 2014;50:70–84.
Wokovich AM, Shen M, Doub WH, Machado SG, Buhse LF. Release liner removal method for transdermal drug delivery systems (TDDS). J Pharm Sci. 2010;99(7):3177–87.
Funding
The authors have no external funding sources to declare.
Author information
Authors and Affiliations
Contributions
Nisha Shrestha: conceptualization, formal analysis, investigation, methodology, visualization, and writing—original draft. Ajay K. Banga: conceptualization, methodology, supervision, and writing—review and editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
The authors have read the manuscript and give their consent to publish the manuscript.
Competing interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shrestha, N., Banga, A.K. Development and evaluation of transdermal delivery system of tranylcypromine for the treatment of depression. Drug Deliv. and Transl. Res. 13, 1048–1058 (2023). https://doi.org/10.1007/s13346-022-01269-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-022-01269-5