Abstract
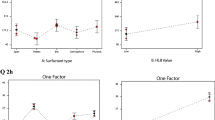
The use of Δ9-tetrahydrocannabinol (THC) and Δ9-tetrahydrocannabinol-valine-hemisuccinate (THC-VHS; NB1111) has recently been investigated in the management of intraocular pressure (IOP). The current study was undertaken to develop an optimized THC-VHS-loaded nanoemulsion formulation (NE; THC-VHS-NE) that could improve the drug load and duration of activity. THC-VHS-NE formulation was prepared by homogenization followed by ultrasonication. Sesame oil, Tween®80, and Poloxamer®188 were used as the oil, surfactant, and cosurfactant, respectively. Stability of the optimized THC-VHS-NE formulation was observed at 4 °C. The IOP lowering effect of the lead formulations, commercial timolol, and latanoprost ophthalmic solutions, as well as an emulsion in Tocrisolve™ (THC-VHS-TOC), was studied in New Zealand White rabbits following topical administration. The effect of surfactant concentration and sterilization process on IOP-lowering activity was also studied. THC-VHS-NE formulations (0.5, 1.0, and 2.0% w/v) showed dose dependent duration of action. The 1.0%w/v THC-VHS-NE formulation was selected for further evaluation because of its desirable physical and chemical characteristics. THC-VHS-NE formulation prepared with 2% w/v Tween®80 exhibited a higher drop in IOP than the 0.75 and 4.0% w/v of Tween®80 containing formulations. The IOP-lowering duration was, however, similar for the formulations with 0.75 and 2.0% Tween®80, while that with 4.0% Tween®80 was shorter. THC-VHS-NE formulation produced a greater drop in IOP (p < 0.05) and a longer duration of activity compared to THC-VHS-TOC, latanoprost, and timolol. The formulation could be sterilized by filtration without impacting product attributes. Overall, the optimized THC-VHS-NE formulation demonstrated a significantly better IOP reduction profile in the test model compared to the commercial ophthalmic solutions evaluated.
Graphical abstract






Similar content being viewed by others
References
Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: a review. JAMA. 2014;311:1901.
Taskar PS, Patil A, Lakhani P, Ashour E, Gul W, ElSohly MA, et al. Δ9-Tetrahydrocannabinol derivative-loaded nanoformulation lowers intraocular pressure in normotensive rabbits. Transl Vis Sci Technol. 2019;8:15–15.
Parihar JKS. Glaucoma: the ‘Black hole’ of irreversible blindness. Med J Armed Forces India. 2016;72:3–4.
Flaxman SR, Bourne RRA, Resnikoff S, Ackland P, Braithwaite T, Cicinelli MV, et al. Global causes of blindness and distance vision impairment 1990–2020: a systematic review and meta-analysis. Lancet Glob Health. 2017;5:e1221–34.
Goel M, Picciani RG, Lee RK, Bhattacharya SK. Aqueous humor dynamics: a review. Open Ophthalmol J. 2010;4:52–9.
Braunger BM, Fuchshofer R, Tamm ER. The aqueous humor outflow pathways in glaucoma: a unifying concept of disease mechanisms and causative treatment. Eur J Pharm Biopharm. 2015;95:173–81.
Tham Y-C, Li X, Wong TY, Quigley HA, Aung T, Cheng C-Y. Global prevalence of glaucoma and projections of glaucoma burden through 2040. Ophthalmology. 2014;121:2081–90.
Glaucoma Summary Benchmarks - 2018 [Internet]. AAO; 2017 Nov p. 6. Available from: https://www.aao.org/summary-benchmark-detail/glaucoma-summary-benchmarks-2018
Glaucoma - Diagnosis and treatment - Mayo Clinic [Internet]. [cited 2019 Oct 15]. Available from: https://www.mayoclinic.org/diseases-conditions/glaucoma/diagnosis-treatment/drc-20372846
Adelli GR, Bhagav P, Taskar P, Hingorani T, Pettaway S, Gul W, et al. Development of a Δ9-tetrahydrocannabinol amino acid-dicarboxylate prodrug with improved ocular bioavailability. Invest Ophthalmol Vis Sci. 2017;58:2167–79.
Green K. Marijuana smoking vs cannabinoids for glaucoma therapy. Arch Ophthalmol. 1998;116:1433–7.
Abrahamov A, Abrahamov A, Mechoulam R. An efficient new cannabinoid antiemetic in pediatric oncology. Life Sci. 1995;56:2097–102.
Hepler RS, Frank IM, Ungerleider JT. Pupillary constriction after marijuana smoking. Am J Ophthalmol. 1972;74:1185–90.
Marijuana and Medicine: Assessing the Science Base [Internet]. Washington, D.C.: National Academies Press; 1999 [cited 2020 Jan 23]. Available from: https://www.nap.edu/catalog/6376
Merritt JC, Crawford WJ, Alexander PC, Anduze AL, Gelbart SS. Effect of marihuana on intraocular and blood pressure in glaucoma. Ophthalmology. 1980;87:222–8.
Flach AJ. Delta-9-tetrahydrocannabinol (THC) in the treatment of end-stage open-angle glaucoma. Trans Am Ophthalmol Soc. 2002;100:215–24.
Miller S, Daily L, Leishman E, Bradshaw H, Straiker A. Δ9-Tetrahydrocannabinol and cannabidiol differentially regulate intraocular pressure. Invest Ophthalmol Vis Sci. 2018;59(15):5904–11.
Green K, Bigger JF, Kim K, Bowman K. Cannabinoid penetration and chronic effects in the eye. Exp Eye Res. 1977;24:197–205.
Hingorani T, Gul W, ElSohly M, Repka MA, Majumdar S. Effect of ion-pairing on in vitro transcorneal permeability of a Δ9-tetrahydrocannabinol prodrug: potential in glaucoma therapy. J Pharm Sci. 2012;101:616–26.
Elsohly MA, Gul W, Repka MA, Majumdar S, inventors; ElSohly Laboratories Inc, assignee. Compositions containing delta-9-thc-amino acid esters and process of preparation. United States patent US 8,809,261. 2014 Aug 19.
Thumma S, Majumdar S, ElSohly MA, Gul W, Repka MA. Preformulation studies of a prodrug of Δ 9-tetrahydrocannabinol. AAPS PharmSciTech Sep 1. 2008;9(3):982–90.
Urtti A, Salminen L. Minimizing systemic absorption of topically administered ophthalmic drugs. Surv Ophthalmol. 1993;37:435–56.
Kale SN, Deore SL. Emulsion micro emulsion and nano emulsion: A Review. 2016.
Sharma N, Bansal M, Visht S, Sharma P, Kulkarni G. Nanoemulsion: a new concept of delivery system. Chron Young Sci. 2010;5.
Patel A, Cholkar K, Agrahari V, Mitra AK. Ocular drug delivery systems: an overview. World J Pharmacol. 2013;2:47–64.
Kumari B. Ocular drug delivery system: approaches to improve ocular bioavailability. GSC Biol Pharm Sci. 2019;6:001–10.
Youssef A, Dudhipala N, Majumdar S. Ciprofloxacin loaded nanostructured lipid carriers incorporated into in-situ gels to improve management of bacterial endophthalmitis. Pharmaceutics Jun. 2020;12(6):572.
Janga KY, Tatke A, Dudhipala N, Balguri SP, Ibrahim MM, Maria DN, Jablonski MM, Majumdar S. Gellan gum based sol-to-gel transforming system of natamycin transfersomes improves topical ocular delivery. J Pharmacol Exp Ther Sep 1. 2019;370(3):814–22.
Inactive Ingredient Search for Approved Drug Products [Internet]. [cited 2020 Jan 28]. Available from: https://www.accessdata.fda.gov/scripts/cder/iig/index.cfm?event=browseByLetter.page&Letter=P
Abismaı̈l B, Canselier JP, Wilhelm AM, Delmas H, Gourdon C. Emulsification by ultrasound: drop size distribution and stability. Ultrason Sonochem. 1999;6:75–83.
Delmas T, Piraux H, Couffin A-C, Texier I, Vinet F, Poulin P, et al. How to prepare and stabilize very small nanoemulsions. Langmuir American Chemical Society. 2011;27:1683–92.
Lovelyn C, Attama AA. Current state of nanoemulsions in drug delivery. J Biomater Nanobiotechnology. 2011;02:626–39.
Tatke A, Dudhipala N, Janga KY, Balguri SP, Avula B, Jablonski MM, Majumdar S. In situ gel of triamcinolone acetonide-loaded solid lipid nanoparticles for improved topical ocular delivery: tear kinetics and ocular disposition studies. Nanomaterials. 2019;9(1):33.
Guan Y, Wu J, Zhong Q. Eugenol improves physical and chemical stabilities of nanoemulsions loaded with β-carotene. Food Chem. 2016;194:787–96.
Diebold Y, Calonge M. Applications of nanoparticles in ophthalmology. Prog Retin Eye Res. 2010;29:596–609.
Ban J, Zhang Y, Huang X, Deng G, Hou D, Chen Y, et al. Corneal permeation properties of a charged lipid nanoparticle carrier containing dexamethasone. Int J Nanomedicine. 2017;12:1329–39.
Chanana GD, Sheth BB. Particle size reduction of emulsions by formulation design-II: effect of oil and surfactant concentration. PDA J Pharm Sci Technol. 1995;49:71–6.
Pepi I, Lovri J, Filipovi J. Polymeric micelles in ocular drug delivery: rationale, strategies and challenges. :14.
Kiland JA, Gabelt BT, Kaufman PL. Studies on the mechanism of action of timolol and on the effects of suppression and redirection of aqueous flow on outflow facility. Exp Eye Res. 2004;78:639–51.
Lim KS, Nau CB, O’Byrne MM, Hodge DO, Toris CB, McLaren JW, et al. Mechanism of action of bimatoprost, latanoprost, and travoprost in healthy subjects: a crossover study. Ophthalmology. 2008;115:790–5.
Funding
This work has been supported by a research grant from Emerald Bioscience, INC.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics declarations
All animal experiments conformed to the tenets of the Association for Research in Vision and Ophthalmology statement on the Use of Animals in Ophthalmic and Vision Research and followed the University of Mississippi Institutional Animal Care and Use Committee approved protocols (18-029).
Conflict of interest
This research is sponsored by Emerald Bioscience, INC, and may lead to the development of products from which W.G., M.E., and S.M. may receive income as part of licensing fees and royalties paid to the University of Mississippi. M.E. is a scientific advisor to Emerald Bioscience. B.M. was the CMO of Emerald Bioscience, Inc. No competing financial interests exist for the other authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sweeney, C., Dudhipala, N., Thakkar, R. et al. Effect of surfactant concentration and sterilization process on intraocular pressure–lowering activity of Δ9-tetrahydrocannabinol-valine-hemisuccinate (NB1111) nanoemulsions. Drug Deliv. and Transl. Res. 11, 2096–2107 (2021). https://doi.org/10.1007/s13346-020-00871-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-020-00871-9