Abstract
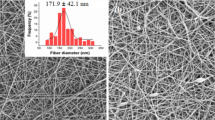
Aiming to develop biological skin dresses with improved performance in the treatment of skin wounds, acellular collagen I scaffolds were modified with polymeric microparticles and the subsequent loading of a hydroglycolic extract of Calendula officinalis flowers. Microparticles made of gelatin-collagen were produced by a water-in-oil emulsion/cross-linking method. Thereafter, these microparticles were mixed with collagen suspensions at three increasing concentrations and the resulting mixtures lyophilized to make microparticle-loaded porous collagen scaffolds. Resistance to enzymatic degradation, ability to associate with the C. officinalis extract, and the extract release profile of the three gelatin-collagen microparticle-scaffold prototypes were assessed in vitro and compared to collagen scaffolds without microparticles used as control. Data indicated that the incorporation of gelatin-collagen microparticles increased the resistance of the scaffolds to in vitro enzymatic degradation, as well as their association with the C. officinalis flower extract. In addition, a sharp decrease in cytotoxicity, as well as more prolonged release of the extract, was attained. Overall results support the potential of these systems to develop innovative dermal substitutes with improved features. Furthermore, the gelatin-collagen mixture represents a low-cost and scalable alternative with high clinical transferability, especially appealing in developing countries.

To develop biological skin dresses with improved performance in the treatment of chronic skin wounds, gelatin-collagen microparticles were mixed with collagen suspensions and the resulting mixtures lyophilized to make porous scaffolds. Scaffolds were then loaded with a hydroglycolic extract of C. officinalis flowers and fully characterized in vitro.





Similar content being viewed by others
References
Yannas IV. Emerging rules for inducing organ regeneration. Biomaterials. 2013;34:321–30.
Rajan N, Habermehl J, Coté M-F, Doillon CJ, Mantovani D. Preparation of ready-to-use, storable and reconstituted type I collagen from rat tail tendon for tissue engineering applications. Nat Prot. 2007;1:2753–8.
Espinosa L, Sosnik A, Fontanilla MR. Development and preclinical evaluation of acellular collagen scaffolding and autologous artificial connective tissue in the regeneration of oral mucosa wounds. Tissue Eng Part A. 2010;16:1667–79.
Fontanilla MR, Espinosa LG. In vitro and in vivo assessment of oral autologous artificial connective tissue characteristics that influence its performance as a graft. Tissue Eng Part A. 2012;18:1857–66.
Wong T, McGrath JA, Navsaria H. The role of fibroblasts in tissue engineering and regeneration. Br J Dermatol. 2007;156:1149–55.
Tabata Y. Biomaterial technology for tissue engineering applications. J R Soc Interface. 2009;6:S311–324.
Geiger M, Li RH, Friess W. Collagen sponges for bone regeneration with rhBMP-2. Adv Drug Deliv Rev. 2003;55:1613–29.
Shi J, Votruba AR, Farokhzad OC, Langer R. Nanotechnology in drug delivery and tissue engineering: from discovery to applications. Nano Lett. 2010;10:3223–30.
Basch E, Bent S, Foppa I, Haskmi S, Kroll D, Mele M, et al. Marigold (Calendula officinalis L.): an evidence-based systematic review by the Natural Standard Research Collaboration. J Herbal Pharmacother. 2006;6:135–59.
Fonseca YM, Catini CD, Vicentini FT, Nomizo A, Gerlach RF, Fonseca MJ. Protective effect of Calendula officinalis extract against UVB-induced oxidative stress in skin: Evaluation of reduced glutathione levels and matrix metalloproteinase secretion. J Ethnopharmacol. 2010;127:596–601.
Preethi KC, Kuttan G, Kuttan R. Anti-inflammatory activity of flower extract of Calendula officinalis Linn. and its possible mechanism of action. Indian J Exp Biol. 2009;47:113–20.
Brown DJ, Dattner AM. Phytotherapeutic approaches to common dermatologic conditions. Arch Dermatol. 1998;134:1401–4.
Lee JE, Kim KE, Kwon IC, Ahn HJ, Lee SH, Cho H, et al. Effects of the controlled-released TGF-beta 1 from chitosan microspheres on chondrocytes cultured in a collagen/chitosan/glycosaminoglycan scaffold. Biomaterials. 2004;25:4163–73.
Kimura Y, Tsuji W, Yamashiro H, Toi M, Inamoto T, Tabata Y. In situ adipogenesis in fat tissue augmented by collagen scaffold with gelatin microspheres containing basic fibroblast growth factor. J Tissue Eng Regen Med. 2010;4:55–61.
Bustos RH, Suesca E, Millan D, Gonzalez JM, Fontanilla MR. Real-time quantification of proteins secreted by artificial connective tissue made from uni- or multidirectional collagen I scaffolds and oral mucosa fibroblasts. Anal Chem. 2014;86:2421–8.
Schäfer M, Werner S. Oxidative stress in normal and impaired wound repair. Pharmacol Res. 2008;58(2):165–71.
Kawai K, Suzuki S, Tabata Y, Ikada Y, Nishimura Y. Accelerated tissue regeneration through incorporation of basic fibroblast growth factor-impregnated gelatin microspheres into artificial dermis. Biomaterials. 2000;21:489–99.
ISO. The International Organization for Standardization 10993–5. Biological evaluation of medical devices Part 5: Tests for in vitro cytotoxicity. 2009;1–24.
USP. The United States Pharmacopeia. Biological reactivity tests in vitro. 2013;87:36, 1832.
Singleton VL, Rossi JA. Colorimetry of total phenolics with phosphomolybdic-phosphotungstic acid reagents. Am J Enol Viticult. 1965;16:144–58.
Shah VP, Tsong Y, Sathe P, Liu JP. In vitro dissolution profile comparison-statistics and analysis of the similarity factor, f2. Pharm Res. 1998;15:889–96.
Freiberg S, Zhu XX. Polymer microspheres for controlled drug release. Int J Pharm. 2004;282:1–18.
Tran VT, Benoit JP, Venier-Julienne MC. Why and how to prepare biodegradable, monodispersed, polymeric microparticles in the field of pharmacy? Int J Pharm. 2011;407:1–11.
Galeska I, Kim TK, Patil SD, Bhardwaj U, Chatttopadhyay D, Papadimitrakopoulos F, et al. Controlled release of dexamethasone from PLGA microspheres embedded within polyacid-containing PVA hydrogels. AAPS J. 2005;7:E231–40.
Ju YM, Yu B, West L, Moussy Y, Moussy F. A dexamethasone-loaded PLGA microspheres/collagen scaffold composite for implantable glucose sensors. J Biomed Mater Res Part A. 2010;93:200–10.
Holzapfel BM, Reichert JC, Schantz JT, Gbureck U, Rackwitz L, Noth U, et al. How smart do biomaterials need to be? A translational science and clinical point of view. Adv Drug Deliv Rev. 2013;65:581–603.
Murphy GF, Orgill DP, Yannas IV. Partial dermal regeneration is induced by biodegradable collagen-glycosaminoglycan grafts. Lab Invest. 1990;62:305–13.
Freyman TM, Yannas IV, Gibson LJ. Cellular materials as porous scaffolds for tissue engineering. Prog Mat Sci. 2001;46:273–82.
Defail AJ, Edington HD, Matthews S, Lee WC, Marra KG. Controlled release of bioactive doxorubicin from microspheres embedded within gelatin scaffolds. J Biomed Mater Res Part A. 2006;79:954–62.
Kikkinides ES, Charalambopoulou GC, Stubos AK, Kanellopoulos NK, Varelas CG, Steiner CA. A two-phase model for controlled drug release from biphasic polymer hydrogels. J Control Release. 1998;51:313–25.
Friess W. Collagen-biomaterial for drug delivery. Eur J Pharm Biopharm. 1998;45:113–36.
Korsemeyer RW, Gurny R, Doelker EM, Buri P, Peppas NA. Mechanism of solute release from porous hydrophilic polymers. Int J Pharm. 1983;15:25–35.
Ritger PL, Peppas NA. A simple equation for description of solute release. I. Fickian and non-Fickian release from non-swellable devices in the form of slabs, spheres, cylinders or discs. J Control Release. 1987;5:23–6.
Acknowledgments
This work was supported by Universidad Nacional de Colombia and the Colombian Department of Science, Technology and Innovation (COLCIENCIAS) (grants 1101-521-28661 and 1101-452-21387). We would like to thank Gabriel Zea Jimenez for his contribution to the preliminary experiments and “Fundación Instituto de Inmunología de Colombia” for lending us facilities to make the microparticles. Ronald Jimenez was financed by the Faculty of Science at Universidad Nacional de Colombia (teaching assistant scholarship) and by COLCIENCIAS (grant 1101-521-28661). Edward Suesca and Diana Millán were also supported by COLCIENCIAS (grants 1101-452-21387 and 1101-521-28661).
Conflict of interest
Ronald A. Jiménez, Diana Millán, Edward Suesca, Alejandro Sosnik, and Marta R. Fontanilla declare that they have no conflict of interest. The authors declare no competing financial interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Ronald A. Jiménez and Diana Millán contributed equally to this work.
Rights and permissions
About this article
Cite this article
Jiménez, R.A., Millán, D., Suesca, E. et al. Controlled release of an extract of Calendula officinalis flowers from a system based on the incorporation of gelatin-collagen microparticles into collagen I scaffolds: design and in vitro performance. Drug Deliv. and Transl. Res. 5, 209–218 (2015). https://doi.org/10.1007/s13346-015-0217-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-015-0217-3