Abstract
Aims
We aimed to identify patients who would benefit from basal insulin-supported oral therapy (BOT) with a glinide and an α-glucosidase inhibitor (a fixed-dose combination tablet of mitiglinide 10 mg and voglibose 0.2 mg) in Japanese type 2 diabetic patients.
Methods
Patients who were hospitalized to improve hyperglycemia received basal–bolus insulin therapy. After the reduction of glucose toxicity, a 75 g oral glucose tolerance test and a glucagon test were performed. Thereafter, the basal–bolus insulin therapy was switched to BOT with mitiglinide, followed by further addition of voglibose. Interstitial glucose levels were continuously monitored throughout the study period. Diurnal glucose profile was recorded and analyzed. Patients were divided into two groups according to whether their percentage of time in range (TIR, 70–180 mg/dL) under BOT with mitiglinide/voglibose was higher than 70% or not, and the differences in clinical characteristics between the groups were analyzed.
Results
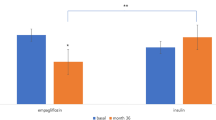
Twenty patients were enrolled, and 19 of them completed the study. BOT with mitiglinide/voglibose achieved ≥ 70% of TIR in thirteen patients. The area under the curve of serum C-peptide levels during the oral glucose tolerance test was significantly higher in the patients with ≥ 70% of TIR. The daily insulin dosages and blood glucose profiles were comparable between the two groups.
Conclusions
The efficacy of BOT with mitiglinide/voglibose depended on residual insulin secretory abilities. This therapy would be a useful therapeutic option for patients with type 2 diabetes.




Similar content being viewed by others
Data availability
The data sets used and/or analysed in this study are available from the corresponding author on reasonable request.
References
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan B, et al. IDF Diabetes Atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109109. https://doi.org/10.1016/j.diabres.2021.109119.
Takeshita Y, Takamura T, Kita Y, Takazakura A, Kato K, Isobe Y, et al. Sitagliptin versus mitiglinide switched from mealtime dosing of a rapid-acting insulin analog in patients with type 2 diabetes: a randomized, parallel-group study. BMJ Open Diabetes Res Care. 2015. https://doi.org/10.1136/bmjdrc-2015-000122.
Tsukube S, Ikeda Y, Kadowaki T, Odawara M. Improved treatment satisfaction and self-reported health status after introduction of basal-supported oral therapy using insulin glargine in patients with type 2 diabetes: sub-analysis of ALOHA2 study. Diabetes Ther. 2015. https://doi.org/10.1007/s13300-015-0111-5.
Li H. Revisiting the strategies for the pharmacological management of type 2 diabetes—from glycemic control, organ protection, safety to weight reduction. J Diabetes Investig. 2022;13(1):3–5. https://doi.org/10.1111/jdi.13726.
Danne T, Bluhmki T, Seufert J, Kaltheuner M, Rathmann W, Beyersmann J, et al. Treatment intensification using long-acting insulin -predictors of future basal insulin supported oral therapy in the DIVE registry. BMC Endocr Disord. 2015;15:54. https://doi.org/10.1186/s12902-015-0051-0.
Xu W, Qiu L, Luo S, Li M, Weng J, Guo X, et al. Status of basal-supported oral therapy in Chinese type 2 diabetic patients with inadequate glycemic control on oral anti-diabetic drugs. Diabetes Metab Res Rev. 2015;31(8):796–802. https://doi.org/10.1002/dmrr.2709.
Rathmann W, Czech M, Franek E, Kostev K. Regional differences in insulin therapy regimens in five European countries. Int J Clin Pharmacol Ther. 2017;55(5):403–8. https://doi.org/10.5414/CP202906.
ElSayed N, Aleppo G, Aroda V, Bannuru R, Brown F, Bruemmer D, et al. Pharmacologic approaches to glycemic treatment: standards of care in diabetes-2023. Diabetes Care. 2023;46(Suppl 1):S140–57. https://doi.org/10.2337/dc23-S009.
Matthaei S, Bierwirth R, Fritsche A, Gallwitz B, Häring H, Joost H, et al. Medical antihyperglycaemic treatment of type 2 diabetes mellitus: update of the evidence-based guideline of the German Diabetes Association. Exp Clin Endocrinol Diabetes. 2009;117(9):522–57. https://doi.org/10.1055/s-0029-1239559.
Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358(24):2560–72. https://doi.org/10.1056/NEJMoa0802987.
United Kingdom Prospective Diabetes Study Group. United Kingdom Prospective Diabetes Study 24: a 6-year, randomized, controlled trial comparing sulfonylurea, insulin, and metformin therapy in patients with newly diagnosed type 2 diabetes that could not be controlled with diet therapy. Ann Intern Med. 1998;128(3):165–75. https://doi.org/10.7326/0003-4819-128-3-199802010-00001.
Nathan DM, Genuth S, Lachin J, Cleary P, Crofford O, Diabetes Control and Complications Trial Research Group, et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–86. https://doi.org/10.1056/nejm199309303291401.
Katsuno T, Watanabe N, Nagai E, Okazaki K, Yokoyama A, Hamaguchi T, et al. Comparison of efficacy of concomitant administration of mitiglinide with voglibose and double dose of mitiglinide in patients with type 2 diabetes mellitus. J Diabetes Investig. 2011;2(3):204–9. https://doi.org/10.1111/j.2040-1124.2010.00082.x.
Ono Y, Kameda H, Cho K. Mitiglinide/voglibose fixed-dose combination improves postprandial glycemic excursions in Japanese patients with type 2 diabetes mellitus. Expert Opin Pharmacother. 2013;14(4):361–70. https://doi.org/10.1517/14656566.2013.770839.
Fujimoto K, Shibayama Y, Yamaguchi E, Honjo S, Hamasaki A, Hamamoto Y. Glucose excursions and hypoglycemia in patients with type 2 diabetes treated with mitiglinide/voglibose versus glimepiride: a randomized cross-over trial. J Diabetes. 2018;10(8):675–82. https://doi.org/10.1111/1753-0407.12658.
Ihana-Sugiyama N, Yamamoto-Honda R, Sugiyama T, Tsujimoto T, Kakei M, Noda M. Cross-over study comparing postprandial glycemic increase after addition of a fixed-dose mitiglinide/voglibose combination or a dipeptidyl peptidase-4 inhibitor to basal insulin therapy in patients with type 2 diabetes mellitus. Med Sci Monit Basic Res. 2017;23:36–44. https://doi.org/10.12659/msmbr.902218.
Murakami M, Bouchi R, Ohara N, Fukuda T, Minami I, Hashimoto K, et al. Beneficial effect of combination therapy with mitiglinide and voglibose on fasting and postprandial endothelial dysfunction in patients with type2 diabetes: a pilot study. Integr Obesity Diabetes. 2017;3:1.
Ihana N, Tsujimoto T, Yamamoto-Honda R, Kishimoto M, Kajio H, Noto H, et al. Improvement of both fasting and postprandial glycemic control by the two-step addition of miglitol and mitiglinide to basal insulin therapy: a pilot study. Diabetol Metab Syndr. 2014;6:48. https://doi.org/10.1186/1758-5996-6-48.
Battelino T, Danne T, Bergenstal R, Amiel S, Beck R, Biester T, et al. Clinical targets for continuous glucose monitoring data interpretation: recommendations from the International Consensus on Time in Range. Diabetes Care. 2019;42(8):1593–603. https://doi.org/10.2337/dci19-0028.
Service F, Molnar G, Rosevear J, Ackerman E, Gatewood L, Taylor W. Mean amplitude of glycemic excursions, a measure of diabetic instability. Diabetes. 1970;19(9):644–55. https://doi.org/10.2337/diab.19.9.644.
Wallace T, Levy J, Matthews D. Use and abuse of HOMA modeling. Diabetes Care. 2004;27(6):1487–95. https://doi.org/10.2337/diacare.27.6.1487.
Vos R, van Avendonk M, Jansen H, Goudswaard A, van den Donk M, Gorter K, et al. Insulin monotherapy compared with the addition of oral glucose-lowering agents to insulin for people with type 2 diabetes already on insulin therapy and inadequate glycaemic control. Cochrane Database Syst Rev. 2016;9(9):CD006992. https://doi.org/10.1002/14651858.CD006992.pub2.
Chang C, Hsieh C, Huang J, Huang I. Acute and chronic fluctuations in blood glucose levels can increase oxidative stress in type 2 diabetes mellitus. Acta Diabetol. 2012;49(Suppl 1):S171–7. https://doi.org/10.1007/s00592-012-0398-x.
Quagliaro L, Piconi L, Assaloni R, Martinelli L, Motz E, Ceriello A. Intermittent high glucose enhances apoptosis related to oxidative stress in human umbilical vein endothelial cells: the role of protein kinase C and NAD(P)H-oxidase activation. Diabetes. 2003;52(11):2795–804. https://doi.org/10.2337/diabetes.52.11.2795.
Zhang X, Xu X, Jiao X, Wu J, Zhou S, Lv X. The effects of glucose fluctuation on the severity of coronary artery disease in type 2 diabetes mellitus. J Diabetes Res. 2013;2013:576916. https://doi.org/10.1155/2013/576916.
Mazze R, Strock E, Borgman S, Wesley D, Stout P, Racchini J. Evaluating the accuracy, reliability, and clinical applicability of continuous glucose monitoring (CGM): Is CGM ready for real time? Diabetes Technol Ther. 2009;11(1):11–8. https://doi.org/10.1089/dia.2008.0041.
Mu P, Liu D, Lin Y, Liu D, Zhang F, Zhang Y, et al. The postprandial-to-fasting serum c-peptide ratio is a predictor of response to basal insulin-supported oral antidiabetic drug(s) therapy: a retrospective analysis. Diabetes Ther. 2018;9(3):963–71. https://doi.org/10.1007/s13300-018-0404-6.
DECODE Study Group. Glucose tolerance and cardiovascular mortality: comparison of fasting and 2-hour diagnostic criteria. Arch Intern Med. 2001;161(3):397–405. https://doi.org/10.1001/archinte.161.3.397.
Tominaga M, Eguchi H, Manaka H, Igarashi K, Kato T, Sekikawa A. Impaired glucose tolerance is a risk factor for cardiovascular disease, but not impaired fasting glucose. The Funagata Diabetes Study. Diabetes Care. 1999;22(6):920–4. https://doi.org/10.2337/diacare.22.6.920.
Chittari M, McTernan P, Bawazeer N, Constantinides K, Ciotola M, O’Hare J, et al. Impact of acute hyperglycaemia on endothelial function and retinal vascular reactivity in patients with Type 2 diabetes. Diabet Med. 2011;28(4):450–4. https://doi.org/10.1111/j.1464-5491.2010.03223.x.
Gapstur S, Gann P, Lowe W, Liu K, Colangelo L, Dyer A. Abnormal glucose metabolism and pancreatic cancer mortality. JAMA. 2000;283(19):2552–8. https://doi.org/10.1001/jama.283.19.2552.
Abbatecola A, Rizzo M, Barbieri M, Grella R, Arciello A, Laieta M, et al. Postprandial plasma glucose excursions and cognitive functioning in aged type 2 diabetics. Neurology. 2006;67(2):235–40. https://doi.org/10.1212/01.wnl.0000224760.22802.e8.
International Diabetes Federation Guideline Development Group. Guideline for management of postmeal glucose in diabetes. Diabetes Res Clin Pract. 2014;103(2):256–68. https://doi.org/10.1016/j.diabres.2012.08.002.
Sunaga Y, Gonoi T, Shibasaki T, Ichikawa K, Kusama H, Yano H, et al. The effects of mitiglinide (KAD-1229), a new anti-diabetic drug, on ATP-sensitive K+ channels and insulin secretion: comparison with the sulfonylureas and nateglinide. Eur J Pharmacol. 2001;431(1):119–25. https://doi.org/10.1016/s0014-2999(01)01412-1.
Assaloni R, Da Ros R, Quagliaro L, Piconi L, Maier A, Zuodar G, et al. Effects of S21403 (mitiglinide) on postprandial generation of oxidative stress and inflammation in type 2 diabetic patients. Diabetologia. 2005;48(9):1919–24. https://doi.org/10.1007/s00125-005-1849-5.
Kitasato L, Tojo T, Hatakeyama Y, Kameda R, Hashikata T, Yamaoka-Tojo M. Postprandial hyperglycemia and endothelial function in type 2 diabetes: focus on mitiglinide. Cardiovasc Diabetol. 2012;11:79. https://doi.org/10.1186/1475-2840-11-79.
Bonds D, Miller M, Bergenstal R, Buse J, Byington R, Cutler J, et al. The association between symptomatic, severe hypoglycaemia and mortality in type 2 diabetes: retrospective epidemiological analysis of the ACCORD study. BMJ. 2010;340:b4909. https://doi.org/10.1136/bmj.b4909.
Zoungas S, Patel A, Chalmers J, de Galan B, Li Q, Billot L, et al. Severe hypoglycemia and risks of vascular events and death. N Engl J Med. 2010. https://doi.org/10.1056/NEJMoa1003795.
Chow E, Bernjak A, Williams S, Fawdry R, Hibbert S, Freeman J, et al. Risk of cardiac arrhythmias during hypoglycemia in patients with type 2 diabetes and cardiovascular risk. Diabetes. 2014;63(5):1738–2347. https://doi.org/10.2337/db13-0468.
Funakoshi S, Fujimoto S, Hamasaki A, Fujiwara H, Fujita Y, Ikeda K, et al. Utility of indices using C-peptide levels for indication of insulin therapy to achieve good glycemic control in Japanese patients with type 2 diabetes. J Diabetes Investig. 2011;2(4):297–303. https://doi.org/10.1111/j.2040-1124.2010.00096.x.
Acknowledgements
The authors are grateful to many people for their guidance and support in conducting this study and preparing this manuscript, including the following medical staff in Division of Diabetes, Department of Internal Medicine, Aichi Medical University School of Medicine: Yusuke Hayashi, Risa Shimauchi, Yukiko Funahashi, Yuki Uchihara, and Nobuhiro Hirai.
Funding
This study was conducted with funding from Kissei Pharmaceutical Co. Ltd.
Author information
Authors and Affiliations
Contributions
Conceptualization: HK, JN; methodology: TH, ST, YK; formal analysis and investigation: TA, MK, YA-Y, MK, EA-H, TH, MM, YE, EN, RK, HN-S, SA, MK, YY, EY-M, TI, YS-R, CK, EN; writing—original draft preparation: TA, MK, TH; writing—review and editing: HK, JN; supervision: HK, JN.
Corresponding author
Ethics declarations
Conflict of interest
Hideki Kamiya: lecture fees: Novo Nordisk Pharma, Sanofi, Sumitomo Pharma, Nippon Boehringer Ingelheim, Eli Lilly Japan, Daiichi Sankyo, Ono Pharmaceutical, Kissei Pharmaceutical, Mitsubishi Tanabe Pharma, Kowa, Novartis Pharma, MSD, Sanwa Kagaku Kenkyusho, Otsuka Pharmaceutical, Ltd., Terumo, Taisho Pharmaceutical. Research funding: Ono Pharmaceutical, Eli Lilly Japan, Kissei Pharmaceutical. Subsidies or donations: Ono Pharmaceutical, Taisho Pharmaceutical, Sumitomo Pharma, Takeda Pharmaceutical, Mitsubishi Tanabe Pharma, Japan Tobacco, Novo Nordisk Pharma. Endowed departments by commercial entities: Ono Pharmaceutical, Abbott Japan, Sanwa Kagaku Kenkyusho, Kowa, Terumo. Jiro Nakamura: lecture fees: Novo Nordisk Pharma, Sanofi, Daiichi Sankyo, Ono Pharmaceutical, Novartis Pharma, MSD, Taisho Pharmaceutical, Takeda Pharmaceutical, Terumo. Research funding: Eli Lilly Japan, Ono Pharmaceutical, Kissei Pharmaceutical. Subsidies or donations: MSD, Ono Pharmaceutical, Sumitomo Pharma, Takeda Pharmaceutical, Mitsubishi Tanabe Pharma, Japan Tobacco, Novo Nordisk Pharma, Taisho Pharmaceutical. Endowed departments by commercial entities: Ono Pharmaceutical, Abbott Japan, Sanwa Kagaku Kenkyusho, Kowa, Terumo. The other authors declare no conflict of interest.
Ethical approval
All the procedures followed were in accordance with the ethical standards of the Ethics Committee of the Aichi Medical University (Approval No. 15-035, approval data: 09/04/2015) and with the Helsinki Declaration of 1964 and later versions.
Informed consent
Informed consent or substitute for it was obtained from all the patients for being included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Ando, T., Kondo, M., Asada-Yamada, Y. et al. The efficacy of switching basal–bolus insulin therapy to basal insulin-supported oral therapy with a glinide and an α-glucosidase inhibitor in patients with type 2 diabetes depends on insulin secretory capacity, but not on blood glucose profiles and insulin dosages prior to the switching. Diabetol Int 15, 99–108 (2024). https://doi.org/10.1007/s13340-023-00651-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13340-023-00651-z