Abstract
Aims
Muscle atrophy is a diabetic complication, which results in a deterioration in glycemic control in type 2 diabetes mellitus (T2DM) individuals. The psoas muscle mass index (PMI) is a reliable indicator for estimating whole-body muscle mass. We aimed to examine the relationship between clinical parameters and the PMI to clarify the mechanism underlying muscle atrophy in diabetes.
Methods
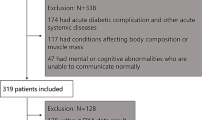
This retrospective, cross-sectional study examined 51 patients (31 men and 20 women) with T2DM and a mean HbA1c value of 9.9 ± 1.7%. These patients were admitted to Aichi Medical University Hospital and underwent abdominal computed tomography imaging from July 2020 to April 2021. Multiple clinical parameters were assessed with the PMI.
Results
In a multiple regression analysis adjusted for age and sex, the PMI was correlated with body weight, body mass index, serum concentrations of corrected calcium, aspartate aminotransferase, alanine aminotransferase, creatine kinase, thyroid-stimulating hormone (TSH), urinary C-peptide concentrations, the free triiodothyronine/free thyroxine (FT3/FT4) ratio, and the young adult mean score at the femur neck. Receiver operating characteristic curves were created using TSH concentrations and the FT3/FT4 ratio for diagnosing a low PMI. The area under the curve was 0.593 and 0.699, respectively. The cut-off value with maximum accuracy for TSH concentrations was 1.491 μIU/mL, sensitivity was 56.1%, and specificity was 80.0%. Corresponding values for the FT3/FT4 ratio were 1.723, 78.0, and 66.7%, respectively.
Conclusion
TSH concentrations and the FT3/FT4 ratio are correlated with the PMI, and their thresholds may help prevent muscle mass loss in Japanese individuals with T2DM.



Similar content being viewed by others
References
DeFronzo RA, Ferrannini E, Groop L, Henry RR, Herman WH, Holst JJ, et al. Type 2 diabetes mellitus. Nat Rev Dis Primers. 2015;1:15019. https://doi.org/10.1038/nrdp.2015.19.
Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol. 2018;14(2):88–98. https://doi.org/10.1038/nrendo.2017.151.
Umegaki H. Sarcopenia and diabetes: hyperglycemia is a risk factor for age-associated muscle mass and functional reduction. J Diabetes Investig. 2015;6(6):623–4. https://doi.org/10.1111/jdi.12365.
Stitt TN, Drujan D, Clarke BA, Panaro F, Timofeyva Y, Kline WO, et al. The IGF-1/PI3K/Akt pathway prevents expression of muscle atrophy-induced ubiquitin ligases by inhibiting FOXO transcription factors. Mol Cell. 2004;14(3):395–403. https://doi.org/10.1016/s1097-2765(04)00211-4.
Yang S, Yang G, Wu H, Kang L, Xiang J, Zheng P, et al. MicroRNA-193b impairs muscle growth in mouse models of type 2 diabetes by targeting the PDK1/Akt signalling pathway. Diabetologia. 2022;65(3):563–81. https://doi.org/10.1007/s00125-021-05616-y.
Perry BD, Caldow MK, Brennan-Speranza TC, Sbaraglia M, Jerums G, Garnham A, et al. Muscle atrophy in patients with Type 2 Diabetes Mellitus: roles of inflammatory pathways, physical activity and exercise. Exerc Immunol Rev. 2016;22:94–109.
Cherrington AD. Banting Lecture 1997. Control of glucose uptake and release by the liver in vivo. Diabetes. 1999;48(5):1198–214. https://doi.org/10.2337/diabetes.48.5.1198.
Eckardt K, Görgens SW, Raschke S, Eckel J. Myokines in insulin resistance and type 2 diabetes. Diabetologia. 2014;57(6):1087–99. https://doi.org/10.1007/s00125-014-3224-x.
Ueki H, Hara T, Okamura Y, Bando Y, Terakawa T, Furukawa J, et al. Association between sarcopenia based on psoas muscle index and the response to nivolumab in metastatic renal cell carcinoma: a retrospective study. Investig Clin Urol. 2022;63(4):415–24. https://doi.org/10.4111/icu.20220028.
Hamaguchi Y, Kaido T, Okumura S, Kobayashi A, Hammad A, Tamai Y, et al. Proposal for new diagnostic criteria for low skeletal muscle mass based on computed tomography imaging in Asian adults. Nutrition. 2016;32(11–12):1200–5. https://doi.org/10.1016/j.nut.2016.04.003.
Ito K, Ookawara S, Imai S, Kakuda H, Bandai Y, Fueki M, et al. Muscle mass evaluation using psoas muscle mass index by computed tomography imaging in hemodialysis patients. Clin Nutr ESPEN. 2021;44:410–4. https://doi.org/10.1016/j.clnesp.2021.04.029.
Yamaguchi K, Kitamura M, Takazono T, Sato S, Yamamoto K, Notomi S, et al. Association between the psoas muscle index and hospitalization for pneumonia in patients undergoing hemodialysis. BMC Nephrol. 2021;22(1):394. https://doi.org/10.1186/s12882-021-02612-7.
Murea M, Lenchik L, Register TC, Russell GB, Xu J, Smith SC, et al. Psoas and paraspinous muscle index as a predictor of mortality in African American men with type 2 diabetes mellitus. J Diabetes Complic. 2018;32(6):558–64. https://doi.org/10.1016/j.jdiacomp.2018.03.004.
Tucker BM, Hsu FC, Register TC, Xu J, Smith SC, Murea M, et al. Psoas and paraspinous muscle measurements on computed tomography predict mortality in European Americans with type 2 diabetes mellitus. J Frailty Aging. 2019;8(2):72–8. https://doi.org/10.14283/jfa.2019.5.
Li S, Yu H, Zhang P, Tu Y, Xiao Y, Yang D, et al. The Nonlinear relationship between psoas cross-sectional area and BMI: A new observation and its insights into diabetes remission after roux-en-Y gastric bypass. Diabetes Care. 2021;44(12):2783–6. https://doi.org/10.2337/dc20-2907.
Lu CQ, Wang YC, Meng XP, Zhao HT, Zeng CH, Xu W, et al. Diabetes risk assessment with imaging: a radiomics study of abdominal CT. Eur Radiol. 2019;29(5):2233–42. https://doi.org/10.1007/s00330-018-5865-5.
Kalyani RR, Corriere M, Ferrucci L. Age-related and disease-related muscle loss: the effect of diabetes, obesity, and other diseases. Lancet Diabetes Endocrinol. 2014;2(10):819–29. https://doi.org/10.1016/S2213-8587(14)70034-8.
Monaco CMF, Perry CGR, Hawke TJ. Diabetic myopathy: current molecular understanding of this novel neuromuscular disorder. Curr Opin Neurol. 2017;30(5):545–52. https://doi.org/10.1097/WCO.0000000000000479.
Park SW, Goodpaster BH, Strotmeyer ES, Kuller LH, Broudeau R, Kammerer C, et al. Accelerated loss of skeletal muscle strength in older adults with type 2 diabetes: the health, aging, and body composition study. Diabetes Care. 2007;30(6):1507–12. https://doi.org/10.2337/dc06-2537.
Park SW, Goodpaster BH, Lee JS, Kuller LH, Boudreau R, de Rekeneire N, et al. Excessive loss of skeletal muscle mass in older adults with type 2 diabetes. Diabetes Care. 2009;32(11):1993–7. https://doi.org/10.2337/dc09-0264.
Andersen H, Gjerstad MD, Jakobsen J. Atrophy of foot muscles: a measure of diabetic neuropathy. Diabetes Care. 2004;27(10):2382–5. https://doi.org/10.2337/diacare.27.10.2382.
Andersen H, Gadeberg PC, Brock B, Jakobsen J. Muscular atrophy in diabetic neuropathy: a stereological magnetic resonance imaging study. Diabetologia. 1997;40(9):1062–9. https://doi.org/10.1007/s001250050788.
Yagihashi S, Yamagishi S, Wada R. Pathology and pathogenetic mechanisms of diabetic neuropathy: correlation with clinical signs and symptoms. Diabetes Res Clin Pract. 2007;77(Suppl 1):S184–9. https://doi.org/10.1016/j.diabres.2007.01.054.
Funamizu T, Nagatomo Y, Saji M, Iguchi N, Daida H, Yoshikawa T. Low muscle mass assessed by psoas muscle area is associated with clinical adverse events in elderly patients with heart failure. PLoS ONE. 2021;16(2): e0247140. https://doi.org/10.1371/journal.pone.0247140.
Ozeki N, Kawaguchi K, Fukui T, Nakamura S, Hakiri S, Mori S, et al. Psoas muscle mass in patients undergoing lung cancer surgery: a prognostic difference between squamous cell carcinoma and adenocarcinoma. Int J Clin Oncol. 2020;25(5):876–84. https://doi.org/10.1007/s10147-020-01624-x.
Sinaki M, McPhee MC, Hodgson SF, Merritt JM, Offord KP. Relationship between bone mineral density of spine and strength of back extensors in healthy postmenopausal women. Mayo Clin Proc. 1986;61(2):116–22. https://doi.org/10.1016/s0025-6196(12)65197-0.
Reginster JY, Beaudart C, Buckinx F, Bruyère O. Osteoporosis and sarcopenia: two diseases or one? Curr Opin Clin Nutr Metab Care. 2016;19(1):31–6. https://doi.org/10.1097/MCO.0000000000000230.
Pan Y, Xu J. Association between muscle mass, bone mineral density and osteoporosis in type 2 diabetes. J Diabetes Investig. 2022;13(2):351–8. https://doi.org/10.1111/jdi.13642.
Tagliaferri C, Wittrant Y, Davicco MJ, Walrand S, Coxam V. Muscle and bone, two interconnected tissues. Ageing Res Rev. 2015;21:55–70. https://doi.org/10.1016/j.arr.2015.03.002.
Han Y, Cowin SC, Schaffler MB, Weinbaum S. Mechanotransduction and strain amplification in osteocyte cell processes. Proc Natl Acad Sci USA. 2004;101(47):16689–94. https://doi.org/10.1073/pnas.0407429101.
Srikanthan P, Hevener AL, Karlamangla AS. Sarcopenia exacerbates obesity-associated insulin resistance and dysglycemia: findings from the national health and nutrition examination survey III. PLoS ONE. 2010;5(5): e10805. https://doi.org/10.1371/journal.pone.0010805.
Landi F, Cruz-Jentoft AJ, Liperoti R, Russo A, Giovannini S, Tosato M, et al. Sarcopenia and mortality risk in frail older persons aged 80 years and older: results from ilSIRENTE study. Age Ageing. 2013;42(2):203–9. https://doi.org/10.1093/ageing/afs194.
Kwak JH, Jun DW, Lee SM, Cho YK, Lee KN, Lee HL, et al. Lifestyle predictors of obese and non-obese patients with nonalcoholic fatty liver disease: a cross-sectional study. Clin Nutr. 2018;37(5):1550–7. https://doi.org/10.1016/j.clnu.2017.08.018.
Hayashi Y. Glutaminostatin: another facet of glucagon as a regulator of plasma amino acid concentrations. J Diabetes Investig. 2019;10(6):1391–3. https://doi.org/10.1111/jdi.13110.
Watanabe C, Seino Y, Miyahira H, Yamamoto M, Fukami A, Ozaki N, et al. Remodeling of hepatic metabolism and hyperaminoacidemia in mice deficient in proglucagon-derived peptides. Diabetes. 2012;61(1):74–84. https://doi.org/10.2337/db11-0739.
Ueno S, Seino Y, Hidaka S, Maekawa R, Takano Y, Yamamoto M, et al. High protein diet feeding aggravates hyperaminoacidemia in mice deficient in proglucagon-derived peptides. Nutrients. 2022;14(5):975. https://doi.org/10.3390/nu14050975.
Verlaan S, Aspray TJ, Bauer JM, Cederholm T, Hemsworth J, Hill TR, et al. Nutritional status, body composition, and quality of life in community-dwelling sarcopenic and non-sarcopenic older adults: a case-control study. Clin Nutr. 2017;36(1):267–74. https://doi.org/10.1016/j.clnu.2015.11.013.
Ter Borg S, de Groot LC, Mijnarends DM, de Vries JH, Verlaan S, Meijboom S, et al. Differences in nutrient intake and biochemical nutrient status between sarcopenic and nonsarcopenic older adults-results from the maastricht sarcopenia study. J Am Med Dir Assoc. 2016;17(5):393–401. https://doi.org/10.1016/j.jamda.2015.12.015.
Waters DL, Wayne SJ, Andrieu S, Cesari M, Villareal DT, Garry P, et al. Sexually dimorphic patterns of nutritional intake and eating behaviors in community-dwelling older adults with normal and slow gait speed. J Nutr Health Aging. 2014;18(3):228–33. https://doi.org/10.1007/s12603-014-0004-8.
Brancaccio P, Lippi G, Maffulli N. Biochemical markers of muscular damage. Clin Chem Lab Med. 2010;48(6):757–67. https://doi.org/10.1515/CCLM.2010.179.
Liu J, Yu D, Xu M, Feng R, Sun Y, Yin X, et al. β-Cell function is associated with osteosarcopenia in middle-aged and older nonobese patients with type 2 diabetes: a cross-sectional study. Open Med (Wars). 2021;16(1):1583–90. https://doi.org/10.1515/med-2021-0376.
Tanaka K, Kanazawa I, Sugimoto T. Reduction in endogenous insulin secretion is a risk factor of sarcopenia in men with type 2 diabetes mellitus. Calcif Tissue Int. 2015;97(4):385–90. https://doi.org/10.1007/s00223-015-9990-8.
Sakai S, Tanimoto K, Imbe A, Inaba Y, Shishikura K, Tanimoto Y, et al. Decreased β-cell function is associated with reduced skeletal muscle mass in Japanese subjects without diabetes. PLoS ONE. 2016;11(9): e0162603. https://doi.org/10.1371/journal.pone.0162603.
Shishikura K, Tanimoto K, Sakai S, Tanimoto Y, Terasaki J, Hanafusa T. Association between skeletal muscle mass and insulin secretion in patients with type 2 diabetes mellitus. Endocr J. 2014;61(3):281–7. https://doi.org/10.1507/endocrj.ej13-0375.
Chung YH, Park KS, Lee KU, Kim SY, Lee HK, Min HK. High 24-hour urinary C-peptide excretion in non-insulin dependent diabetes mellitus. Korean J Intern Med. 1986;1(2):172–7. https://doi.org/10.3904/kjim.1986.1.2.172.
Mullur R, Liu YY, Brent GA. Thyroid hormone regulation of metabolism. Physiol Rev. 2014;94(2):355–82. https://doi.org/10.1152/physrev.00030.2013.
Larsen PR. Thyroidal triiodothyronine and thyroxine in Graves’ disease: correlation with presurgical treatment, thyroid status, and iodine content. J Clin Endocrinol Metab. 1975;41(06):1098–104. https://doi.org/10.1210/jcem-41-6-1098.
Citterio CE, Veluswamy B, Morgan SJ, Galton VA, Banga JP, Atkins S, et al. Triiodothyronine formation from thyrocytes activated by thyroid-stimulating hormone. J Biol Chem. 2017;292(37):15434–44. https://doi.org/10.1074/jbc.M117.784447.
Razvi S, Weaver JU, Pearce SH. Subclinical thyroid disorders: significance and clinical impact. J Clin Pathol. 2010;63(5):379–86. https://doi.org/10.1136/jcp.2008.057414.
Biondi B, Cooper DS. The clinical significance of subclinical thyroid dysfunction. Endocr Rev. 2008;29(1):76–131. https://doi.org/10.1210/er.2006-0043.
de Lloyd A, Bursell J, Gregory JW, Rees DA, Ludgate M. TSH receptor activation and body composition. J Endocrinol. 2010;204(1):13–20. https://doi.org/10.1677/JOE-09-0262.
Brennan MD, Powell C, Kaufman KR, Sun PC, Bahn RS, Nair KS. The impact of overt and subclinical hyperthyroidism on skeletal muscle. Thyroid. 2006;16(4):375–80. https://doi.org/10.1089/thy.2006.16.375.
Ohn JH, Han SK, Park DJ, Park KS, Park YJ. Expression of thyroid stimulating hormone receptor mRNA in mouse C2C12 skeletal muscle cells. Endocrinol Metab (Seoul). 2013;28(2):119–24. https://doi.org/10.3803/EnM.2013.28.2.119.
Moon MK, Kang GH, Kim HH, Han SK, Koo YD, Cho SW, et al. Thyroid-stimulating hormone improves insulin sensitivity in skeletal muscle cells via cAMP/PKA/CREB pathway-dependent upregulation of insulin receptor substrate-1 expression. Mol Cell Endocrinol. 2016;436:50–8. https://doi.org/10.1016/j.mce.2016.07.018.
Boschi A, Daumerie C, Spiritus M, Beguin C, Senou M, Yuksel D, et al. Quantification of cells expressing the thyrotropin receptor in extraocular muscles in thyroid associated orbitopathy. Br J Ophthalmol. 2005;89(6):724–9. https://doi.org/10.1136/bjo.2004.050807.
Acknowledgements
We thank the staff of the Division of Diabetes for collecting the clinical data, and Masato Yamauchi for guiding us in measuring the area of the psoas muscles by CT images. We thank Ellen Knapp, PhD, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by EA-H, YM, and TH. The first draft of the manuscript was written by EA-H, YM, and TH and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Hideki Kamiya received lecture fees from Novo Nordisk Pharma, Sanofi, Sumitomo Pharma, Nippon Boehringer Ingelheim, Eli Lilly Japan, Daiichi Sankyo, Ono Pharmaceutical, Kissei Pharmaceutical, Mitsubishi Tanabe Pharma, Kowa, Novartis Pharma, MSD, and Sanwa Kagaku Kenkyusho. Jiro Nakamura received lecture fees from MSD, Novo Nordisk Pharma, Sanofi, Daiichi Sankyo, Ono Pharmaceutical, Novartis Pharma, Taisho Pharmaceutical, Takeda Pharmaceutical, and Terumo. Hideki Kamiya and Jiro Nakamura received research funding from Eli Lilly Japan, Ono Pharmaceutical, and Kissei Pharmaceutical. Hideki Kamiya and Jiro Nakamura received subsidies or donations from MSD, Ono Pharmaceutical, Sumitomo, Pharma, Takeda Pharmaceutical, Mitsubishi Tanabe Pharma, Japan Tobacco, Novo Nordisk Pharma, and Taisho Pharmaceutical. Hideki Kamiya and Jiro Nakamura received endowed departments by commercial entities from Ono Pharmaceutical, Abbott Japan, Sanwa Kagaku Kenkyusho, Kowa, and Terumo. The remaining authors (E Asano-Hayami, Yoshiaki Morishita, T Hayami, Y Shibata, T Kiyose, S Sasajima, Y Hayashi, M Motegi, M Kato, S Asano, H Nakai-Shimoda, Y Yamada, E Miura-Yura, T Himeno, M Kondo, S Tsunekawa, and Y Kato) declare that they have no conflict of interest.
Ethical approval
This study has been approved by the Institutional Review Board of Aichi Medical University (approval number: 2019–133, approval date: 01/10/2020). This study was conducted in compliance with the ethical principles of the Declaration of Helsinki. Informed consent was obtained by the opt-out methods on the website of Aichi Medical University Hospital (https://www.aichi-med-u.ac.jp/hospital/files/byoin/rinH_2019-149.pdf).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Asano-Hayami, E., Morishita, Y., Hayami, T. et al. Clinical parameters correlated with the psoas muscle index in Japanese individuals with type 2 diabetes mellitus. Diabetol Int 14, 76–85 (2023). https://doi.org/10.1007/s13340-022-00602-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13340-022-00602-0