Abstract
Aim
Diabetes mellitus is a well-known risk factor for onset and progression of periodontal disease. However, the continuous relationship between glycemic control and the number of natural teeth has not been well characterized in large-scale studies. We aimed to determine whether the glycated hemoglobin A1c (HbA1c) level and fasting plasma glucose (FPG) are associated with the number of natural teeth.
Methods
A cross-sectional study: A database comprising employment-based health insurance claim and medical check-up data from 706,150 participants between April 2015 and March 2016 in Japan. The exclusion criteria included missing data regarding dental receipts, number of natural teeth, HbA1c, smoking status, and age < 20 years. Ultimately, 233,567 individuals were analyzed. The participants were allocated to five groups according to their HbA1c and three groups according to their FPG, and then the number of natural teeth were compared.
Results
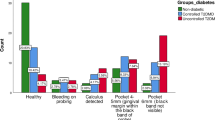
Higher HbA1c was associated with fewer teeth in participants ≥ 30 years of age (P for trend < 0.001). Higher FPG was associated with fewer teeth between 30 and 69 years of age (P for trend < 0.001). Participants with impaired fasting glucose was already at risk for fewer teeth between 40 and 69 years of age than those with normal FPG.
Conclusions
Glycemic control is strongly associated with the number of natural teeth in the real-world setting. Furthermore, there are continuous relationships of HbA1c and FPG with number of natural teeth including individual with impaired fasting glucose. These data emphasize the importance of glycemic control and appropriate oral care for the protection against tooth loss.



Similar content being viewed by others
References
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9. Diabetes Res Clin Pract. 2019;157: 107843. https://doi.org/10.1016/j.diabres.2019.107843.
Nowjack-Raymer RE, Sheiham A. Numbers of natural teeth, diet, and nutritional status in US adults. J Dent Res. 2007;86(12):1171–5. https://doi.org/10.1177/154405910708601206.
Hiratsuka T, Komiyama T, Ohi T, Tanji F, Tomata Y, Tsuji I, et al. Contribution of systemic inflammation and nutritional status to the relationship between tooth loss and mortality in a community-dwelling older Japanese population: a mediation analysis of data from the Tsurugaya project. Clin Oral Investig. 2019. https://doi.org/10.1007/s00784-019-03072-y.
Gu Y, Wu W, Bai J, Chen X, Yu L, Zhang Q, et al. Association between the number of teeth and frailty among Chinese older adults: a nationwide cross-sectional study. BMJ Open. 2019;9(10): e029929. https://doi.org/10.1136/bmjopen-2019-029929.
Petrovsky DV, Wu B, Mao W, Dong X. Oral health symptoms and cognitive function among us community-dwelling chinese older adults. J Am Geriatr Soc. 2019;67(S3):S532–7. https://doi.org/10.1111/jgs.15748.
Koka S, Gupta A. Association between missing tooth count and mortality: a systematic review. J Prosthodont Res. 2018;62(2):134–51. https://doi.org/10.1016/j.jpor.2017.08.003.
Huang DL, Chan KC, Young BA. Poor oral health and quality of life in older US adults with diabetes mellitus. J Am Geriatr Soc. 2013;61(10):1782–8. https://doi.org/10.1111/jgs.12452.
Hobdell M, Petersen PE, Clarkson J, Johnson N. Global goals for oral health 2020. Int Dent J. 2003;53(5):285–8. https://doi.org/10.1111/j.1875-595x.2003.tb00761.x.
Eklund SA, Burt BA. Risk factors for total tooth loss in the United States; longitudinal analysis of national data. J Public Health Dent. 1994;54(1):5–14. https://doi.org/10.1111/j.1752-7325.1994.tb01173.x.
Nelson RG, Shlossman M, Budding LM, Pettitt DJ, Saad MF, Genco RJ, et al. Periodontal disease and NIDDM in Pima Indians. Diabetes Care. 1990;13(8):836–40. https://doi.org/10.2337/diacare.13.8.836.
Lalla E, Papapanou PN. Diabetes mellitus and periodontitis: a tale of two common interrelated diseases. Nat Rev Endocrinol. 2011;7(12):738–48. https://doi.org/10.1038/nrendo.2011.106.
Hintao J, Teanpaisan R, Chongsuvivatwong V, Dahlen G, Rattarasarn C. Root surface and coronal caries in adults with type 2 diabetes mellitus. Community Dent Oral Epidemiol. 2007;35(4):302–9. https://doi.org/10.1111/j.1600-0528.2007.00325.x.
Sandberg GE, Sundberg HE, Fjellstrom CA, Wikblad KF. Type 2 diabetes and oral health: a comparison between diabetic and non-diabetic subjects. Diabetes Res Clin Pract. 2000;50(1):27–34. https://doi.org/10.1016/s0168-8227(00)00159-5.
Suzuki S, Yoshino K, Takayanagi A, Ishizuka Y, Satou R, Nara N, et al. Relationship between blood HbA1c level and decayed teeth in patients with type 2 diabetes: a cross-sectional study. Bull Tokyo Dent Coll. 2019;60(2):89–96. https://doi.org/10.2209/tdcpublication.2018-0039.
Shima D, Ii Y, Yamamoto Y, Nagayasu S, Ikeda Y, Fujimoto Y. A retrospective, cross-sectional study of real-world values of cardiovascular risk factors using a healthcare database in Japan. BMC Cardiovasc Disord. 2014;14:120. https://doi.org/10.1186/1471-2261-14-120.
Yuasa A, Murata T, Imai K, Yamamoto Y, Fujimoto Y. Treatment procedures and associated medical costs of methicillin-resistant. SAGE Open Med. 2019;7:2050312119871181. https://doi.org/10.1177/2050312119871181.
Murata T, Arai K, Kashiwagi K, Baba S. Relationship between the number of occlusal supporting and medical cost: analysis using large claims database from employee health care insurance in Japan. J Health Econ Outcomes Res. 2020;7(1):1–9. https://doi.org/10.36469/001c.11594.
Tsuneishi M, Yamamoto T, Yamaguchi T, Kodama T, Sato T. Association between number of teeth and Alzheimer’s disease using the National Database of Health Insurance Claims and Specific Health Checkups of Japan. PLoS ONE. 2021;16(4): e0251056. https://doi.org/10.1371/journal.pone.0251056.
Kobayashi D, Kuriyama N, Hirano K, Takahashi O, Noto H. Malignancy incidences by glycemic control among diabetic patients. Endocr Connect. 2018;7(12):1457–63. https://doi.org/10.1530/EC-18-0355.
Organization. WH. Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycemia: Report of a WHO/IDF Consultation. Geneva: World Health Org.
Japanese Ministry of Health LaW: Statistical Tables of the Survey of Dental Diseases 2016. https://www.mhlw.go.jp/toukei/list/xls/62-17c28-1.xls. (September 2017). Accessed December 27 2019.
Luo H, Pan W, Sloan F, Feinglos M, Wu B. Forty-year trends in tooth loss among american adults with and without diabetes mellitus: an age-period-cohort analysis. Prev Chronic Dis. 2015;12:E211. https://doi.org/10.5888/pcd12.150309.
Patel MH, Kumar JV, Moss ME. Diabetes and tooth loss: an analysis of data from the National Health and Nutrition Examination Survey, 2003–2004. J Am Dent Assoc. 2013;144(5):478–85. https://doi.org/10.14219/jada.archive.2013.0149.
Demmer RT, Holtfreter B, Desvarieux M, Jacobs DR, Kerner W, Nauck M, et al. The influence of type 1 and type 2 diabetes on periodontal disease progression: prospective results from the Study of Health in Pomerania (SHIP). Diabetes Care. 2012;35(10):2036–42. https://doi.org/10.2337/dc11-2453.
Costa FO, Miranda Cota LO, Pereira Lages EJ, Soares Dutra Oliveira AM, Dutra Oliveira PA, Cyrino RM, et al. Progression of periodontitis and tooth loss associated with glycemic control in individuals undergoing periodontal maintenance therapy: a 5-year follow-up study. J Periodontol. 2013;84(5):595–605. https://doi.org/10.1902/jop.2012.120255.
Jung YS, Shin MH, Kweon SS, Lee YH, Kim OJ, Kim YJ, et al. Periodontal disease associated with blood glucose levels in urban Koreans aged 50 years and older: the Dong-gu study. Gerodontology. 2015;32(4):267–73. https://doi.org/10.1111/ger.12107.
Katagiri S, Nitta H, Nagasawa T, Izumi Y, Kanazawa M, Matsuo A, et al. Effect of glycemic control on periodontitis in type 2 diabetic patients with periodontal disease. J Diabetes Investig. 2013;4(3):320–5. https://doi.org/10.1111/jdi.12026.
D’Aiuto F, Gkranias N, Bhowruth D, Khan T, Orlandi M, Suvan J, et al. Systemic effects of periodontitis treatment in patients with type 2 diabetes: a 12 month, single-centre, investigator-masked, randomised trial. Lancet Diabetes Endocrinol. 2018;6(12):954–65. https://doi.org/10.1016/S2213-8587(18)30038-X.
Similä T, Auvinen J, Puukka K, Keinänen-Kiukaanniemi S, Virtanen JI. Impaired glucose metabolism is associated with tooth loss in middle-aged adults: the Northern Finland Birth Cohort Study 1966. Diabetes Res Clin Pract. 2018;142:110–9. https://doi.org/10.1016/j.diabres.2018.05.035.
Yoshihara A, Watanabe R, Nishimuta M, Hanada N, Miyazaki H. The relationship between dietary intake and the number of teeth in elderly Japanese subjects. Gerodontology. 2005;22(4):211–8. https://doi.org/10.1111/j.1741-2358.2005.00083.x.
Choi SE, Sima C, Pandya A. Impact of treating oral disease on preventing vascular diseases: a model-based cost-effectiveness analysis of periodontal treatment among patients with Type 2 diabetes. Diabetes Care. 2019. https://doi.org/10.2337/dc19-1201.
Albandar JM, Streckfus CF, Adesanya MR, Winn DM. Cigar, pipe, and cigarette smoking as risk factors for periodontal disease and tooth loss. J Periodontol. 2000;71(12):1874–81. https://doi.org/10.1902/jop.2000.71.12.1874.
Jepsen S, Caton JG, Albandar JM, Bissada NF, Bouchard P, Cortellini P, et al. Periodontal manifestations of systemic diseases and developmental and acquired conditions: consensus report of workgroup 3 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Clin Periodontol. 2018;45(Suppl 20):S219–29. https://doi.org/10.1111/jcpe.12951.
Souto MLS, Rovai ES, Villar CC, Braga MM, Pannuti CM. Effect of smoking cessation on tooth loss: a systematic review with meta-analysis. BMC Oral Health. 2019;19(1):245. https://doi.org/10.1186/s12903-019-0930-2.
Saito M, Shimazaki Y, Fukai K, Furuta M, Aida J, Ando Y, et al. Risk factors for tooth loss in adult Japanese dental patients: 8020 Promotion Foundation Study. J Investig Clin Dent. 2019;10(2): e12392. https://doi.org/10.1111/jicd.12392.
Japanese Ministry of Health LaW: The National Health and Nutrition Survey in Japan, 2015. (in Japanese). https://www.mhlw.go.jp/bunya/kenkou/eiyou/h27-houkoku.html (2015). Accessed July 6 2021.
Acknowledgements
The authors thank Dr. Satoshi Shizukuishi, and Dr. Midori Tsuneishi for their expert technical assistance. We also thank Mark Cleasby, PhD from Edanz Group (https://en-author-services.edanzgroup.com/ac) for editing the English text of drafts of this manuscript.
Funding
This work was funded by Sunstar Inc, Japan.
Author information
Authors and Affiliations
Contributions
KH and KM conceived and designed the study. KM takes responsibility for the integrity of the data and the accuracy of the data analysis. KH, MI, IM and TY performed the statistical analysis. HM and AI supervised the study. All authors reviewed, edited, and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
KH, MI, TY, MH and AI are employees of Sunstar Inc. The authors participated in the preparation, analysis and interpretation of the data. HM received research support unrelated to this study from Astellas Pharma Inc., AstraZeneca K.K., Bayer, Daiichi Sankyo, Eli Lilly Japan, Kowa Pharmaceutical, Kyowa Hakko Kirin, Miki Corporation, Mitsubishi Tanabe Pharma, MSD, Nippon Boehringer Ingelheim, Nipro, Nissan Chemical Corporation, Novartis, Novo Nordisk Pharma, Ono Pharmaceutical, Sanofi, Sumitomo Dainippon Pharma, Taisho Toyama Pharmaceutical, Takeda Pharmaceutical, Sanwa Chemical, Shionogi and Teijin Pharma; and lecture fees and fees for serving on advisory boards from AstraZeneca K.K., Daiichi Sankyo, Eli Lilly Japan, Mitsubishi Tanabe Pharma, MSD, Nippon Boehringer Ingelheim, Novo Nordisk Pharma, Sanofi, Sumitomo Dainippon Pharma and Takeda Pharmaceutical. KM received grants from Astellas, AstraZeneca, Ono Pharmaceutics and Sanwa Kagaku Kenkyusho that were unrelated to this study. No other potential conflicts of interest relevant to this study are declared.
Ethics approval
As secondary database we used for research purposes contained anonymized data only, this article does not contain any studies with human or animal subjects performed by any of the authors. Patient informed consent was not required, because it is impossible to link the identifiers with external information.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Harada, K., Morino, K., Ishikawa, M. et al. Glycemic control and number of natural teeth: analysis of cross-sectional Japanese employment-based dental insurance claims and medical check-up data. Diabetol Int 13, 244–252 (2022). https://doi.org/10.1007/s13340-021-00533-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13340-021-00533-2