Abstract
Aim
Diabetes and aging are both well-established risk factors for insomnia. Therefore, we investigated the changes in subjective sleep quality in relation to clinical backgrounds and age in patients with type 2 diabetes mellitus (T2DM).
Methods
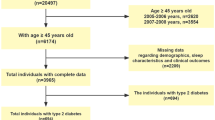
This cross-sectional study included 380 participants with T2DM who were between 18 and 79 years of age from our outpatient clinics. Individuals with any symptoms and medical histories associated with obstructive sleep apnea (OSA) were excluded from the interview and analyses. Data were collected using self-administered questionnaires, namely the Pittsburgh Sleep Quality Index (PSQI) and the Morning-Evening Questionnaire (MEQ), as well as medical records and blood samples. We performed stratified analyses according to age decades.
Results
The number of patients in the age groups (in years) was as follows: < 50 (n = 69), 50–60 (n = 52), 60–70 (n = 138), and 70–80 (n = 121). PSQI score was highest in the < 50 group (4.99 ± 2.40), and significantly decreased with age (p < 0.05). Body mass index (BMI) was also highest in the < 50 group (25.5 ± 4.8 kg/m2), and markedly decreased with age (p < 0.01). Interestingly, BMI was significantly correlated with the PSQI score (rs = 0.157, p < 0.05). We also found that younger patients had shorter sleep duration, stronger daytime sleepiness, and a tendency for the evening type.
Conclusion
Younger T2DM patients had poorer sleep quality and higher BMI. Our findings suggest that insomnia should be accounted for as a potential comorbidity when examining or treating patients with T2DM and obesity even in the younger population.



Similar content being viewed by others

References
Matsumoto T, Murase K, Tabara Y, Gozal D, Smith D, Minami T, Tachikawa R, Tanizawa K, Oga T, Nagashima S, Wakamura T, Komenami N, Setoh K, Kawaguchi T, Tsutsumi T, Takahashi Y, Nakayama T, Hirai T, Matsuda F, Chin K. Impact of sleep characteristics and obesity on diabetes and hypertension across genders and menopausal status: the Nagahama study. Sleep. 2018. https://doi.org/10.1093/sleep/zsy071.
Ministry of Health Labour and Welfare. Summary results of the national health and nutrition survey Japan; 2018. https://www.mhlw.go.jp/content/10900000/000688863.pdf. (Accessed 8 May 2021).
Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262:1479–84.
Knutson KL, Ryden AM, Mander BA, Van Cauter E. Role of sleep duration and quality in the risk and severity of type 2 diabetes mellitus. Arch Intern Med. 2006;166:1768–74.
Yoda K, Inaba M, Hamamoto K, Yoda M, Tsuda A, Mori K, Imanishi Y, Emoto M, Yamada S. Association between poor glycemic control, impaired sleep quality, and increased arterial thickening in type 2 diabetic patients. PLoS ONE. 2015;10:e0122521.
Leproult R, Deliens G, Gilson M, Peigneux P. Beneficial impact of sleep extension on fasting insulin sensitivity in adults with habitual sleep restriction. Sleep. 2015;38:707–15.
Bruehl H, Rueger M, Dziobek I, Sweat V, Tirsi A, Javier E, Arentoft A, Wolf OT, Convit A. Hypothalamic-pituitary-adrenal axis dysregulation and memory impairments in type 2 diabetes. J Clin Endocrinol Metab. 2007;92:2439–45.
Vgontzas AN, Chrousos GP. Sleep, the hypothalamic-pituitary-adrenal axis, and cytokines: multiple interactions and disturbances in sleep disorders. Endocrinol Metab Clin North Am. 2002;31:15–36.
Pallayova M, Donic V, Gresova S, Peregrim I, Tomori Z. Do differences in sleep architecture exist between persons with type 2 diabetes and nondiabetic controls? J Diabetes Sci Technol. 2010;4:344–52.
Haba-Rubio J, Marques-Vidal P, Andries D, Tobback N, Preisig M, Vollenweider P, Waeber G, Luca G, Tafti M, Heinzer R. Objective sleep structure and cardiovascular risk factors in the general population: the HypnoLaus Study. Sleep. 2015;38:391–400.
Sridhar GR, Madhu K. Prevalence of sleep disturbances in diabetes mellitus. Diabetes Res Clin Pract. 1994;23:183–6.
Van Cauter E, Leproult R, Plat L. Age-related changes in slow wave sleep and REM sleep and relationship with growth hormone and cortisol levels in healthy men. JAMA. 2000;284:861–8.
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213.
Bastien CH, Vallières A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307.
Antúnez JM. Circadian typology is related to emotion regulation, metacognitive beliefs and assertiveness in healthy adults. PLoS ONE. 2020;15:e0230169.
Kim K, Uchiyama M, Okawa M, Liu X, Ogihara R. An epidemiological study of insomnia among the Japanese general population. Sleep. 2000;23:41–7.
Tasali E, Leproult R, Ehrmann DA, Van Cauter E. Slow-wave sleep and the risk of type 2 diabetes in humans. Proc Natl Acad Sci USA. 2008;105:1044–9.
Boffetta P, McLerran D, Chen Y, Inoue M, Sinha R, He J, Gupta PC, Tsugane S, Irie F, Tamakoshi A, Gao Y-T, Shu X-O, Wang R, Tsuji I, Kuriyama S, Matsuo K, Satoh H, Chen C-J, Yuan J-M, Yoo K-Y, Ahsan H, Pan W-H, Gu D, Pednekar MS, Sasazuki S, Sairenchi T, Yang G, Xiang Y-B, Nagai M, Tanaka H, Nishino Y, You S-L, Koh W-P, Park SK, Shen C-Y, Thornquist M, Kang D, Rolland B, Feng Z, Zheng W, Potter JD. Body mass index and diabetes in Asia: a cross-sectional pooled analysis of 900000 individuals in the Asia cohort consortium. PLoS ONE. 2011;6:e19930.
Someya Y, Tamura Y, Kohmura Y, Aoki K, Kawai S, Daida H, Naito H. A body mass index over 22 kg/m2 at college age is a risk factor for future diabetes in Japanese men. PLoS ONE. 2019;14:e0211067.
Sasai H, Sairenchi T, Iso H, Irie F, Otaka E, Tanaka K, Ota H, Muto T. Relationship between obesity and incident diabetes in middle-aged and older Japanese adults: the Ibaraki Prefectural Health Study. Mayo Clin Proc. 2010;85:36–40.
Higurashi N, Kikuchi M, Miyazaki S, Itasaka Y. Comparison of Ricketts analysis and downs-Northwestern analysis for the evaluation of obstructive sleep apnea cephalograms. Psychiatry Clin Neurosci. 2001;55:259–60.
Feher M, Hinton W, Munro N, de Lusignan S. Obstructive sleep apnoea in type 2 diabetes mellitus: increased risk for overweight as well as obese people included in a national primary care database analysis. Diabet Med. 2019;36:1304–11.
Aurora RN, Punjabi NM. Obstructive sleep apnoea and type 2 diabetes mellitus: a bidirectional association. Lancet Respir Med. 2013;1:329–38.
Cizza G, Piaggi P, Lucassen EA, de Jonge L, Walter M, Mattingly MS, Kalish H, Csako G, Rother KI, Sleep Extension Study Group. Obstructive sleep apnea is a predictor of abnormal glucose metabolism in chronically sleep deprived obese adults. PLoS ONE. 2013;8:e65400.
Cedernaes J, Schiöth HB, Benedict C. Determinants of shortened, disrupted, and mistimed sleep and associated metabolic health consequences in healthy humans. Diabetes. 2015;64:1073–80.
Ford ES, Li C, Wheaton AG, Chapman DP, Perry GS, Croft JB. Sleep duration and body mass index and waist circumference among US adults. Obesity (Silver Spring). 2014;22:598–607.
Acknowledgements
We would like to thank Shuki Usui, Hiroshi Yoshino, and Ken Kanazawa, as well as all the staff of the outpatient clinic for their help in collecting data for this study. We also thank Editage (www.editage.com) for English language editing.
Funding
This work was supported by JSPS KAKENHI, Grant Number 18K07481.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
T. Hirose received research funds from Nippon Boehringer Ingelheim Co., Ltd., AstraZeneca K.K., Mitsubishi Tanabe Pharma Corporation, Novo Nordisk Pharma Ltd.; and received lecture fees from Sanofi K.K., Eli Lilly Japan K.K., Novo Nordisk Pharma Ltd., Takeda Pharmaceutical Company Limited, MSD K.K., Sumitomo Dainippon Pharma Co., Ltd., Nippon Boehringer Ingelheim Co., Ltd., Ono Pharmaceutical Co., Ltd., AstraZeneca K.K., Mitsubishi Tanabe Pharma Corporation, Kowa Company, Limited, Kissei Pharmaceutical Co., Ltd. N. Kumashiro received research funds from Boehringer Ingelheim Pharmaceuticals, Inc., and lecture fees from Takeda Pharmaceutical Company Limited, Sanofi K.K., Novo Nordisk Pharma Ltd., Ono Pharmaceutical Co., Ltd., Mitsubishi Tanabe Pharma Corporation, Nippon Boehringer Ingelheim Co., Ltd. None of the funding agencies had any role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Human and animal rights
The study was approved by the Medical Ethics Committee of Toho University Omori Medical Center (Approval no. #M19093; Approval date: August 29, 2019). This study was conducted according to the Declaration of Helsinki and current legal regulations in Japan.
Informed consent
Prior to enrollment in the survey, all eligible participants were informed about this study in written form, and the answer to the questionnaire was considered consent to enrollment.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Yoshikawa, F., Kumashiro, N., Shigiyama, F. et al. Changes in subjective sleep quality in patients with type 2 diabetes who did not use Sleep agents: a cross-sectional study according to age and clinical background. Diabetol Int 13, 142–147 (2022). https://doi.org/10.1007/s13340-021-00516-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13340-021-00516-3