Abstract
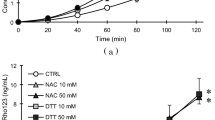
Increased intestinal permeability of macromolecules is a common feature of oxidative stress-induced gastrointestinal diseases; how it affects the absorption of drugs is not investigated. Hence, it was proposed to study the influence of hydrogen peroxide-induced oxidative stress on permeability of atenolol and metoprolol using a modified everted rat intestine technique. Atenolol was chosen as a marker of paracellular drug transport and metoprolol was selected to represent transcellular drug transport. Wistar rats were used as a source of intestine, which was everted using a glass rod, mounted on permeability apparatus, having test drug (100 μg/ml in Krebs) in donor compartment. Samples were taken from receiver compartment every 5 min for 60 min, and analyzed by HPLC. For induction of oxidative stress isolated ileum was incubated in H2O2 (200 μM) containing Krebs for 15 min and then again permeability was estimated. Extent of oxidative stress was determined by estimating lipid peroxidation using thiobarbituric acid assay, which was found to be increased by 42 % in hydrogen peroxide treated rat intestine as compared to control group. The mean apparent permeability of atenolol and metoprolol was found to be 0.054 ± 0.024 × 10−4 and 0.84 ± 0.14 × 10−4 cm/s, respectively, in control group rat intestinal segments. After exposure to hydrogen peroxide, there was a significant increase in the mean permeability of atenolol (0.11 ± 0.01 × 10−4 cm/s), however, metoprolol permeability was unaltered (0.94 ± 0.047 × 10−4 cm/s). The marked increase in the apparent permeability of atenolol may be attributed to rupture of intestinal barrier. In conclusion, the present study reports the differential effect of oxidative stress-induced damage on drug transport across rat intestine.




Similar content being viewed by others
References
Alhamoruni A, Lee AC, Wright KL, Larvin M, Sullivan EO (2010) Pharmacological effects of cannabinoids on the Caco-2 cell culture model of intestinal permeability. J Pharmacol Expt Ther 335:92–102. doi:10.1124/jpet.110.168237
Bernotti S, Seidman E, Sinnett D, Brunet S, Dionne S, Delvin E (2003) Inflammatory reaction without endogenous antioxidant response in caco-2 cells exposed to iron/ascorbate-mediated lipid peroxidation. Am J Physiol Gastrointest Liver Physiol 285:G898–G906. doi:10.1152/ajpgi.90340.2008
Brouwers J, Mols R, Augustijns P et al (2010) Validation of a differential in situ perfusion method with mesenteric blood sampling in rats for intestinal drug interaction profiling. Biopharm Drug Disp 31:278–285. doi:10.1002/bdd.710
Cani PD, Possemiers S, Van de Wiele T, Guiot Y, Everard A, Rottier O, Geurts L, Naslain D, Neyrinck A, Lambert DM, Muccioli GG, Delzenne NM (2009) Changes in gut microbiota control inflammation in obese mice through a mechanism involving GLP-2-driven improvement of gut permeability. Gut 58(8):1091–1103. doi:10.1136/gut.2008.165886
Cuzzocrea S, Mazzon E, Sarro AD, Caputi AP (2000) Role of free radicals and poly(ADP-ribose) synthetase in intestinal tight junction permeability. Mol Med 6:766–778
Darley-Usmar V, Halliwell B (1996) Blood radicals: reactive nitrogen species, reactive oxygen species, transition metal ions, and the vascular system. Pharm Res 13:649–662. doi:10.1023/A:1016079012214
Dixit PV, Jain DK, Dumbwani J (2012) Standardization of an ex vivo method for determination of intestinal permeability of drugs using everted rat intestine apparatus. J Pharmacol Toxicol Methods 65:13–17. doi:http://dx.doi.org/10.1016/j.vascn.2011.11.001
Fink MP (2003) Intestinal epithelial hyperpermeability: update on the pathogenesis of gut mucosal barrier dysfunction in critical illness. Curr Opin Crit Care 9:143–151. doi:http://dx.doi.org/10.1097/00075198-200304000-00011
Forsyth CB, Banan A, Farhadi A, Fields JZ, Tang Y, Shaikh M, Zhang LJ, Engen PA, Keshavarzian A (2007) Regulation of oxidant-induced intestinal permeability by metalloprotease-dependent epidermal growth factor receptor signaling. J Pharmacol Exp Ther 321:84–97. doi:10.1124/jpet.106.113019
Hilgendorf C, Spahn-Langguth H, Regardh CG, Lipka E, Amidon GL, Langguth P (1999) Caco-2 versus caco-2/HT29-MTX co-cultured cell lines: permeabilities via diffusion, inside- and outside-directed carrier-mediated transport. J Pharm Sci 89:63–75. doi:10.1002/(SICI)1520-6017(200001)89:1<63:AID-JPS7>3.0.CO;2-6
Jamal IS, Smith JC (1985) Effect of cadmium on glutathione peroxidase, superoxide dismutase, and lipid peroxidation in the rat heart: a possible mechanism of cadmium cardiotoxicity. Toxicol Appl Pharmacol 80:33–42. doi:10.1016/0041-008X(85)90098-5
Kelly P, Shawa T, Mwanamakondo S, Soko R, Smith G, Barclay GR, Sanderson IR (2010) Gastric and intestinal barrier impairment in tropical enteropathy and HIV: limited impact of micronutrient supplementation during a randomised controlled trial. BMC Gastroenterol 6:10–72. doi:10.1186/1471-230X-10-72
Le Ferrec E, Chesne C, Artusson P, Brayden D, Fabre G, Gires P, Guillou F, Rousset M, Rubas W, Scarino ML (2001) In vitro models of the intestinal barrier. The report and recommendations of ECVAM Workshop 46. European Centre for the Validation of Alternative methods. Altern Lab Anim 29:649–668
Leppert PS, Fix JA (1994) Use of everted intestinal rings for in vitro examination of oral absorption potential. J Pharm Sci 83:976–998. doi:10.1002/jps.2600830712
Maeda T, Miyazono Y, Ito k, Hamada K, Sekine S, Horie T (2010) Oxidative stress and enhanced paracellular permeability in the small intestinal of methotrexate-treated rats. Cancer Chemother Pharmacol 65:1117–1123. doi:10.1007/s00280-009-1119-1
Nazli A, Wang A, Steen O, Prescott D, Lu J, Perdue MH, Söderholm JD, Sherman PM, McKay DM (2006) Enterocyte cytoskeleton changes are crucial for enhanced translocation of nonpathogenic Escherichia coli across metabolically stressed gut epithelia. Infect Immun 74(192):201. doi:10.1128/IAI.74.1.192-201.2006
Neil-Dwyer G, Bartlett J, McAinsh J, Cruickshank JM (1981) β-Adrenoceptor blockers and the blood brain barrier. Br J Clin Pharm 11:549–553
Nellans HN (1991) (B) Mechanisms of peptide and protein absorption: (1) Paracellular intestinal transport: modulation of absorption. Adv Drug Deliv Rev 7:339–364. doi:10.1016/0169-409X(91)90013-3
Rao RK, Li L, Baker SS, Gupta A (2000) Glutathion peroxidation and PTPase inhibition by hydrogen peroxide in Caco-2 cell monolayer. Am J Physiol Gastrointest Liver Physiol 279:G332–G340
Shirasaka Y, Masaoka Y, Kataoka M, Sakuma S, Yamashita S (2008) Scaling of in vitro membrane permeability to predict p-glycoprotien-mediated drug absorption in vivo. Drug Metab Dispos 36:916–922. doi:10.1124/dmd.107.020040
Spahr L, Bresson-Hadni S, Amann P, Kern I, Golaz O, Frossard JL, Hadengue A (2007) Allopurinol, oxidative stress and intestinal permeability in patients with cirrhosis: an open-label pilot study. Liver Int 27:54–60. doi:10.1111/j.1478-3231.2006.01382.x
Visser JT, Lammers K, Hoogendijk A, Boer MW, Brugman S, Beijer-Liefers S, Zandvoort A, Harmsen H, Welling G, Stellaard F, Bos NA, Fasano A, Rozing J (2010) Restoration of impaired intestinal barrier function by the hydrolysed casein diet contributes to the prevention of type 1 diabetes in the diabetes-prone BioBreeding rat. Diabetologia 53:2621–2628. doi:10.1007/s00125-010-1903-9
Watanabe E, Takahashi M, Hayashi M (2004) A possibility to predict the absorbability of poorly water-soluble drugs in humans based on rat intestinal permeability assessed by an in vitro chamber method. Eur J Pharm Biopharm 58:659–665. doi:10.1016/j.ejpb.2004.03.029
Zakeri-Milani P, Valizadeh H, Tajerzadeh H, Azarmi Y, Islamboichilar Z, Barzega S, Jalali MB (2007) Predicting human intestinal permeability using single pass intestinal perfusion in rat. J Pharm Pharm Sci 10:368–379
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Dixit, P., Jain, D.K. & Rajpoot, J.S. Differential effect of oxidative stress on intestinal apparent permeability of drugs transported by paracellular and transcellular route. Eur J Drug Metab Pharmacokinet 37, 203–209 (2012). https://doi.org/10.1007/s13318-012-0099-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-012-0099-4